Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we know how critical it is to manage aortic regurgitation well. This issue happens when the aortic valve leaks, causing blood to flow back into the heart. If not treated, it can cause serious problems. Luckily, there are many treatments to help control symptoms and better patient outcomes.
New medical technologies have made managing this condition better. For example, the Trilogy transcatheter valve has a one-year survival rate of 91.9% in severe cases. This gives patients new hope. We will look at the different medication options and treatments, sharing their benefits and possible results.
Key Takeaways
- Understanding the importance of managing aortic regurgitation.
- Overview of available treatments for aortic regurgitation.
- The role of medication in controlling symptoms.
- Latest advancements in aortic regurgitation treatment.
- Insights into the Trilogy transcatheter valve’s effectiveness.
Understanding Aortic Valve Regurgitation
Aortic regurgitation happens when the aortic valve doesn’t close well. This lets blood leak back into the left ventricle. If not treated, it can cause heart failure and arrhythmias.
Pathophysiology of Aortic Valve Leakage
The aortic valve leaks because it doesn’t close right. This lets blood flow back into the left ventricle. It can be caused by damage to the valve, a big aortic root, or diseases affecting the valve.
Key factors contributing to aortic valve leakage include:
- Degenerative valve disease
- Endocarditis
- Aortic dissection
- Marfan syndrome
- Rheumatic fever
Symptoms and Clinical Presentation
People with aortic regurgitation might not show symptoms for years. But, as it gets worse, they might feel dyspnea on exertion, palpitations, and chest pain. The symptoms depend on how severe and long-lasting the regurgitation is.
Doctors might hear a diastolic murmur at the left sternal border. They might also notice a widened pulse pressure and signs of heart failure in severe cases.
Diagnostic Criteria and Assessment
Echocardiography is key for diagnosing aortic regurgitation. It lets doctors see the valve and measure how bad the leak is. Cardiac MRI and CT angiography can also check the aortic root and ascending aorta.
Diagnostic criteria include:
- Echocardiographic evidence of aortic regurgitation
- Quantification of regurgitant fraction and effective regurgitant orifice area
- Assessment of left ventricular size and function
Getting the diagnosis right is important. It helps decide when to use medicine or surgery for aortic regurgitation.
Goals of Aortic Regurgitation Medication

The goals of medication for aortic regurgitation are to control symptoms and slow the disease’s progress. We aim to manage the condition effectively. This means easing symptoms and slowing the disease’s advancement.
Symptom Control vs. Disease Modification
Controlling symptoms is a key goal in treating aortic regurgitation. Vasodilators and diuretics help reduce heart workload. This relieves symptoms like shortness of breath and fatigue.
Disease modification aims to slow valve leakage and heart failure. ACE inhibitors are used for this purpose. It’s important to balance symptom control and disease modification.
Symptom control improves life quality. But, disease modification is key to prevent long-term heart damage.
Preventing Heart Failure Progression
Stopping heart failure from getting worse is vital in managing aortic regurgitation. ACE inhibitors and calcium channel blockers help by reducing afterload. This makes it easier for the heart to pump blood.
Timing of Medical vs. Surgical Intervention
Choosing between medical and surgical treatment depends on several factors. These include symptom severity, valve leakage, and left ventricular function. Medical therapy is often the first choice. But, surgery is needed when symptoms worsen or the condition progresses.
| Factor | Medical Intervention | Surgical Intervention |
|---|---|---|
| Symptom Severity | Mild to Moderate | Severe |
| Valve Leakage | Mild to Moderate | Severe |
| Left Ventricular Dysfunction | Absent or Mild | Significant |
ACE Inhibitors: First-Line Aortic Regurgitation Medication
ACE inhibitors are key in treating aortic regurgitation. They help ease symptoms and slow the disease’s progress. Knowing how they work and how to use them helps doctors treat patients better.
Mechanism of Action in Valve Regurgitation
ACE inhibitors block the conversion of angiotensin I to angiotensin II. This reduces blood pressure and heart load. In aortic regurgitation, they lessen the backflow of blood, helping the heart work less hard.
Lisinopril and Other Common ACE Inhibitors
Lisinopril is a top choice for treating aortic regurgitation. It’s easy to take once a day and has fewer side effects. Other options include enalapril, captopril, and ramipril. Each has its own benefits, depending on the patient’s needs.
The right ACE inhibitor depends on the patient’s health and other medicines. For example, lisinopril’s long action means it only needs to be taken once a day, making it easier for patients to stick to their treatment.
Dosing Strategies and Monitoring Requirements
Starting with a low dose of ACE inhibitors is common. This dose can be increased as needed. For lisinopril, the first dose is usually 2.5 to 5 mg, and it can go up to 20 to 40 mg a day.
It’s important to watch kidney function and potassium levels. ACE inhibitors can raise potassium levels and harm the kidneys in some cases.
Regular check-ups are vital to see how well ACE inhibitors are working. Doctors will check blood pressure, kidney function, and heart failure symptoms. Changes to the treatment plan might be needed based on these checks.
Calcium Channel Blockers for Aortic Insufficiency
Calcium channel blockers are a key treatment for aortic regurgitation. They help by making the heart work less hard. This improves symptoms for people with aortic insufficiency.
Amlodipine (Norvasc): Indications and Benefits
Amlodipine is a type of calcium channel blocker used for aortic regurgitation. It’s mainly for high blood pressure and chest pain. But, it also helps with aortic insufficiency by lowering blood pressure.
Amlodipine is good because it lasts all day. This means you only need to take it once a day. It’s also safe for long-term use.
Diltiazem and Other Options
Diltiazem is another calcium channel blocker for aortic regurgitation. It works differently than amlodipine. It affects heart rate and how well the heart contracts.
Verapamil and nifedipine are also options. But, they might not be used as much because of their side effects or how they work.
Combination Therapy with ACE Inhibitors
Using calcium channel blockers with ACE inhibitors is a good strategy for aortic regurgitation. ACE inhibitors lower blood pressure and the amount of blood going back to the heart. Calcium channel blockers also lower blood pressure.
This combo is great for those who need strong treatment. But, it’s important to watch for too much blood pressure drop and low blood pressure.
Diuretics in Managing Aortic Regurgitation Symptoms
Diuretics are key in managing aortic regurgitation symptoms. They help reduce fluid overload. This makes it easier for the heart to work and improves the patient’s life quality.
Loop Diuretics vs. Thiazides
The choice between loop diuretics and thiazides depends on fluid retention and kidney function. Loop diuretics, like furosemide, are stronger for severe fluid overload.
- Loop diuretics work on the Loop of Henle in the kidneys, helping get rid of sodium and water.
- Thiazide diuretics are weaker but work well for mild fluid retention.
Both diuretics have their uses in aortic regurgitation management. The right choice depends on the patient’s needs and doctor’s judgment.
Controlling Fluid Retention and Congestion
Diuretics mainly help with fluid retention and congestion in aortic regurgitation patients. They reduce fluid in the body, easing the heart’s workload.
Good diuretic therapy can lead to:
- Less heart failure symptoms
- Better exercise ability
- Better overall life quality
Electrolyte Management During Diuretic Therapy
Managing electrolytes is vital during diuretic therapy. Diuretics can cause a loss of important electrolytes like potassium and magnesium. This can lead to problems if not managed right.
| Electrolyte | Common Issues | Management Strategies |
|---|---|---|
| Potassium | Hypokalemia (low potassium levels) | Potassium supplements or potassium-sparing diuretics |
| Magnesium | Magnesium deficiency | Magnesium supplements |
It’s important to regularly check electrolyte levels and adjust diuretic therapy as needed. This ensures safe use and prevents complications in managing aortic regurgitation symptoms.
Beta Blockers: Limited Applications in Treatment
Beta blockers are key in treating many heart problems. But, their use in aortic regurgitation is more complex.
Beta blockers are not usually the first option for aortic regurgitation. Yet, there are times when they might be considered.
When Beta Blockers May Be Appropriate
In some cases, beta blockers can be used for aortic regurgitation. This is more common when patients also have high blood pressure or heart disease.
- Hypertension: Beta blockers help manage high blood pressure, which often goes with aortic regurgitation.
- Coronary artery disease: They can lower the risk of heart attacks and chest pain in those with heart disease.
Risks and Contraindications
Even with benefits, beta blockers can be risky for those with aortic regurgitation. The main worry is they might slow the heart rate. This could make the regurgitation worse by letting the heart fill longer.
| Risks | Consequences |
|---|---|
| Reduced heart rate | Increased diastolic filling time, potentially worsening regurgitation |
| Negative inotropic effect | Reduced left ventricular function, potentially exacerbating heart failure symptoms |
Monitoring Heart Rate and Blood Pressure Response
Using beta blockers in aortic regurgitation patients requires close monitoring to prevent harm.
Regular visits should check heart rate, blood pressure, and symptoms. Echocardiograms might also be needed to look at heart function and regurgitation severity.
Vasodilators and Other Supportive Medications
Vasodilators and other medications are key in treating aortic regurgitation. They help ease symptoms and improve life quality. They might also slow down the disease’s progress.
Hydralazine and Nitrates Combination
Hydralazine and nitrates together are a good treatment for aortic regurgitation. Hydralazine widens blood vessels, helping the heart work better. Nitrates mainly widen veins, easing heart failure symptoms.
Benefits of Hydralazine and Nitrates Combination:
- Improved symptom control
- Enhanced exercise tolerance
- Potential delay in disease progression
Angiotensin Receptor Blockers as Alternatives
Angiotensin receptor blockers (ARBs) are another option for aortic regurgitation. They block a certain receptor, causing blood vessels to widen. This lowers blood pressure.
Key advantages of ARBs include:
- Similar benefits to ACE inhibitors
- Potential for reduced cough incidence compared to ACE inhibitors
- Useful in patients with ACE inhibitor intolerance
Emerging Pharmacological Approaches
New research aims to find better treatments for aortic regurgitation. This includes new vasodilators, anti-inflammatory drugs, and treatments for specific molecular pathways.
Comparison of Vasodilators Used in Aortic Regurgitation
| Medication | Mechanism of Action | Primary Benefits |
|---|---|---|
| Hydralazine | Direct vasodilator | Reduces afterload, improves cardiac output |
| Nitrates | Venodilation | Reduces preload, alleviates heart failure symptoms |
| ARBs | Blocks angiotensin II type 1 receptor | Vasodilation, reduced blood pressure |
In conclusion, vasodilators and other medications are vital in managing aortic regurgitation. Understanding these options helps healthcare providers create personalized treatment plans. This improves outcomes and quality of life for patients.
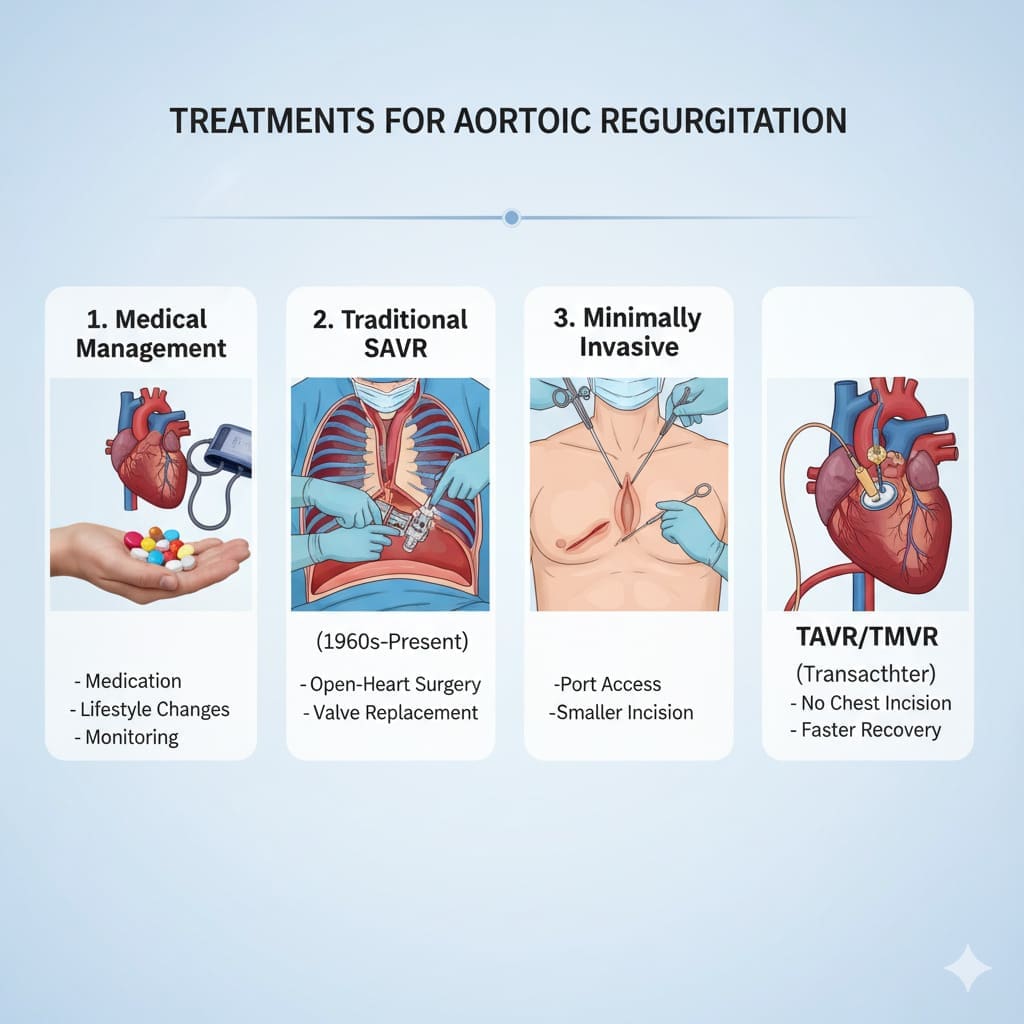
Advanced Interventions: Beyond Medication
Advanced treatments offer new hope for patients with aortic regurgitation. When medication isn’t enough, we use more invasive but effective methods.
Surgical Valve Replacement Options
Surgical valve replacement is key for severe aortic regurgitation. It involves replacing the aortic valve with a new one. Mechanical valves last long but need lifelong blood thinners. Bioprosthetic valves don’t need blood thinners but don’t last as long.
Choosing between mechanical and bioprosthetic valves depends on many factors. We look at age, lifestyle, and health to decide the best option for each patient.
Trilogy Transcatheter Valve: 91.9% One-Year Survival Rate
The Trilogy transcatheter valve is a big step forward in treating aortic regurgitation. It has a 91.9% one-year survival rate. This makes it a good choice for some patients instead of traditional surgery.
Transcatheter aortic valve replacement (TAVR) with the Trilogy valve is less invasive. It’s great for patients at high risk for surgery or who can’t have surgery.
Patient Selection for Transcatheter Procedures
Choosing the right patients for transcatheter procedures is key. We look at how severe the aortic regurgitation is, the heart’s function, and other health issues. Advanced imaging helps us decide the best treatment.
By carefully evaluating these factors and using the latest technology, we create personalized treatment plans. This helps improve outcomes for patients with aortic regurgitation.
Conclusion: Optimizing Aortic Regurgitation Treatment
Treating aortic regurgitation needs a mix of medicines and sometimes surgery. We’ve looked at treatments like ACE inhibitors and calcium blockers. These help manage symptoms and slow the disease.
Choosing the right medicine for each patient is key. This approach improves their life and health. It’s all about matching treatment to the patient’s needs.
Our understanding of aortic regurgitation is growing. A mix of medicines and advanced treatments works best. This way, we can give patients the best care possible.
FAQ
What is aortic regurgitation and how is it treated?
Aortic regurgitation happens when the aortic valve leaks. This lets blood flow back into the heart. Treatment starts with medicines to manage symptoms and slow the disease. Surgery is considered when the disease is more advanced.
What are the primary goals of aortic regurgitation medication?
The main goals of aortic regurgitation medication are to control symptoms and slow the disease. We also aim to prevent heart failure. We use ACE inhibitors, calcium channel blockers, and diuretics to achieve this.
How do ACE inhibitors work in treating aortic regurgitation?
ACE inhibitors, like lisinopril, relax blood vessels. This reduces blood flow back into the heart and lowers the heart’s workload. It helps manage symptoms and slow the disease.
What is the role of calcium channel blockers in treating aortic insufficiency?
Calcium channel blockers, such as amlodipine and diltiazem, relax blood vessels. They reduce the heart’s workload. They can be used alone or with ACE inhibitors to manage symptoms and slow the disease.
How do diuretics help manage symptoms of aortic regurgitation?
Diuretics reduce fluid retention and congestion by increasing urine production. This relieves symptoms like shortness of breath and fatigue. We use loop diuretics and thiazides, monitoring electrolyte levels closely.
Are beta blockers effective in treating aortic regurgitation?
Beta blockers have limited use in treating aortic regurgitation. They can sometimes worsen the condition. But, they might be used in certain situations, like hypertension or arrhythmias, under close watch.
What are the benefits of vasodilators in managing aortic regurgitation?
Vasodilators, like hydralazine and nitrates, relax blood vessels. This reduces blood flow back into the heart. They can be used alone or with other medications to manage symptoms and slow the disease.
What are the advanced interventions available for aortic regurgitation?
Advanced treatments include surgical valve replacement and transcatheter valve replacement, like the Trilogy transcatheter valve. These are usually for patients with severe symptoms or advanced disease.
How is patient selection determined for transcatheter procedures?
Choosing patients for transcatheter procedures depends on several factors. These include symptom severity, valve damage extent, and overall health. We evaluate each patient’s needs to find the best treatment.
What is the role of pharmaceutical interventions in managing aortic regurgitation?
Medications like ACE inhibitors, calcium channel blockers, diuretics, and vasodilators are key in managing aortic regurgitation. They help control symptoms, slow disease progression, and improve patient outcomes.
Are there any emerging pharmacological approaches for aortic regurgitation?
Yes, new medications and treatment strategies are emerging for aortic regurgitation. We stay updated with the latest research to offer the best care for our patients.
References
Discover Aortic Regurgitation (Informational Site): AR Treatment Options