Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we know how important it is to tackle patent ductus arteriosus (PDA). This is a heart defect that messes with the blood flow between the pulmonary artery and the aorta.
The ductus arteriosus is a key vessel in the fetus. It usually closes after birth. But if it stays open, it can cause a machinery-like murmur, known as a heart murmur. We know how vital it is to diagnose and treat it right to avoid problems.
We’re dedicated to top-notch, caring cardiac care. Knowing about PDA and its effects is key for quick action and good management.
Key Takeaways
- Patent ductus arteriosus (PDA) is a congenital heart defect that affects normal blood flow.
- PDA can lead to a characteristic machinery-like murmur, often referred to as a heart murmur.
- Proper diagnosis and treatment are critical to avoid complications.
- Liv Hospital offers world-class, multidisciplinary cardiac care for PDA patients.
- Early intervention and effective management are vital for the best results.
Understanding Patent Ductus Arteriosus (PDA)
To tackle Patent Ductus Arteriosus (PDA), we need to know what it is and its effects. We’ll look into its definition, how common it is, and how it differs from normal fetal blood flow.
Definition and Prevalence
Patent Ductus Arteriosus (PDA) happens when the ductus arteriosus, a blood vessel, doesn’t close after birth. This vessel connects the pulmonary artery to the aorta. PDA is more common in premature infants, showing a problem with the closure process.
Normal Fetal Circulation vs. PDA
In normal fetal circulation, the ductus arteriosus is key. It lets blood bypass the lungs and go straight to the body. After birth, with the start of breathing, the ductus arteriosus closes. This change makes blood flow through the lungs for oxygen.
In PDA, this closure doesn’t happen. This leads to abnormal blood flow. Knowing this difference is key for diagnosing and treating PDA.
Research shows PDA is more common in premature babies. This is because their ductus arteriosus is not fully developed. This underdevelopment means the ductus can’t close after birth, causing PDA.
The Anatomy and Function of Ductus Arteriosus
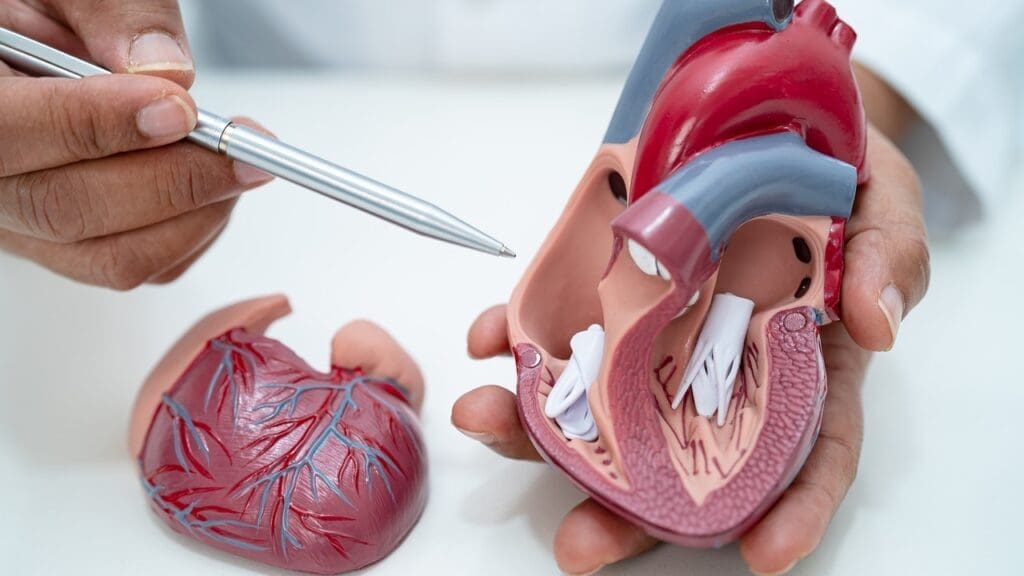
We will explore the ductus arteriosus, a vital shunt in the fetal circulation. It allows blood to bypass the lungs. This blood vessel is key for the normal development of the fetus.
Anatomy PDA: Location and Structure
The ductus arteriosus is between the pulmonary artery and the aortic arch. It’s a muscular artery that lets blood flow from the pulmonary artery to the aorta. This bypasses the lungs, ensuring oxygenated blood from the mother reaches the fetus’s body.
Purpose of Ductus Arteriosus in Fetal Development
The ductus arteriosus’s main purpose is to divert blood away from the lungs. This is vital because the fetus’s lungs are not inflated or functioning for gas exchange. It ensures oxygenated blood is delivered to the developing fetus.
Normal Closure Process After Birth
After birth, the ductus arteriosus closes as the lungs expand and start to receive blood. This closure is triggered by higher oxygen tension and lower prostaglandins. Normally, it closes within the first few days of life.
| Characteristics | Fetal Circulation | Postnatal Circulation |
|---|---|---|
| Ductus Arteriosus State | Open | Closed |
| Blood Flow Through Lungs | Minimal | Significant |
| Oxygen Tension | Low | High |
Understanding the anatomy and function of the ductus arteriosus is key. It shows its role in fetal development and the transition to postnatal circulation.
Why the Extra Blood Vessel Remains Open
The ductus arteriosus failing to close is a complex issue. It’s influenced by many factors like physiology, genetics, and environment. Knowing these factors is key to diagnosing and managing PDA.
Physiological Factors
Premature babies are more likely to have PDA. Their ductus arteriosus is not mature enough. It doesn’t get the signals to close after birth.
Risk Factors for PDA
Several factors increase the chance of PDA. These include being premature, having a low birth weight, and certain genetic conditions. Premature infants are at high risk. Their underdeveloped lungs and need for oxygen therapy can hinder ductus arteriosus closure.
Genetic Associations
Genetics also play a role in PDA. Some genetic syndromes and family patterns of PDA have been found. This suggests a possible hereditary link.
Understanding the physiological, risk, and genetic factors of PDA helps healthcare providers. They can then better diagnose and manage it. This improves outcomes for affected infants.
Classification of PDA Types
The size and shape of PDA are key in classifying it. This helps doctors decide the best treatment. We use these factors to guide our treatment choices.
Size-Based Classification
PDA size greatly affects how it’s treated. Doctors measure the PDA at its narrowest point. This size determines the treatment needed.
- Small PDA: Small PDAs might not need treatment right away but should be watched closely.
- Moderate PDA: These PDAs can cause symptoms like tiredness and trouble breathing. They might need treatment or closure.
- Large PDA: Large PDAs can cause big changes in blood flow. They need to be closed quickly to avoid problems.
Shape-Based Classification
The shape of the PDA is also important. It helps decide which closure method to use.
“The shape and size of PDA are critical factors in determining the appropriate treatment strategy.” –
Clinical Significance of Different PDA Types
Knowing the clinical importance of PDA types is key. The size and shape affect the risk of problems and the need for treatment.
Correctly classifying PDA types helps doctors create better treatment plans. This improves patient outcomes.
The Characteristic Patent Ductus Murmur
The murmur linked to Patent Ductus Arteriosus (PDA) is key for diagnosis. It sounds like a continuous “machinery” noise, a clear sign of PDA.
PDA Murmur Description: The “Machinery” Sound
The “machinery” murmur is heard all the time, loud at the left upper chest. It happens because blood keeps flowing from the aorta to the pulmonary artery through the PDA. This murmur is a clear sign of PDA.
Auscultation Techniques for Heart Murmur PDA
Doctors use a stethoscope to find the PDA murmur. They listen at the left upper chest with the patient lying down. It’s important to listen during both heart beats to hear the murmur’s continuous sound. A quiet place helps hear the murmur better.
Variations in Murmur Based on PDA Size
The size of the PDA changes the murmur’s sound. Bigger PDAs make louder sounds, while smaller ones are softer. The timing and sound of the murmur also change with the PDA’s size and the pressure difference between the aorta and pulmonary artery.
In summary, the PDA murmur is a key sign for doctors. Knowing how it sounds and using the right listening techniques helps make a correct diagnosis.
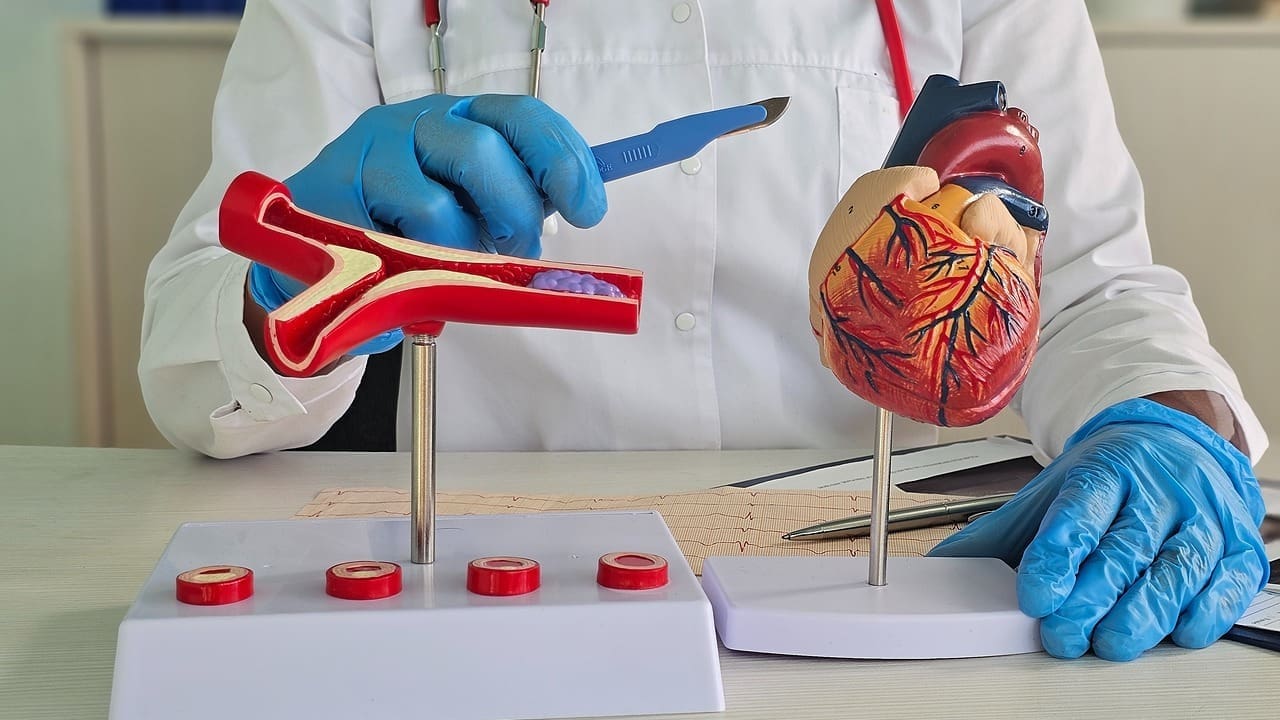
Hemodynamic Effects of Patent Ductus Arteriosus
Understanding the hemodynamic effects of PDA is key to its clinical importance. PDA changes blood flow patterns, affecting both pulmonary and systemic circulation.
Blood Flow Patterns
In a normal heart, blood flows well to meet the body’s needs. But with PDA, an abnormal connection between the aorta and pulmonary artery occurs. This causes left-to-right shunting of blood. Oxygenated blood from the aorta goes back into the pulmonary artery, increasing blood volume in the pulmonary circulation.
Impact on Pulmonary Circulation
The increased blood flow from PDA can cause pulmonary hypertension over time. A study on Nature.com shows this can lead to serious health issues if not treated. The high pressure and volume can harm the pulmonary vasculature, causing complications.
Systemic Effects
PDA also has systemic effects. The heart works harder, leading to cardiac fatigue and possibly heart failure if not treated. The diastolic runoff can also lower diastolic blood pressure, affecting coronary perfusion.
In summary, PDA’s hemodynamic effects are complex, affecting both pulmonary and systemic circulation. It’s vital to understand these effects to manage PDA effectively.
Clinical Manifestations and Symptoms
Understanding PDA symptoms is key to early detection and treatment. The signs can vary based on the ductus arteriosus size and the patient’s age.
Symptoms in Infants
Infants with PDA may not grow well and have respiratory distress. These issues come from too much blood flow to the lungs. This can lead to lung congestion.
Larger PDAs usually cause more severe symptoms at a younger age.
Presentation in Children and Adults
In older kids and adults, PDA might not show symptoms at all. Or, it might cause nonspecific symptoms like palpitations or shortness of breath when trying to exercise. Doctors often find it by chance during exams or tests for other reasons.
Bounding Pulses and Other Physical Signs
Bounding pulses are a key sign of PDA. They happen because of the wide pulse pressure from blood flowing into the pulmonary artery. You might also hear a continuous murmur, like a “machinery” sound, at the left upper chest.
Spotting these signs is vital for diagnosing and treating PDA on time.
Diagnostic Approaches for PDA
We use a multi-faceted approach to diagnose PDA. This includes physical exams, imaging, and ruling out other conditions. This method helps us accurately identify PDA and tell it apart from similar conditions.
Physical Examination Findings
A thorough physical exam is key in diagnosing PDA. We look for a continuous murmur, often called a “machinery” sound. This sound is best heard at the left upper sternal border.
We also check for bounding pulses and a wide pulse pressure. These signs show the blood is shunting left-to-right.
Imaging Techniques
Imaging is vital in confirming PDA diagnosis. We use advanced imaging to see the ductus arteriosus. This helps us assess its size and shape.
Echocardiography
Echocardiography is a main tool for diagnosing PDA. It lets us see the ductus arteriosus and check its size. Doppler echocardiography shows the continuous flow typical of PDA.
Cardiac Catheterization
Cardiac catheterization is also key, mainly for planning PDA closure. It gives detailed info on the PDA’s anatomy and its effects on blood flow.
Differential Diagnosis: PDA vs. PFO
Distinguishing PDA from patent foramen ovale (PFO) is critical. Both involve abnormal heart communications. But, their locations, sizes, and effects are different.
| Characteristics | PDA | PFO |
|---|---|---|
| Location | Between aorta and pulmonary artery | Between atria |
| Typical Murmur | Continuous “machinery” murmur | No characteristic murmur |
| Diagnostic Method | Echocardiography, Cardiac Catheterization | Echocardiography with bubble study |
Treatment Options: Methods to Close Ductus Arteriosus
Choosing the right treatment for patent ductus arteriosus (PDA) depends on several factors. These include the size of the PDA and the patient’s health. We will look at different treatment strategies, from medical management to more invasive procedures.
Medical Management
Medical management is often the first step for PDA, mainly in premature babies. It uses medicines to help close the ductus arteriosus.
NSAIDs and Prostaglandin Inhibitors
Nonsteroidal anti-inflammatory drugs (NSAIDs) like indomethacin and ibuprofen are used to close the PDA. They work by stopping the production of prostaglandins. Prostaglandins help keep the ductus arteriosus open.
Watchful Waiting Approach
In some cases, doctors might choose to wait and watch, mainly for small PDAs. They closely monitor the patient for any signs of problems or if the PDA doesn’t close on its own.
Catheter-Based Interventions
For those who need more than just medicine, catheter-based interventions offer a less invasive option than surgery.
PDA Coil Embolization
PDA coil embolization uses coils or other devices through a catheter to block the PDA. This is done under X-ray guidance.
Occluder Devices
Occluder devices are another way to close a PDA. They are delivered through a catheter and come in different sizes to fit various PDA diameters.
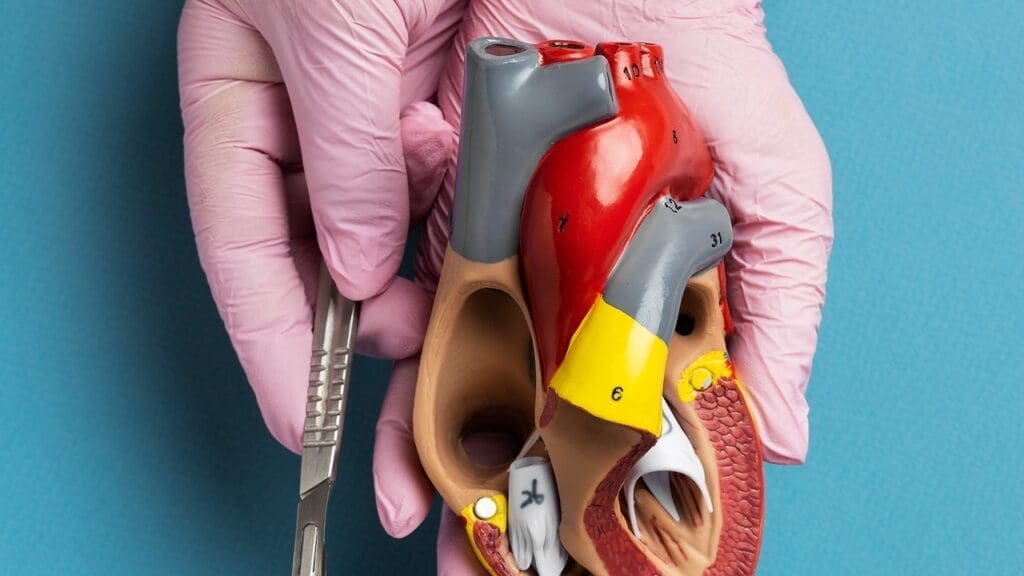
Surgical Options for Closing Ductus Arteriosus
Surgery is also an option for PDA, mainly when other treatments don’t work or aren’t possible.
Surgical Ligation
Surgical ligation closes the PDA directly through a chest incision. This method has been used for many years and is effective.
Video-Assisted Thoracoscopic Surgery
Video-assisted thoracoscopic surgery (VATS) is a less invasive method. It uses a thoracoscope to see the PDA during ligation. This approach can lead to quicker recovery and less scarring.
We summarize the treatment options for PDA in the following table:
| Treatment Option | Description | Advantages |
|---|---|---|
| Medical Management | Use of NSAIDs to promote PDA closure | Non-invasive, effective for premature infants |
| Catheter-Based Interventions | Deployment of coils or occluder devices | Minimally invasive, reduced recovery time |
| Surgical Ligation | Direct closure of PDA through thoracotomy | Effective, traditional method |
| VATS | Less invasive surgical technique using thoracoscope | Reduced scarring, faster recovery |
Long-Term Outcomes and Complications
It’s important to know how Patent Ductus Arteriosus (PDA) affects people over time. Closing PDA can greatly improve a person’s life. It makes them feel better and live more comfortably.
Prognosis After PDA Closure
Most people get much better after PDA is closed. The surgery works well to stop the shunt. This lowers the chance of serious problems.
Getting treatment early is very important. It helps avoid long-term heart issues.
Potential Complications if Left Untreated
Not treating PDA can cause big problems. These include pulmonary hypertension, heart failure, and a higher risk of endocarditis. It can also lead to breathing issues and other health problems.
Follow-up Care Requirements
After PDA closure, regular check-ups are needed. These visits help catch any issues early. They also make sure the heart is working right.
Doctors will do echocardiograms and check-ups with a cardiologist. This helps keep an eye on the heart’s health.
Knowing about PDA’s long-term effects helps doctors give better care. This improves patients’ lives and health.
Conclusion
Understanding Patent Ductus Arteriosus (PDA) is key for both patients and doctors. We’ve looked at the ductus arteriosus’s role and why it might stay open. We’ve also covered the different types of PDA and the “machinery” murmur it makes.
Early diagnosis and treatment are critical to avoid serious problems. We’ve talked about how to diagnose and treat PDA. This includes medical care, catheter-based treatments, and surgery. The right treatment depends on the PDA’s size, the patient’s age, and symptoms.
In short, managing PDA well is essential. By grasping its main points, we can offer better care and better results. It’s also important to keep an eye on patients after they’ve had PDA treatment for any new issues.
FAQ
What is Patent Ductus Arteriosus (PDA)?
Patent Ductus Arteriosus is a condition where the ductus arteriosus, a vital blood vessel in the fetal circulation, fails to close after birth. This leads to abnormal blood flow between the pulmonary artery and the aorta.
What is the function of the ductus arteriosus in fetal development?
The ductus arteriosus is key in fetal development. It bypasses the lungs, allowing blood to flow directly from the pulmonary artery to the aorta. This supplies oxygenated blood to the fetus.
What are the symptoms of PDA in infants?
Infants with PDA may show symptoms like rapid breathing and poor feeding. They may also fail to gain weight at a normal rate, due to the heart’s increased workload.
How is PDA diagnosed?
PDA is diagnosed through physical examination and imaging. The “machinery” murmur is a key finding. Echocardiography and cardiac catheterization are also used.
What are the treatment options for PDA?
Treatment options include medical management with NSAIDs and prostaglandin inhibitors. Catheter-based interventions like PDA coil embolization are also used. Surgical options include ligation and video-assisted thoracoscopic surgery.
What is the difference between PDA and PFO?
PDA is when the ductus arteriosus fails to close. PFO is when the foramen ovale, a hole in the heart, remains open. Both can cause abnormal blood flow but have different implications.
What are the possible complications if PDA is left untreated?
Untreated PDA can lead to complications like pulmonary hypertension and heart failure. It also increases the risk of endocarditis. Timely diagnosis and treatment are key.
How is PDA classified?
PDA is classified by size and shape. This affects its clinical presentation and treatment options. Size-based classification includes small, moderate, and large PDAs.
What is the prognosis after PDA closure?
The prognosis after PDA closure is generally excellent. Most people see significant symptom improvement and a reduced risk of complications.
What follow-up care is required after PDA treatment?
After PDA treatment, regular check-ups with a healthcare provider are needed. These check-ups monitor for complications and assess treatment effectiveness.
References
- Merck Manuals Professional Version (Patent Ductus Arteriosus (PDA)) : https://www.merckmanuals.com/professional/pediatrics/congenital-cardiovascular-anomalies/patent-ductus-arteriosus-(pda
- NCBI Bookshelf (Patent Ductus Arteriosus) : https://www.ncbi.nlm.nih.gov/books/NBK430758
- American Heart Association (AHA) (Patent Ductus Arteriosus (PDA)) : https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects/patent-ductus-arteriosus-pda