Coronary artery disease affects millions worldwide. Many need treatment to improve heart health. The question is, when does a blockage need a stent?
Knowing the severity of heart blockage is key to choosing the right treatment. Symptoms show a blockage is there, but how bad it is decides if a stent is needed.
Our cardiologists look at each patient’s situation closely. They consider 70 percent heart blockage symptoms and overall heart health. This helps them decide the best treatment.
Key Takeaways
- Coronary artery disease can lead to significant blockages requiring medical intervention.
- The severity of the blockage is a critical factor in determining the need for a stent.
- Symptoms and overall health are considered when evaluating the need for stenting.
- Personalized care is essential in treating coronary artery disease effectively.
- Advanced treatments, including stenting, are available for managing coronary artery disease.
Understanding Coronary Artery Disease and Blockages
Coronary artery disease is a major cause of heart problems. It happens when the coronary arteries get damaged or diseased. This leads to plaque buildup in the walls, causing blockages that harm heart health.
How Arterial Blockages Develop
Blockages form over time due to plaque buildup. This plaque is made of fat, cholesterol, and other substances. Factors like diet, lifestyle, and genetics can affect this process.
As plaque grows, it narrows the arteries. This restricts blood flow to the heart. It’s important to know what causes plaque buildup to prevent and manage coronary artery disease.
Risk factors include high cholesterol, smoking, hypertension, and diabetes. By managing these, people can lower their risk of blockages.
Measuring Blockage Percentage
The severity of blockage is measured as a percentage. This shows how much the artery is narrowed. Tests like angiograms and stress tests help diagnose a 70 percent heart blockage.
Serious symptoms of heart blockage include chest pain, shortness of breath, and fatigue. Spotting these symptoms early is key for timely treatment. We’ll look at these symptoms in more detail later.
The Spectrum of Heart Blockage Severity
Coronary artery disease comes in different levels of blockage. Each level affects treatment choices. Knowing the severity is key to picking the right treatment.
Mild Blockage (30-50%)
Mild blockages narrow the arteries by 30% to 50%. People might not feel any symptoms yet. But, it’s a time to start making lifestyle changes and taking medicine to stop it from getting worse.
Moderate Blockage (50-70%)
Moderate blockages narrow the arteries by 50% to 70%. At this point, people might feel chest pain when they exert themselves. Doctors will focus on managing symptoms and stopping the disease from getting worse.
Severe Blockage (70% and Above)
Severe blockages narrow the arteries more than 70%. The risk of a heart attack goes up a lot. Doctors might suggest stenting or coronary artery bypass grafting (CABG) to treat it.
Knowing the severity of heart blockage is more than just a number. It’s about how it affects a person’s life and the risk of future heart problems.
|
Blockage Severity |
Percentage |
Typical Symptoms |
Treatment Approach |
|---|---|---|---|
|
Mild |
30-50% |
Often asymptomatic |
Lifestyle modifications, monitoring |
|
Moderate |
50-70% |
Chest pain on exertion |
Medical management, possible stenting |
|
Severe |
70% and above |
Frequent chest pain, shortness of breath |
Aggressive treatment, stenting, or CABG |
Personalized care is vital for managing heart blockage. The best treatment depends on the person’s health, the blockage’s details, and other risk factors.
70 Percent Heart Blockage Symptoms
Knowing the signs of a 70 percent heart blockage is key for quick medical help. A blockage this big can really hurt your heart’s function. It leads to symptoms that you should watch out for.
Common Physical Symptoms
People with a 70 percent heart blockage might feel a few things. These include:
- Chest pain or discomfort, known as angina, which can feel like pressure or squeezing in the chest.
- Shortness of breath, even at rest or with minimal exertion.
- Fatigue or feeling weak, which can be persistent and debilitating.
- Swelling in the legs, ankles, or feet due to fluid buildup.
Exertion-Related Symptoms
Some symptoms get worse or start with physical activity or stress. These might be:
- Increased chest pain or angina during physical activity.
- Dizziness or lightheadedness, potentially leading to fainting spells.
- Rapid or irregular heartbeat, which can be unsettling.
Silent Symptoms and Hidden Dangers
Some people might not notice symptoms until it’s too late. This is why regular check-ups and screenings are so important.
“The absence of symptoms does not necessarily mean the absence of significant coronary artery disease.” –
A statement from the American Heart Association
The symptoms of a 70 percent heart blockage can differ from person to person. Spotting these signs early is vital for getting medical help fast.
|
Symptom Category |
Common Symptoms |
|---|---|
|
Common Physical Symptoms |
Chest pain, shortness of breath, fatigue, swelling |
|
Exertion-Related Symptoms |
Increased chest pain, dizziness, rapid or irregular heartbeat |
|
Silent Symptoms |
No noticeable symptoms until advanced stages |
Signs of 70 Percent Heart Blockage That Shouldn’t Be Ignored
It’s vital to recognize the signs of a 70 percent heart blockage early. A blocked coronary artery can lead to serious health issues if not treated.
We will look at the main signs of a 70 percent heart blockage. Knowing these signs can help people get medical help quickly.
Chest Pain Patterns
Chest pain, or angina, is a common sign of a big heart blockage. The pain can feel like pressure or tightness in the chest. It can happen when you’re active or stressed.
The chest pain from a 70 percent heart blockage can be different for everyone. Some people might feel:
- Discomfort that spreads to the arms, back, neck, jaw, or stomach
- Pain that gets worse with activity or feels better when you rest
- A feeling of heaviness or squeezing in the chest
Not everyone with a big heart blockage will have chest pain. Some might not feel any pain at all. That’s why it’s important to watch for other symptoms too.
Shortness of Breath
Shortness of breath, or dyspnea, is another important symptom. It happens when the heart can’t pump enough blood. This makes you feel like you can’t breathe well.
Shortness of breath can happen when you’re active or even when you’re resting. It’s a sign that shouldn’t be ignored, along with chest pain or feeling tired.
Fatigue and Weakness
Fatigue and weakness are common in people with big heart blockages. The heart muscle doesn’t get enough blood. This makes you feel tired or weak.
These symptoms can make everyday tasks harder. In some cases, fatigue and weakness might be the only symptoms. It’s important to watch for any changes in how you feel.
Knowing these signs can help you get medical help early. This can prevent more serious problems.
Diagnostic Methods for Heart Blockage
Diagnosing heart blockage uses both non-invasive and invasive tests. These methods help find the right treatment for a 70 percent blockage. It’s important to get an accurate diagnosis.
Non-Invasive Tests
Non-invasive tests are the first step in finding heart blockage. They include:
- Electrocardiogram (ECG): This test records the heart’s electrical activity to spot problems.
- Stress Test: It checks how the heart works when stressed, often through exercise or medicine.
- Echocardiogram: Sound waves create heart images to check its shape and how it works.
Invasive Diagnostic Procedures
If non-invasive tests show a big blockage, more detailed tests might be needed. These are:
- Coronary Angiography: A dye is injected into the arteries to see blockages.
- Cardiac Catheterization: It measures heart pressures and checks for artery disease directly.
Interpreting Test Results
After tests, doctors look at the results to figure out the blockage’s severity. They then talk about treatment options for 70 percent heart blockage. This might include stents or other treatments.
It’s key for patients to understand their diagnosis and treatment. We help explain everything to our patients.
When Does a Blockage Require a Stent?
Deciding on stent placement involves looking at clinical guidelines and how severe the symptoms are. When dealing with treatment options for 70 percent heart blockage, doctors consider many factors. They aim to find the best treatment for each patient.
Medical Guidelines for Stent Placement
Guidelines from medical associations are key in deciding on stent use. Cardiology groups say stents are often needed for blockages causing serious symptoms or at high risk of heart attack.
The American Heart Association and the American College of Cardiology have guidelines. These help doctors decide when stenting is right. They look at blockage percentage, symptoms, and the patient’s health.
“The decision to place a stent should be based on a thorough evaluation. This includes the patient’s symptoms, the blockage’s location, and their overall health.”
Factors Beyond Percentage
Blockage percentage is important, but not the only thing to consider. Other factors include:
- The blockage’s location in the artery
- Presence of symptoms like chest pain or shortness of breath
- The patient’s medical history, including past heart attacks or procedures
- Results from tests, both non-invasive and invasive
|
Factor |
Description |
Impact on Stent Decision |
|---|---|---|
|
Blockage Location |
Proximity to major branches or within a critical segment |
Influences technical difficulty and risk |
|
Symptoms |
Presence and severity of angina or dyspnea |
Affects urgency and necessity of stenting |
|
Medical History |
Previous MI, PCI, or CABG |
Impacts choice between stenting and other treatments |
Emergency vs. Elective Stenting
Stenting can be urgent or planned. Emergency stenting is for heart attacks to quickly restore blood flow.
Elective stenting is planned for those with stable heart disease. The timing depends on symptoms, ischemia extent, and the patient’s health.
Managing 70 percent heart blockage often requires lifestyle changes, medication, and sometimes stenting. The approach is tailored to each patient’s needs.
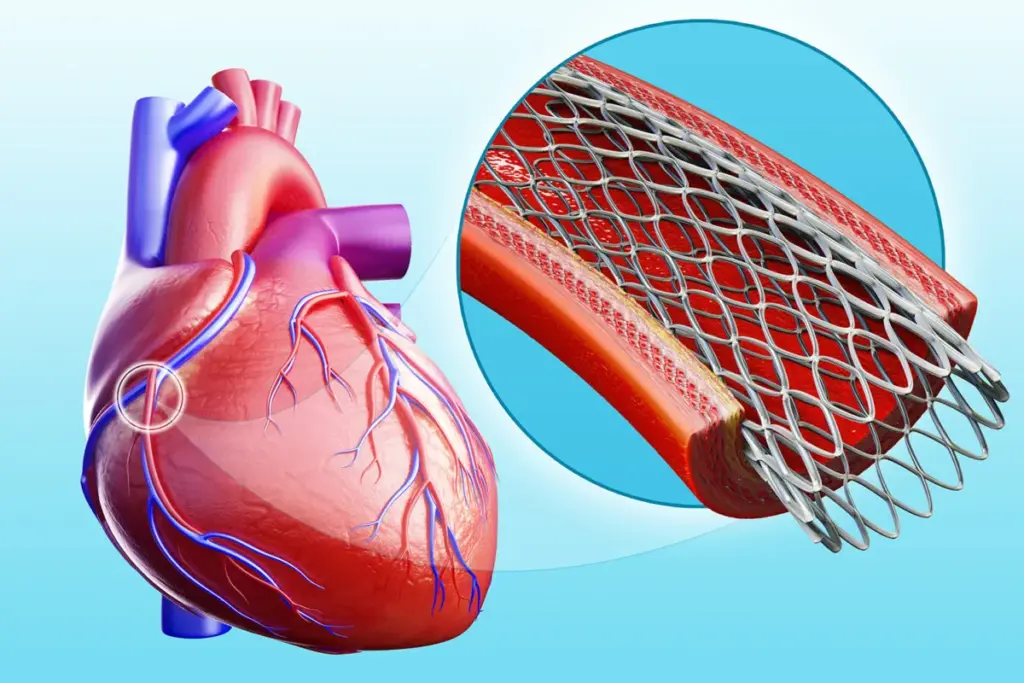
The Stent Procedure Explained
The stent procedure is a common treatment for coronary artery disease. It involves placing a small mesh tube to keep the artery open. Cardiologists who specialize in interventional cardiology perform this procedure.
Types of Stents Available
There are several types of stents, each with its own characteristics. The main types include:
- Bare-metal stents: Made of metal, these stents are designed to keep the artery open.
- Drug-eluting stents: Coated with medication, these stents help prevent the artery from re-narrowing.
While both types are effective, drug-eluting stents are more commonly used. They reduce the risk of restenosis.
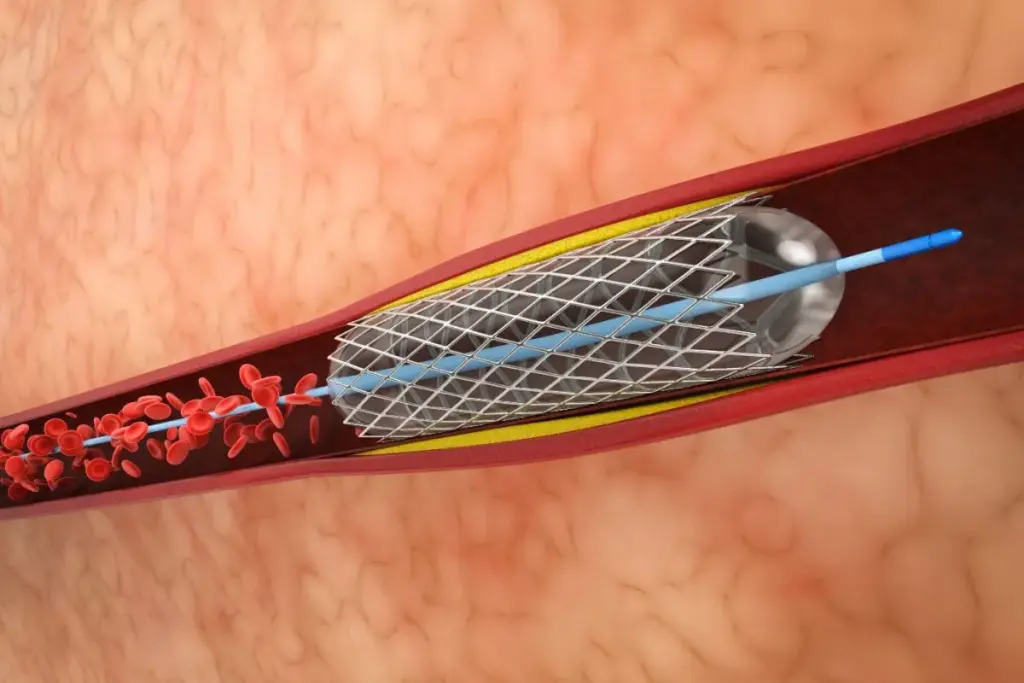
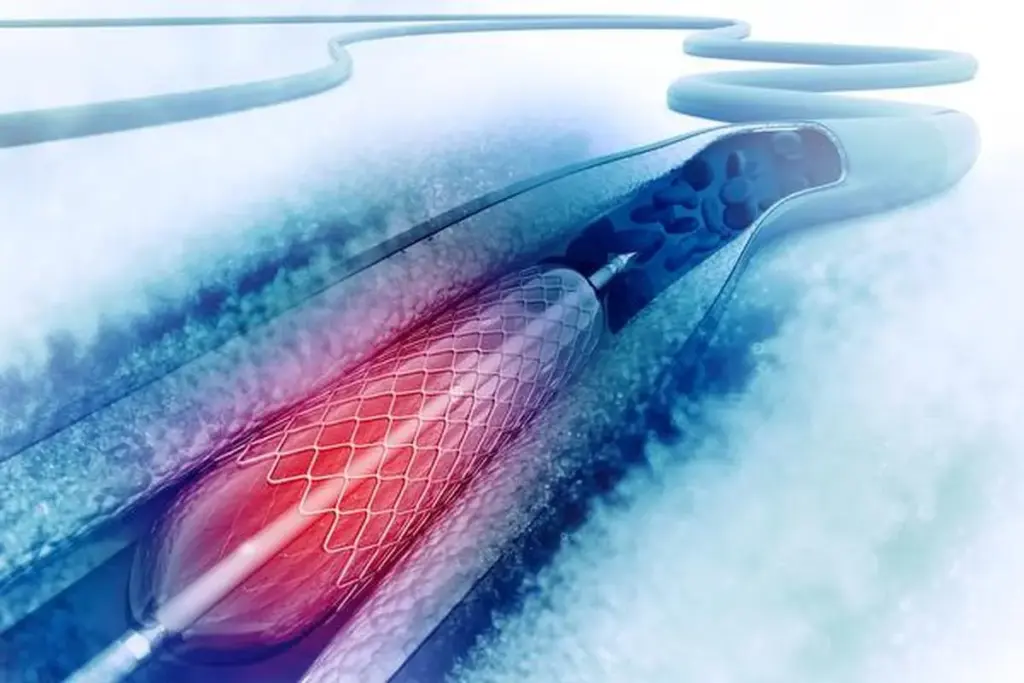
What Happens During Stent Placement
A catheter is inserted into the blocked artery through a small incision in the groin or arm. Using X-ray imaging, the cardiologist guides the catheter to the blockage site. A balloon is then inflated to expand the stent, pushing it against the artery walls.
Once the stent is in place, the balloon is deflated and removed. This leaves the stent to keep the artery open.
Immediate Post-Procedure Care
After the procedure, patients are monitored for a few hours to check for any complications. Medications are prescribed to prevent blood clots from forming on the stent. Patients are usually advised to rest for a day or two and avoid strenuous activities.
Follow-up appointments are scheduled to check on the healing progress and adjust medications as necessary.
In some cases, the stent procedure may be performed with other treatments. This includes ICD placement surgery or heart defib surgery for patients with complex heart conditions. Our medical team will discuss the best treatment plan tailored to the patient’s specific needs.
Alternative Treatments for Heart Blockage
Managing a 70 percent heart blockage can involve more than just stenting. While stenting is common, other treatments might be better for some people.
Medication Management
For some, medication is key in treating heart blockage. It helps manage symptoms, slow disease, and prevent serious problems.
- Antiplatelet agents to prevent blood clots
- Beta-blockers to reduce heart rate and blood pressure
- Statins to lower cholesterol levels
- ACE inhibitors to manage blood pressure and reduce heart strain
The American Heart Association says, “Medications are vital in heart disease management, often with lifestyle changes and other treatments.”
“Medications in coronary artery disease treatment are complex. They aim to ease symptoms and improve survival.”
Coronary Artery Bypass Grafting (CABG)
CABG is a surgery that bypasses blocked arteries with grafts. These grafts are usually from other body parts. It helps improve blood flow to the heart.
|
Procedure |
Description |
Benefits |
|---|---|---|
|
CABG |
Bypassing blocked coronary arteries |
Improved blood flow, symptom relief |
|
Minimally Invasive CABG |
Less invasive version of CABG |
Smaller incisions, quicker recovery |
Lifestyle Modifications as Treatment
Lifestyle changes are key in managing heart blockage. They can slow disease progression and improve health.
Dietary Changes: Eating a heart-healthy diet can help manage cholesterol and blood pressure.
Exercise Regularly: Regular physical activity, as advised by doctors, can boost heart health and overall well-being.
By trying these alternative treatments, patients with 70 percent heart blockage can see big improvements. It’s important to work with healthcare providers to find the best treatment plan.
Implantable Cardioverter Defibrillators (ICDs) for Heart Patients
ICDs are advanced devices that help prevent sudden cardiac death. They watch the heart’s rhythm and shock it back to normal if needed.
When ICDs Are Recommended
We suggest ICDs for those at high risk of sudden cardiac arrest. This includes people with ventricular tachycardia or ventricular fibrillation. The choice to get an ICD depends on a patient’s medical history and current health.
The American Heart Association says ICDs are good for patients who have had cardiac arrest or dangerous arrhythmias. “ICDs have been shown to significantly reduce mortality in patients at high risk of sudden cardiac death.”
ICD Placement Surgery Process
The surgery to put in an ICD is minor. It’s done under local anesthesia and sedation. The device is placed under the skin in the chest and connected to the heart.
notes,
“The ICD placement surgery is a safe and effective procedure that can significantly improve the quality of life for patients at risk of sudden cardiac death.”
Living with an ICD
Having an ICD means some changes in lifestyle, but most people can get back to normal in a few weeks. It’s key to follow the doctor’s advice on medication, appointments, and lifestyle changes.
People with ICDs should know about possible risks like lead malfunction or device failure. Regular check-ups and care can help avoid these issues.
Understanding ICDs helps patients manage their heart conditions better. This can lower the risk of sudden cardiac death.
Recovery from Stent Placement
After getting a stent, it’s important to follow a recovery plan. This helps the procedure work well. We’ll show you what to expect and how to recover smoothly.
Hospital Stay Duration
How long you stay in the hospital after a stent varies. Usually, patients stay for 24 to 48 hours to watch for problems. A patient said, “The hospital care was top-notch, making me feel better.” It’s key to catch any issues early.
Activity Restrictions
After a stent, you’ll need to avoid certain activities. These are to help you heal right:
- Don’t lift heavy or do hard work for at least a week
- Don’t do too much exercise for a time your doctor says
- Start doing normal things again when your doctor says it’s okay
It’s important to stick to these rules to avoid problems and heal well.
Medication Regimen
Following your medication plan is a big part of recovery. You’ll take:
- Medicine to stop clots on the stent
- Medicine for high blood pressure or cholesterol
A cardiologist said, “Taking your medicine as told is key for the stent’s success.” Being consistent is important to keep the stent working right and prevent heart issues later.
By knowing and following these recovery tips, you can get better faster after a stent.
Recovery from ICD Implant Surgery
The recovery after ICD implant surgery is key. It needs careful attention and following doctor’s orders. Knowing the recovery stages can greatly affect the outcome.
Immediate Post-Surgical Care
Right after surgery, patients stay in a recovery area. They are watched for any issues. Rest and avoiding hard work are key in the first days.
“The first 24 to 48 hours are critical,” says a top cardiologist.
Patients should:
- Avoid heavy lifting or bending
- Keep the incision site clean and dry
- Watch for signs of infection or other problems
Return to Work After ICD Implant
Going back to work after surgery depends on the job and how well you recover. It’s best to talk to your doctor about when to go back.
Usually, it takes 4 to 6 weeks to go back to work if your job is physical. But, if you have a desk job, you might go back sooner, with your doctor’s okay.
“Your health should come first,” says a healthcare expert. “Follow your doctor’s advice on going back to work.”
Long-term Considerations
Long-term care means regular check-ups with your doctor. It’s also important to eat well and exercise to keep your heart healthy.
You might need to replace the ICD battery or make adjustments later. Knowing how to manage your condition is key.
By sticking to these tips and talking to your doctor, you can recover well. This will help you live better with an ICD.
Living with 70 Percent Heart Blockage
Managing a 70 percent heart blockage needs a mix of diet changes, regular exercise, and stress control. These lifestyle changes can greatly improve life quality and lower the risk of more problems.
Dietary Recommendations
Eating right is key for a 70 percent heart blockage. Focus on foods low in saturated fats, cholesterol, and sodium. Key dietary recommendations include:
- Eat more fruits, vegetables, and whole grains
- Choose lean proteins like poultry, fish, and legumes
- Reduce foods high in added sugars and refined carbs
Adding foods rich in omega-3s, like salmon and walnuts, is also good. They help lower inflammation and boost heart health.
Exercise Guidelines
Regular exercise is vital for a 70 percent heart blockage. It improves heart health, lessens symptoms, and boosts well-being. Recommended exercises include:
- Brisk walking
- Swimming
- Cycling
- Low-impact aerobics
Always talk to a doctor before starting any new exercise. They can help pick the best activities and levels for you.
Stress Management Techniques
Managing stress well is important for a 70 percent heart blockage. Stress can make heart conditions worse. So, finding healthy ways to deal with stress is key. Stress reduction techniques may include:
- Meditation and mindfulness practices
- Deep breathing exercises
- Yoga
- Progressive muscle relaxation
Doing things that bring joy and calm can also help reduce stress.
By making these lifestyle changes, people with a 70 percent heart blockage can manage their condition better. They can also improve their health and well-being overall.
Preventing Further Blockage Progression
Managing heart blockage is complex. We need to focus on preventing it from getting worse. A 70 percent heart blockage needs a detailed plan. This plan should tackle the current issue and prevent future problems.
Medication Adherence
Following your medication plan is key. Drugs like antiplatelets, beta-blockers, and statins help keep your heart healthy. They lower the risk of more blockages and serious issues.
Being consistent with your meds is important. Try setting reminders, using pill boxes, or asking a family member for help. This ensures you take your meds as directed.
Regular Monitoring
Regular check-ups are essential. They help catch any heart changes early. This includes doctor visits, tests like echocardiograms, and watching for new symptoms.
By keeping up with these checks, we can spot problems early. This allows for quick action that can greatly improve your health.
Lifestyle Optimization
Improving your lifestyle is also vital. This means making diet, exercise, and stress changes. It’s about eating right, staying active, quitting smoking, and managing stress.
- Eat a diet full of fruits, veggies, whole grains, and lean proteins.
- Do regular exercise, like walking, that fits your health and abilities.
- Stay away from tobacco and drink less alcohol.
- Try stress-reducing activities like meditation or yoga.
By changing your lifestyle, you can lower your heart blockage risk. This improves your life quality too.
In summary, stopping blockage progression needs a full plan. This includes sticking to your meds, regular check-ups, and lifestyle changes. With the right approach and choices, managing a 70 percent heart blockage is possible. This can also reduce the risk of serious problems.
When to Seek Emergency Care
Knowing when to seek emergency care for heart blockage can save lives. It’s important to know when to act fast to avoid serious problems or even death.
Warning Signs of Heart Attack
It’s key to recognize heart attack warning signs. Look out for chest pain or discomfort that feels like pressure or tightness. This pain can spread to the arms, back, neck, jaw, or stomach.
Other signs include shortness of breath, feeling lightheaded, or discomfort in the upper body.
If you or someone else has these symptoms, act fast. Call emergency services or head to the nearest hospital right away.
Symptoms of Stent Complications
After getting a stent, watch for signs of trouble. Look out for chest pain that’s worse than before. Other signs are shortness of breath, feeling tired, or generally not feeling well.
If you notice these symptoms, get medical help right away. Catching stent problems early can make a big difference.
ICD Alert Signals
For those with an Implantable Cardioverter Defibrillator (ICD), knowing the alert signals is vital. These devices help control abnormal heart rhythms. If you get multiple shocks in a short time, it’s a medical emergency.
Also, if you feel dizziness, lightheadedness, or palpitations and your ICD is active, seek help immediately.
Conclusion
Managing heart blockage needs a full approach. This includes knowing the condition, its signs, and sticking to treatment plans. We’ve looked at heart blockage’s severity, how it’s diagnosed, and treatments like stenting and lifestyle changes.
Handling a 70 percent heart blockage means more than just medical help. It also means big changes in how you live. Knowing how severe heart blockage is helps patients choose the right treatments and care.
At our place, we aim to give top-notch healthcare to everyone, including international patients. Our team works hard to give care that fits each patient’s needs. This way, we help them get the best results.
With the help of doctors and following treatment plans, people with heart blockage can live full lives. We urge patients to stay up-to-date and involved in their care. This way, they can keep their hearts healthy.
FAQ
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5880567/[4
What are the symptoms of a 70 percent heart blockage?
Symptoms include chest pain and shortness of breath. You might also feel tired or weak. Some people have symptoms only when they exert themselves or none at all.
How is heart blockage severity categorized?
Severity is based on the blockage percentage in coronary arteries. It ranges from mild (30-50%) to moderate (50-70%) to severe (70% and above).
At what percentage of blockage is a stent typically required?
A stent might be needed for a blockage of 70% or higher. This decision depends on several factors, including medical guidelines and the patient’s symptoms.
What is the difference between emergency and elective stenting?
Emergency stenting is for acute coronary syndromes or heart attacks. Elective stenting is planned for significant blockages.
What are the alternative treatments for heart blockage beside stenting?
Treatments include medication, coronary artery bypass grafting (CABG), and lifestyle changes. These include diet, exercise, and stress management.
When are Implantable Cardioverter Defibrillators (ICDs) recommended?
ICDs are for those at high risk of sudden cardiac death. This includes severe heart blockage or other heart conditions.
What is the recovery process like after stent placement?
Recovery includes a hospital stay and activity restrictions. You’ll also need medication to prevent clotting and promote healing.
How long does it take to recover from ICD implant surgery?
Recovery from ICD implant surgery is gradual. It involves careful post-surgical care and a slow return to work. Long-term care ensures the device works right.
What lifestyle changes are necessary for managing 70 percent heart blockage?
Managing 70 percent heart blockage requires a healthy diet and regular exercise. Stress management and medication adherence are also key to prevent further blockage.
How can I prevent further blockage progression?
Preventing further blockage involves sticking to medication and regular monitoring. A healthy diet, exercise, and stress management are also important.
When should I seek emergency care for heart blockage?
Seek emergency care for heart attack warning signs, stent complications, or ICD alert signals.









