Understanding moderate aortic stenosis is key to good heart health. This condition narrows the aortic valve opening. This can block blood flow from the heart to the body.
People with this condition might feel chest pain, get tired easily, or have trouble breathing. These symptoms often happen when they’re active. It’s important to watch for these signs and get the right care to avoid worse problems.
At Liv Hospital, we offer top-notch heart care. Our team is here to help with aortic stenosis. We provide detailed support and the latest treatments.
Key Takeaways
- Moderate aortic stenosis is defined by specific echocardiographic criteria.
- Symptoms can include chest pain, fatigue, and shortness of breath.
- Regular monitoring is key to avoid complications.
- Effective management means a detailed treatment plan.
- Liv Hospital offers patient-focused heart care with the latest treatments.
What Is Aortic Stenosis and How Does It Develop?
Let’s dive into aortic stenosis, starting with the basics. The aortic valve is key to the heart, controlling blood flow to the body. It’s vital for our heart’s health.
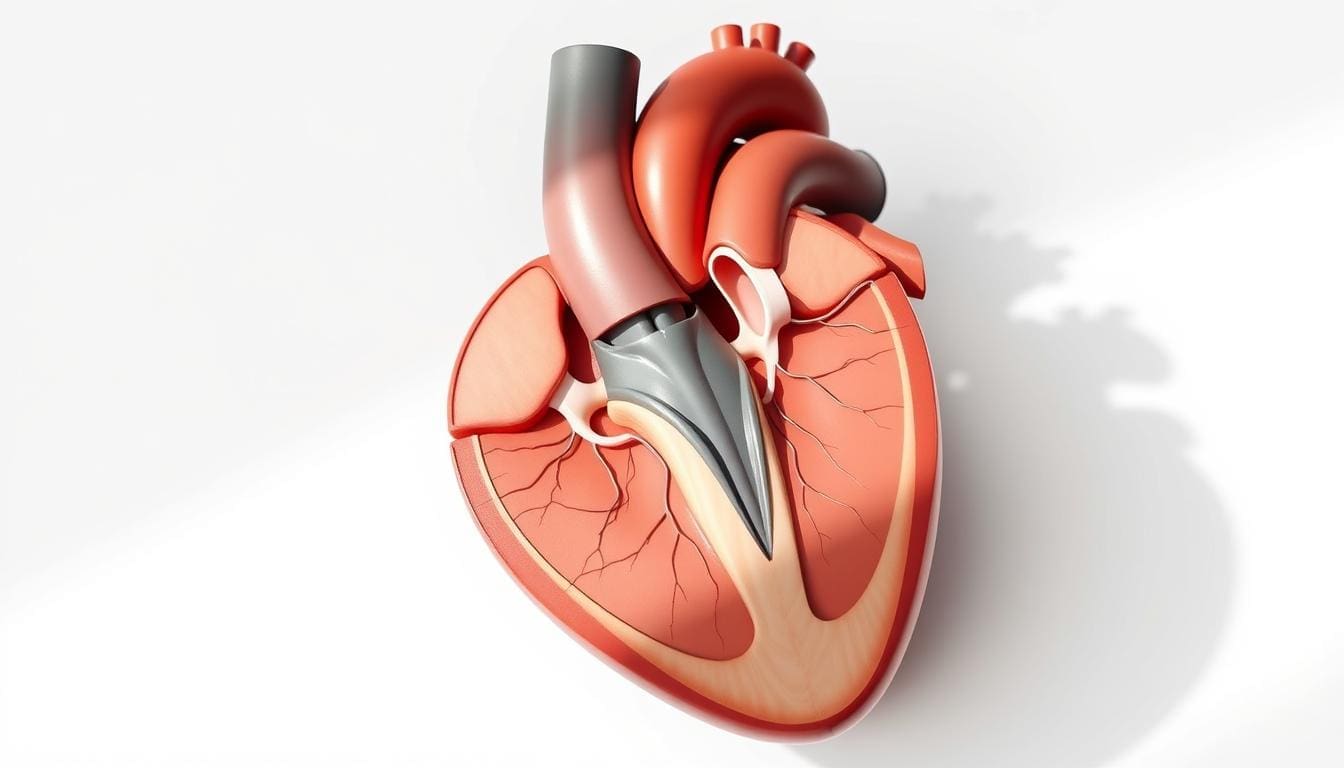
The Anatomy of a Healthy Aortic Valve
A healthy aortic valve has three parts that open and close with each heartbeat. This lets blood flow forward and keeps it from going back. Its function is essential for good blood flow and heart health.
Pathophysiology of Aortic Stenosis
Aortic stenosis happens when the valve’s parts become stiff or stick together. This narrows the valve opening and blocks blood flow. It makes the heart work harder, leading to symptoms like chest pain and shortness of breath.
The disease progresses due to changes like calcification and fibrosis in the valve. Knowing these changes helps in finding ways to manage it.
Common Causes and Risk Factors
Several things can lead to aortic stenosis, including:
- Age: The risk grows with age, more so after 60.
- Calcification: Calcium buildup on the valve can cause stenosis.
- Congenital Heart Defects: People born with certain heart defects are at higher risk.
- Lifestyle and Medical Conditions: High blood pressure, high cholesterol, and smoking can speed up the disease.
Managing these factors can slow down aortic stenosis. Studies show that controlling them is key to keeping the heart healthy and avoiding complications.
While we can’t reverse aortic stenosis, a good management plan can help. Knowing the causes and risk factors helps us take care of our heart health.
Understanding Moderate Aortic Stenosis: Definition and Classification

Understanding moderate aortic stenosis starts with knowing its definition and how it’s measured. It’s a heart disease where the aortic valve gets narrower. This blocks blood flow from the left ventricle to the aorta. Doctors use echocardiography to measure how severe it is.
Echocardiographic Criteria for Moderate Aortic Stenosis
Echocardiography is key for diagnosing and classifying aortic stenosis. It looks at the speed of blood flow and the size of the valve. These help doctors decide the best treatment.
Transaortic velocity is important. It shows how fast blood flows across the valve. Faster flow means more severe stenosis.
Transaortic Velocity and Valve Area Measurements
To spot moderate aortic stenosis, doctors use specific measurements. These include:
- Peak transaortic velocity
- Mean pressure gradient across the aortic valve
- Aortic valve area calculated using the continuity equation
The aortic valve area is also key. It’s found using the continuity equation. This equation looks at blood flow in the left ventricle and the aorta.
| Parameter | Mild Stenosis | Moderate Stenosis | Severe Stenosis |
|---|---|---|---|
| Peak Velocity (m/s) | 2.0 – 2.9 | 3.0 – 3.9 | ≥ 4.0 |
| Mean Gradient (mmHg) | < 20 | 20 – 39 | ≥ 40 |
| Valve Area (cm²) | 1.5 – 2.0 | 1.0 – 1.5 | < 1.0 |
Differentiating Between Mild, Moderate, and Severe Stenosis
Telling mild, moderate, and severe aortic stenosis apart is vital. The table shows how to do it. It looks at peak velocity, mean gradient, and valve area.
“Accurate diagnosis and classification of aortic stenosis severity are essential for guiding treatment decisions and improving patient outcomes.”
We use these criteria to figure out how severe aortic stenosis is. Knowing the differences helps doctors give the right care to patients.
7 Essential Facts About Moderate Aortic Stenosis You Should Know
We will explore seven key facts about moderate aortic stenosis. These facts are essential for patients to know. Understanding them can help individuals manage their condition better and make informed decisions about their care.
Prevalence Across Different Age Groups
Moderate aortic stenosis can happen at any age. But, it’s more common among older adults. The incidence significantly increases after the age of 65.
Natural Progression of the Condition
Moderate aortic stenosis can get worse over time. The rate of progression varies among individuals. Regular monitoring is key to managing the condition effectively.
Research shows that age, smoking, and hypertension can affect how fast the condition progresses.
Impact on Cardiac Function and Output
Moderate aortic stenosis can greatly affect the heart’s function and output. As it progresses, symptoms like chest pain, fatigue, and shortness of breath can occur. Understanding its impact on cardiac health is vital for managing the condition.
Relationship to Other Cardiovascular Conditions
Aortic stenosis often coexists with other heart conditions. These include hypertension, coronary artery disease, and heart failure. Managing these conditions is essential for overall cardiac health and prognosis.
| Condition | Relationship to Aortic Stenosis | Management Strategy |
|---|---|---|
| Hypertension | Can exacerbate aortic stenosis progression | Monitor and control blood pressure |
| Coronary Artery Disease | Can coexist and complicate surgery | Assess and manage CAD alongside AS |
| Heart Failure | Can result from untreated severe AS | Monitor for signs of heart failure |
Managing moderate aortic stenosis requires a detailed approach. This includes monitoring its progression, understanding its impact on cardiac function, and addressing related heart conditions. By knowing these essential facts, individuals can better navigate their condition and improve their overall cardiac health.
Recognizing the Symptoms of Moderate Aortic Stenosis
It’s key to spot the signs of moderate aortic stenosis early. As it gets worse, people may face symptoms that really affect their life.
Chest Pain and Angina During Activity
Chest pain or angina often shows up when you’re active. This happens because your heart doesn’t get enough oxygen-rich blood. It feels like pain or discomfort in your chest.
Feeling chest pain is scary. It’s vital to talk to a doctor to figure out why and how to handle it.
Fatigue and Exercise Intolerance
Fatigue and exercise intolerance are common too. Your heart can’t pump blood well, making you feel very tired. This can happen even after doing a little bit of work.
Shortness of Breath and Dyspnea
Shortness of breath or dyspnea can happen when you’re doing everyday things or even when you’re just sitting. It’s because your heart can’t pump enough blood. This causes fluid to build up in your lungs.
When Symptoms Require Immediate Medical Attention
Knowing when to get help right away is important. Severe chest pain, trouble breathing, or fainting are signs to get emergency care. These could mean your condition is getting worse or you have a serious heart problem.
It’s important to listen to your body and get help when you need it. Don’t wait.
Diagnosis and Monitoring Protocols for Moderate Aortic Stenosis
Getting a correct diagnosis of moderate aortic stenosis is key. We use a mix of clinical checks, medical history, and advanced tests to spot and check the condition.
Initial Diagnostic Approaches and Tests
At first, we use non-invasive tests when we think of moderate aortic stenosis. These include a physical check-up, electrocardiogram (ECG), and chest X-ray. A heart murmur found during the physical check-up can hint at aortic stenosis.
Next, we do an echocardiogram. It gives us clear pictures of the heart’s shape and how it works. This test is vital for seeing how bad the aortic stenosis is by looking at the valve’s opening and blood flow.
The Role of Echocardiography in Diagnosis
Echocardiography is key in finding and keeping an eye on aortic stenosis. It lets us check the valve’s shape, how it works, and blood flow speed. This info helps us figure out how serious the stenosis is and what treatment is best.
We pick different echocardiography types, like TTE and TEE, based on what the patient needs and what we need to know.
Frequency and Importance of Regular Monitoring
Keeping an eye on aortic stenosis regularly is very important. We suggest regular echocardiograms to watch the valve’s changes and adjust treatment plans as needed.
How often to check depends on the patient’s situation and symptoms. Usually, those with moderate aortic stenosis should get an echocardiogram every 6 to 12 months.
Advanced Imaging Techniques for Assessment
Sometimes, we need more tests to look at the aortic valve and heart better. Cardiac MRI or CT scans give detailed pictures of the heart’s structure and function.
These advanced tests help us understand the disease better and plan the best treatment.
Treatment Options and Management Strategies
Managing moderate aortic stenosis needs a detailed plan. This includes both conservative management and, when needed, interventional treatments. We create treatment plans that fit each person’s health and needs.
Conservative Management Approaches
For patients with moderate aortic stenosis, conservative management is often the first step. This includes lifestyle modifications like eating well, exercising, and not smoking. We also keep a close eye on any changes in their condition.
Regular follow-ups are key to adjusting the treatment plan as needed. Our aim is to manage symptoms and slow the disease’s progression.
Medication Considerations and Limitations
There are no direct treatments for aortic stenosis, but we use drugs for related conditions like hypertension and heart failure. Beta-blockers and ACE inhibitors help reduce the heart’s workload.
But, it’s important to know the limits of medication for aortic stenosis. We focus on easing symptoms and treating other health issues.
Managing Underlying Conditions to Slow Progression
It’s key to manage underlying conditions to slow aortic stenosis’s progression. We stress controlling risk factors like high blood pressure, high cholesterol, and diabetes.
- Monitoring and managing hypertension
- Controlling cholesterol levels
- Managing diabetes effectively
By tackling these conditions, we can slow the disease’s progression and improve the patient’s life quality.
When to Consider Interventional Treatment
Deciding on interventional treatment depends on several factors. These include the severity of symptoms and the disease’s progression. We consider aortic valve replacement when symptoms significantly impact the patient’s life or when the disease progresses quickly.
Regular monitoring and assessment help determine the best time for interventional treatment. Our team works closely with patients to choose the best treatment based on their needs.
Aortic Valve Replacement: Surgical and Minimally Invasive Approaches
Choosing to have aortic valve replacement is a big decision for those with aortic stenosis. It’s important to think about the different surgical and minimally invasive options. Replacing the aortic valve is the best treatment for severe stenosis. It might also be an option for moderate cases in some cases.
SAVR and TAVR are both treatments for aortic stenosis. Each has its own benefits and when to use them depends on the patient’s health and stenosis severity.
Traditional Surgical Aortic Valve Replacement (SAVR)
SAVR is a long-standing procedure that involves open-heart surgery. It replaces the diseased valve with a prosthetic one. This method has been used for decades and offers excellent outcomes for many patients.
- Benefits: SAVR removes the diseased valve and replaces it with a prosthetic one. This can greatly improve heart function.
- Considerations: The procedure requires a sternotomy and cardiopulmonary bypass. This can lead to a longer recovery time.
Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a less invasive option compared to SAVR. It involves delivering a new valve through a catheter inserted into an artery, usually in the leg. This method is great for patients at high risk for surgery complications or who are considered inoperable.
- TAVR is less invasive, leading to fewer complications and a shorter hospital stay.
- The procedure is done under general anesthesia or conscious sedation, based on the patient’s condition and the operator’s preference.
Determining the Right Procedure for Individual Patients
Choosing between SAVR and TAVR requires a thorough evaluation of the patient’s condition. A heart team, including cardiologists and cardiac surgeons, decides the best treatment plan.
Key factors considered include:
- The severity of aortic stenosis
- The patient’s age and overall health status
- The presence of comorbid conditions
- The patient’s preferences and lifestyle
Recovery and Rehabilitation After Valve Replacement
Recovery after aortic valve replacement is critical. It requires careful monitoring and support. Patients usually go through a rehabilitation program to regain strength and improve heart health.
Key aspects of recovery include:
- Monitoring for possible complications
- Managing pain and discomfort
- Gradually increasing physical activity
- Adhering to prescribed medications
Living With Moderate Aortic Stenosis: Lifestyle Modifications and Daily Management
People with moderate aortic stenosis must make lifestyle changes to manage their condition well. We will look at key adjustments to keep the heart healthy and slow disease progression.
Physical Activity Recommendations and Limitations
Regular exercise is key for heart health. But, those with moderate aortic stenosis should talk to their doctor before starting or continuing any workout. Low to moderate intensity activities like brisk walking, swimming, or cycling are good choices.
Avoid high-intensity exercises that can strain the heart too much. It’s best to discuss your workout plan with your cardiologist to find the right activities for you.
Dietary Considerations for Heart Health
Eating a heart-healthy diet is important for managing aortic stenosis and heart health. Focus on eating a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats.
It’s also important to limit sodium. Too much sodium can cause fluid retention and high blood pressure, which can strain the heart.
| Dietary Component | Recommended Foods | Foods to Limit |
|---|---|---|
| Fruits and Vegetables | Berries, leafy greens, citrus fruits | Fruits canned in syrup, vegetables fried in oil |
| Proteins | Lean meats, fish, legumes | Processed meats, high-fat dairy products |
| Grains | Whole grains, oats, brown rice | Refined grains, sugary cereals |
Managing Comorbid Conditions
It’s important to manage conditions like hypertension, diabetes, and high cholesterol if you have moderate aortic stenosis. Work closely with your healthcare provider to control these conditions through medication, lifestyle changes, or a combination of both.
Psychological Aspects of Living With Valve Disease
Living with moderate aortic stenosis can affect your mental health, causing anxiety and depression. Seek support from mental health professionals, support groups, or counseling services to deal with these feelings.
Keeping a positive outlook and staying connected with loved ones can also help manage the emotional side of living with valve disease.
Conclusion: Navigating Your Heart Health Journey With Moderate Aortic Stenosis
Managing heart health with moderate aortic stenosis needs a full plan. This includes medical care, lifestyle changes, and keeping an eye on your health. We’ve looked at the key facts, signs, and treatment choices for this condition. It’s vital to know and handle moderate aortic stenosis to keep your heart in good shape.
Good management mixes medical care with lifestyle changes. With the help of doctors, people with moderate aortic stenosis can live full and active lives. It’s important to watch your health closely and get the right treatment to slow the disease and improve your life.
Handling moderate aortic stenosis as part of a bigger heart health plan lets people take charge of their health. By making smart choices about their care and living a healthy lifestyle, people can get the best results for their heart health. This also helps lower the chance of serious problems.
What is moderate aortic stenosis, and how is it diagnosed?
Moderate aortic stenosis is when the aortic valve opening narrows. This can slow blood flow from the heart. Doctors use echocardiography to check this. They look at how fast blood moves and the size of the valve.
What are the common symptoms of moderate aortic stenosis?
Symptoms include chest pain and feeling tired during activity. You might also have trouble breathing or feel short of breath. It’s important to notice these signs early.
How is moderate aortic stenosis treated, and what are the management strategies?
Treatment can be lifestyle changes or medicine. In some cases, a new valve is needed. It’s key to manage other health issues to slow the disease.
What is the difference between traditional surgical aortic valve replacement (SAVR) and transcatheter aortic valve replacement (TAVR)?
SAVR is open-heart surgery. TAVR is a less invasive procedure. The choice depends on the patient’s health and the disease’s severity.
How can individuals with moderate aortic stenosis manage their condition and maintain heart health?
Making lifestyle changes is important. This includes staying active, eating right, and managing other health issues. Regular check-ups are also key.
What are the echocardiographic criteria used to define moderate aortic stenosis?
Doctors use echocardiography to check blood flow and valve size. These help tell if the stenosis is mild, moderate, or severe. This is important for choosing the right treatment.
Can moderate aortic stenosis be managed without surgery?
Yes, it can be managed with lifestyle changes and medicine. But, sometimes surgery is needed to avoid serious problems.
How often should individuals with moderate aortic stenosis undergo follow-up assessments?
Follow-up visits depend on the patient’s health and how severe the stenosis is. Regular checks are important for managing the condition well.
References
American Heart Association (AHA): Managing Aortic Stenosis Symptoms
PubMed Central (NCBI): Genomic and Metabolic Risk Factors for Aortic Stenosis (Specific PMC ID)
American Academy of Family Physicians (AAFP): Aortic Stenosis (Journal Article)





