
An ascending aortic aneurysm is a serious condition. It happens when the aorta, the main artery, gets too big. This can go unnoticed for years, making it very important to know about its risks and how to manage it.
At Liv Hospital, we take the risk of an aneurysm of the ascending aorta without rupture very seriously. Our team is focused on giving you the best care. We use the latest methods to help those at risk.
Getting an early diagnosis and treatment can save lives. In this article, we’ll talk about the risks, causes, and how to manage aneurysm of ascending aorta without rupture. We aim to give you important information about this condition and what you can expect from our services.
Key Takeaways
- Understanding the risks associated with aneurysm of ascending aorta without rupture.
- The importance of early detection and intervention.
- Overview of the causes and symptoms of ascending aortic aneurysm.
- Management strategies for aortic arch dilation.
- Liv Hospital’s approach to treating aneurysm of ascending aorta without rupture.
What Is an Aneurysm of Ascending Aorta Without Rupture
It’s important to understand what an aneurysm of the ascending aorta without rupture is. We’ll explore its definition and how it grows. This knowledge helps in managing and treating the condition.
Definition and Pathophysiology
An aneurysm of the ascending aorta without rupture is when the top part of the aorta gets bigger but doesn’t burst. This happens when the aorta’s wall gets weak. Hypertension and age-related degeneration play big roles in causing this.
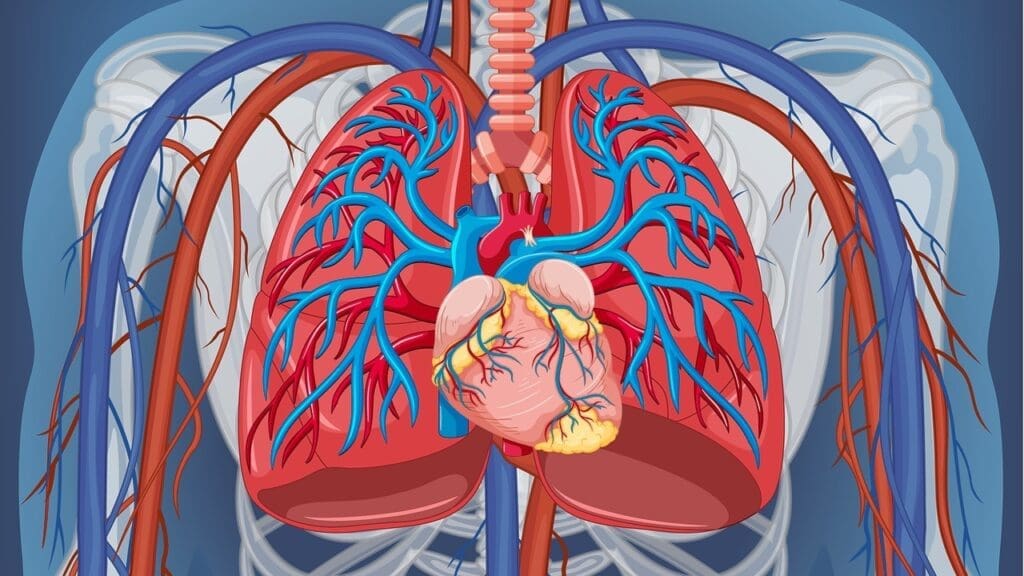
The aorta has three layers: intima, media, and adventitia. In aneurysms, the media layer gets damaged. This damage can come from genes, like Marfan syndrome, or from high blood pressure.
Ascending Aortic Enlargement Patterns
An aneurysm in the ascending aorta grows slowly. How fast it grows varies from person to person. Aneurysms under 4 cm are very unlikely to burst. But, the risk goes up when they get bigger than 5.5 cm.
The aneurysm usually grows by 1-2 mm each year. But, it can grow faster if blood pressure is high or if there are genetic issues.
It’s key to watch how big the aneurysm gets and how fast. Doctors use tests like echocardiography or CT scans to check its size. This helps decide when to take action.
Epidemiology and Prevalence
Studies on ascending aortic aneurysms give us important data. They tell us how common these conditions are and who they affect. This info helps us plan for public health and manage care better.
Incidence Rates in the United States
In the United States, ascending aortic aneurysms are a big worry for public health. About 10 in 100,000 people get them each year. We’ll look at the numbers and what affects them.
Most thoracic aortic aneurysms happen in the ascending aorta. This makes studying them even more important.
| Population | Incidence Rate (per 100,000) |
|---|---|
| General Population | 10 |
| High-Risk Groups | 50 |
Demographic Distribution and Risk Groups
Who gets ascending aortic aneurysms varies by age and gender. We’ll talk about who’s at higher risk. This includes people with certain genes and those with high blood pressure.
Risk Factors: Being born with certain genes, having high blood pressure, and getting older are big risks.
- Genetic predispositions: Some genes make you more likely to get it.
- Hypertension: High blood pressure is a big risk factor.
- Age: Older people are more likely to get it.
Anatomical Considerations of the Aorta
Understanding the aorta’s anatomy is key to managing aortic aneurysms. The aorta is the largest artery in the body. Its structure is vital for diagnosing and treating aneurysms.
The aorta has different sections, with the ascending aorta and aortic arch being key areas for aneurysms. Knowing these sections helps doctors give the right care.
Ascending Aorta vs Aortic Arch: Critical Distinctions
The ascending aorta and aortic arch are two parts of the aorta with unique features. The ascending aorta starts at the left ventricle and ends at the innominate artery. The aortic arch then goes from the innominate artery to the left subclavian artery.
- The ascending aorta is more likely to get aneurysms because of its size and pressure.
- The aortic arch is harder to fix surgically because of its shape and branches.
Knowing these differences is key for diagnosing and treating aneurysms. For example, surgeries for aneurysms in the ascending aorta might differ from those in the aortic arch.
Structural Vulnerabilities of the Ascending Aortic Artery
The ascending aortic artery is at risk because of its structure. Its wall faces high pressure and stress, making it more likely to develop aneurysms.
- The media layer of the ascending aorta has many elastic fibers. These can weaken with high blood pressure.
- The ascending aorta also gets atherosclerosis easily, which weakens its wall further.
These weaknesses show why it’s important to watch and manage risks for aneurysms in the ascending aorta.
In summary, knowing the aorta’s anatomy, like the differences between the ascending aorta and aortic arch, is vital for managing aortic aneurysms. By understanding the ascending aortic artery’s weaknesses, doctors can give better care to those at risk.
Natural Progression and Growth Patterns
It’s important to know how ascending aortic aneurysms grow. They usually get bigger slowly over time. Their growth is influenced by different factors.
Typical Growth Rates
Aneurysms of the ascending aorta grow about 1-2 mm each year. But, this rate can change as the aneurysm gets bigger. The size of the aneurysm is key in figuring out its growth rate and risks.
Growth Rate Acceleration: When the aneurysm gets larger, the stress on its walls goes up. This can make it grow faster. It’s vital to watch these changes closely for timely action.
Factors Accelerating Aneurysm Expansion
Several things can make an ascending aortic aneurysm grow faster. These include:
- Hypertension: High blood pressure puts more stress on the aortic wall, making it grow faster.
- Genetic predisposition: Some genetic conditions can make the aortic wall weaker, leading to quicker growth.
- Connective tissue disorders: Conditions like Marfan syndrome can also weaken the aortic wall, raising the risk of faster growth.
| Factor | Effect on Aneurysm Growth |
|---|---|
| Hypertension | Increases wall stress, promoting faster growth |
| Genetic Predisposition | Affects aortic wall integrity, potentially leading to more rapid expansion |
| Connective Tissue Disorders | Weakens the aortic wall, increasing the risk of accelerated growth |
Knowing these factors and keeping an eye on the aneurysm’s growth is key. It helps manage the condition well and avoid serious problems.
Risk Assessment for Aneurysm in Ascending Aorta
To figure out the risk of rupture for ascending aortic aneurysms, we need to look at several things. These include the size of the aneurysm, the patient’s risk factors, and if they have symptoms.
Getting the risk right is key to choosing the best treatment for patients with ascending aortic aneurysms. It helps doctors decide if surgery is needed or if they can just watch and wait. This is important for preventing rupture and improving patient outcomes.
Size-Related Risk Stratification
The size of the aneurysm is very important when assessing the risk of rupture. Research shows that the risk goes up a lot when the aneurysm gets close to or bigger than 5.5 cm. So, the size of the aneurysm is a main factor in deciding the risk level.
- Aneurysms less than 4 cm are usually at lower risk of rupture.
- Aneurysms between 4 cm and 5.4 cm need regular checks and looking at other risk factors.
- Aneurysms 5.5 cm or bigger are high-risk and often need surgery.
Additional Risk Factors for Rupture
There are other things that can make the risk of rupture higher. These include:
- Genetic predispositions: People with a family history of aortic aneurysms or certain genetic disorders (like Marfan syndrome) are at higher risk.
- Hypertension: High blood pressure that’s not controlled can put more stress on the aortic wall, raising the risk of rupture.
- Rate of aneurysm growth: Aneurysms that grow fast are considered higher risk.
- Presence of symptoms: Aneurysms that cause symptoms may be at higher risk of rupture.
By looking at these factors, doctors can do a more detailed risk assessment. This helps them tailor treatment plans to meet each patient’s specific needs.
Causes of Ascending Aortic Aneurysm
Understanding what causes ascending aortic aneurysms is key to managing them. We’ll look at genetic predispositions, hypertension, connective tissue disorders, and age-related changes.
Genetic Predisposition and Inherited Disorders
Genetics play a big role in ascending aortic aneurysms. Certain inherited conditions can weaken the aortic wall. For example, Marfan syndrome and Ehlers-Danlos syndrome increase the risk.
Familial thoracic aortic aneurysms and dissections (FTAAD) are also genetic. People with a family history of aortic issues should get genetic screening and counseling.
Hypertension and Cardiovascular Contributors
Hypertension is a big risk factor for ascending aortic aneurysms. High blood pressure can stretch and weaken the aortic wall. Other heart issues like atherosclerosis and valve problems can also contribute.
Controlling hypertension through lifestyle changes and medication can lower the risk of aneurysms. Regular check-ups with a healthcare provider are important for those with hypertension.
Connective Tissue Disorders
Conditions like Marfan syndrome and Ehlers-Danlos syndrome raise the risk of aneurysms. These disorders affect the aortic wall’s structure, making it more likely to dilate and form an aneurysm.
People with these conditions need regular monitoring and follow-up with a healthcare provider to manage their condition and prevent complications.
Age-Related Degenerative Changes
As we age, our aortic walls can weaken, increasing the risk of aneurysms. The risk grows after age 60.
Regular screenings can help catch issues early. This allows for timely management and treatment.
| Cause | Description | Risk Factors |
|---|---|---|
| Genetic Predisposition | Inherited disorders that weaken the aortic wall | Family history, Marfan syndrome, Ehlers-Danlos syndrome |
| Hypertension | Chronic high blood pressure | High blood pressure, cardiovascular disease |
| Connective Tissue Disorders | Conditions that affect the structural integrity of the aortic wall | Marfan syndrome, Ehlers-Danlos syndrome |
| Age-Related Degenerative Changes | Changes that occur as we age | Age over 60, atherosclerosis |
Symptoms of Ascending Aortic Aneurysm
Ascending aortic aneurysms often have no symptoms until they grow large or dissect. This makes them very dangerous. The lack of symptoms can make people feel safe, but it’s not true.
Asymptomatic Presentation and Incidental Discovery
Many people with an ascending aortic aneurysm don’t show any symptoms. This means the aneurysm is often found by accident during tests for other reasons. Regular check-ups and screenings are key for early detection, for those with a family history or other risk factors.
Warning Signs and Symptoms
As an ascending aortic aneurysm grows, it may start to cause symptoms. These include:
- Chest pain or discomfort, which can spread to the back
- Back pain, often in the upper or middle back
- Difficulty breathing or shortness of breath from trachea or bronchi compression
- Hoarseness or coughing from recurrent laryngeal nerve compression
It’s vital to recognize these symptoms and get medical help if they don’t go away or get worse.
Emergency Symptoms Requiring Immediate Medical Attention
An aortic dissection or rupture can cause severe symptoms that need quick medical help. Emergency symptoms include:
- Sudden, severe chest or back pain that feels like tearing or ripping
- Severe pain that spreads to the arms, legs, or jaw
- Fainting or loss of consciousness
- Shortness of breath
- Weak or absent pulse in the arms or legs
If you or someone you know has these symptoms, get emergency medical care right away.
Diagnostic Approaches for Aortic Arch Dilation
Healthcare experts use advanced imaging to diagnose aortic arch dilation. These methods help spot and track aneurysms. This is key for early treatment.
Imaging Techniques
Many imaging tools are used to diagnose aortic arch dilation. They help us see the aorta and check for any swelling or aneurysms.
- Computed Tomography (CT) scans: CT scans give detailed images of the aorta. They help measure its size and spot any swelling.
- Magnetic Resonance Imaging (MRI): MRI gives clear images of the aortic arch without harmful radiation. It’s great for long-term checks.
- Transthoracic Echocardiography (TTE): TTE uses ultrasound to show the heart and aorta in real-time. It’s good for first checks and follow-ups.
- Transesophageal Echocardiography (TEE): TEE uses a probe in the esophagus for detailed aortic arch images.
Each imaging method has its own benefits. We choose the best one for each patient’s needs and the specifics of their aortic arch dilation.
Monitoring Protocols for Unruptured Aneurysms
Patients with unruptured aortic arch aneurysms need regular checks. We watch how big the aneurysm gets and how fast. How often we check depends on the aneurysm’s size and other health factors.
| Aneurysm Size (cm) | Recommended Monitoring Interval |
|---|---|
| < 4.0 | 12 months |
| 4.0 – 5.4 | 6-12 months |
| ≥ 5.5 | 3-6 months or consider surgical intervention |
We adjust the check-up plan based on the aneurysm’s growth and the patient’s health. This way, we catch any big changes early and act fast when needed.
Treatment Options for Dilated Aortic Arch
Treatment for a dilated aortic arch includes surgery, medical management, and lifestyle changes. The right treatment depends on the aneurysm size, the patient’s health, and other factors.
Surgical Interventions as Definitive Treatment
Surgery is often the best choice for large or symptomatic aneurysms. Open surgery replaces the dilated aorta with a synthetic graft. This complex procedure requires cutting through the breastbone to reach the aorta.
Endovascular repair is a less invasive option. It involves placing a stent-graft inside the aorta to block blood flow to the aneurysm. This method is best for high-risk patients or those with certain anatomical features.
| Surgical Approach | Description | Indications |
|---|---|---|
| Open Surgery | Replacement of the dilated aorta with a synthetic graft | Large or symptomatic aneurysms |
| Endovascular Repair | Placement of a stent-graft to exclude the aneurysm | High-risk patients or specific anatomical features |
Medical Management Strategies
For smaller aneurysms or those not ready for surgery, medical management is key. It includes controlling hypertension and other heart risks. Beta-blockers and ACE inhibitors help reduce aortic wall stress.
Regular imaging tests are vital to monitor the aneurysm’s size and growth. This allows for timely surgery if needed.
Lifestyle Modifications and Risk Reduction
Lifestyle changes are important for managing aortic arch dilation. Quitting smoking is essential, as it greatly increases aneurysm risk. Eating well and exercising regularly also help manage blood pressure and heart health.
By making these lifestyle changes and following medical advice, patients can lower their risk of complications from a dilated aortic arch.
Conclusion: Living with an Unruptured Ascending Aortic Aneurysm
Living with an unruptured ascending aortic aneurysm means you need to be careful. Regular check-ups and imaging tests are key. They help track the aneurysm’s size and growth.
Managing your condition well is important. This includes controlling high blood pressure and living a healthy lifestyle. Avoiding smoking is also vital. These steps can lower your risk of serious problems.
It’s important to know the signs that mean you need to see a doctor right away. Being proactive and informed helps manage your condition. This can lead to better health outcomes.
FAQ
What is an aneurysm of the ascending aorta?
An aneurysm of the ascending aorta is when the main artery, the aorta, gets too big. It happens in the part closest to the heart. This can go unnoticed for a long time, making it important to know the risks and how to prevent it.
What are the risk factors for developing an aneurysm of the ascending aorta?
Factors that increase the risk include genetics, high blood pressure, age, and certain diseases like Marfan and Ehlers-Danlos syndromes.
How is an aneurysm of the ascending aorta diagnosed?
Doctors use CT scans, MRI, or echocardiography to see the aorta and find any aneurysms.
What are the symptoms of an ascending aortic aneurysm?
Many aneurysms don’t show symptoms and are found by accident. But, some may cause chest or back pain. Severe cases can lead to aortic dissection or rupture, which is a medical emergency.
How is an unruptured ascending aortic aneurysm managed?
Doctors monitor it with imaging, control blood pressure, and suggest lifestyle changes. Sometimes, surgery is needed.
What is the typical growth rate of an ascending aortic aneurysm?
Aneurysms usually grow about 1-2mm each year. But, this can change based on the size and other factors.
When is surgical intervention recommended for an ascending aortic aneurysm?
Surgery is often suggested for big aneurysms or those causing symptoms. The risk of rupture goes up with size.
Can lifestyle modifications help reduce the risk of aneurysm growth or rupture?
Yes, living a healthy lifestyle can help. This includes keeping blood pressure in check, not smoking, and staying active.
What is the difference between the ascending aorta and the aortic arch?
The ascending aorta starts at the heart, while the aortic arch curves and supplies blood to the head and arms. Knowing the difference is key for diagnosing and treating aneurysms.
Are there any genetic tests available for assessing the risk of an ascending aortic aneurysm?
Yes, genetic tests can spot inherited conditions that raise the risk of aneurysms, like Marfan syndrome.






