Last Updated on November 27, 2025 by Bilal Hasdemir
ut the Most Common Sites
Knowing where meningioma tumors usually grow is key for quick diagnosis and good treatment. At Liv Hospital, we focus on top-notch care and making sure each patient feels valued. We offer trusted care to people from all over.
Meningiomas are the top type of tumor in the brain and spine. They make up 37-39 percent of all such tumors. Knowing where these tumors often grow can really help patients.
We believe in the power of knowing and learning about meningiomas. Our goal is to give our patients the best care and support. We help international patients find the advanced medical treatments they need.
Key Takeaways
- Meningiomas are the most common primary central nervous system tumors.
- Understanding common locations is key for diagnosis and treatment.
- Liv Hospital provides patient-centered care with a focus on clinical excellence.
- Awareness and education are key to improving patient outcomes.
- Comprehensive care and support are available for international patients.
What You Need to Know About Meningioma Tumors
Meningiomas are slow-growing tumors that start in the meninges. These are protective membranes around the brain and spinal cord. Most are non-cancerous, but their location can affect health and life quality.
Definition and Basic Characteristics
Meningioma tumors start in the meninges, which have three layers. Most come from the arachnoid mater. They can grow at different rates, sometimes causing symptoms, other times not.
The World Health Organization (WHO) sorts meningiomas into three grades. Grade I is the most common and rarely comes back. Grades II and III are more aggressive and more likely to return.
Prevalence as Primary Central Nervous System Tumors (37-39%)
Meningiomas are the most common CNS tumors, making up 37-39% of primary brain tumors. This shows how important it is to know about meningioma tumors. It’s key for both patients and doctors.
More people get meningiomas as they get older, usually between 40 and 70. Women are more likely to get them than men, in some age groups. Knowing this helps with early detection and treatment.
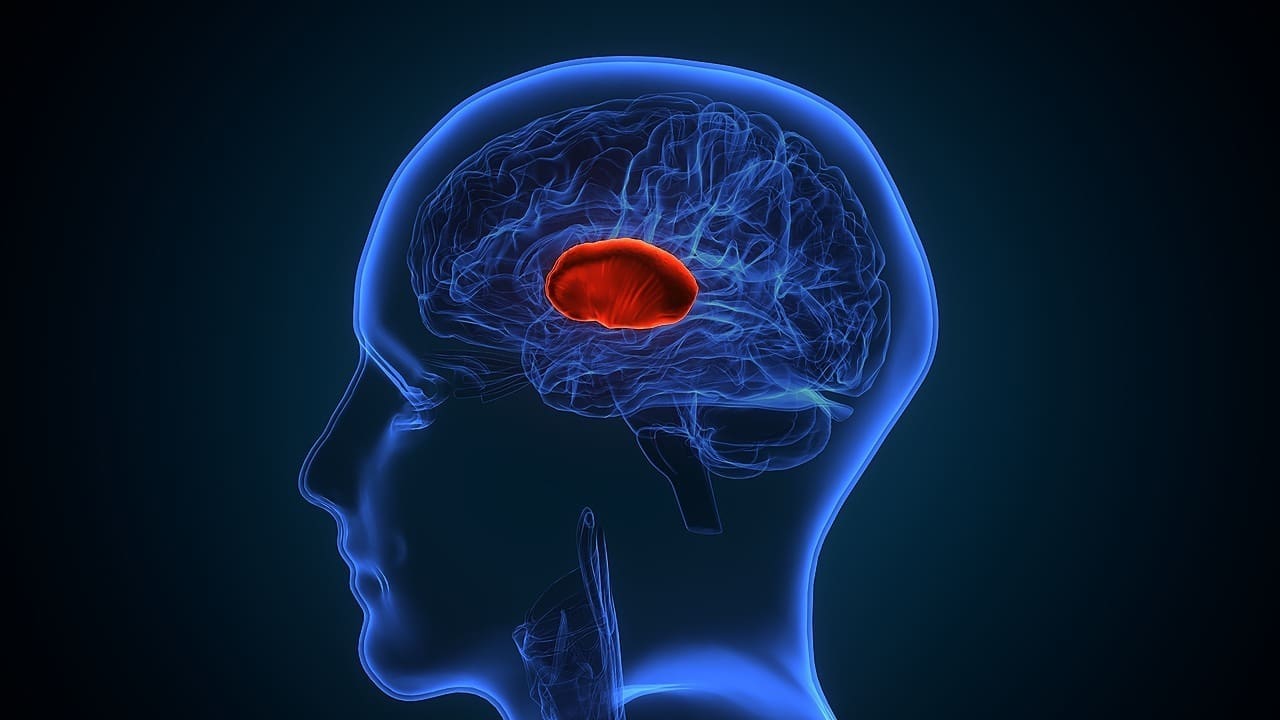
Key Fact #1: The Convexity of the Brain is the Most Common Meningioma Tumor Location

The brain’s outer surface, known as the convexity, is where meningioma tumors often grow. This is true, most often, in the left frontal area. Knowing this is key for doctors to diagnose and treat these tumors.
Understanding Brain Convexity
The brain’s convexity is its outer layer, touching the skull. It’s a common spot for meningiomas because it’s close to the meninges. These are protective membranes around the brain and spinal cord.
The shape and structure of the brain’s convexity are important for meningioma growth. The left frontal area is a major concern because it’s where many meningiomas start.
Left Frontal Convexity: Primary Site (20-37% of Cases)
Research shows that 20-37% of meningiomas start in the left frontal convexity. This makes it a critical area for doctors to study and understand.
This area is not just common for meningiomas. It’s also important because tumors here can affect brain function and movement.
Clinical Significance of Convexity Meningiomas
Convexity meningiomas can cause various neurological symptoms. This depends on the tumor’s size and where it is. Finding and treating them early is vital to avoid lasting harm.
Managing convexity meningiomas requires a team effort. Doctors need to look at the tumor and the patient’s health as a whole.
Key Fact #2: Posterior Fossa Meningiomas Present Unique Challenges
Meningiomas in the posterior fossa are hard to diagnose and treat. This area is complex and has important parts like the brainstem and cerebellum. Tumors here are tricky because they’re close to these key structures.
Prevalence of Posterior Fossa Meningiomas
These tumors make up about 6-15% of meningioma cases. Even though they’re not common, they need special care because of their effect on nearby brain parts
A well-known neurosurgeon, says, “Handling posterior fossa meningiomas needs a deep grasp of the area’s anatomy. It also requires a team effort for treatment.”
Distinctive Symptoms and Presentation
The symptoms of these tumors vary based on their size and location. Common signs include:
- Balance and coordination problems
- Speech and swallowing issues
- Hearing loss or tinnitus
- Headaches and nausea
At first, these symptoms might be mild, making it hard to catch the tumor early. But as it grows, it can press on important parts, causing serious brain problems.
Treatment Complexities in This Region
Dealing with these tumors is tricky because of the sensitive areas around them. Surgery is often needed, but it must be done carefully to protect the brain.
“The surgical management of posterior fossa meningiomas is one of the most challenging tasks in neurosurgery, requiring a high degree of skill and experience.” –
We use the latest imaging and monitoring during surgery to help our patients. Sometimes, we also suggest radiation therapy, either alone or with surgery.
Key Fact #3: Other Critical Meningioma Locations and Their Impact
Meningiomas can happen in many important places, not just the usual ones. We’ll look at areas like the parasagittal and falx regions, sphenoid ridge, olfactory groove, and the spine. Each has its own special features and how they affect patients.
Parasagittal and Falx Meningiomas
Parasagittal and falx meningiomas are close to key brain parts. They grow near the falx cerebri, a part that divides the brain’s hemispheres. Symptoms can include headaches, seizures, and cognitive changes, based on the tumor’s size and where it is.
These tumors are tricky because they can harm the brain around them. Doctors usually remove them surgically, being very careful of nearby structures.
Sphenoid Ridge and Olfactory Groove Meningiomas
Sphenoid ridge and olfactory groove meningiomas are special challenges. Sphenoid ridge meningiomas can mess with vision and eye movement because of their close location to the optic nerve and cavernous sinus. Olfactory groove meningiomas can cause loss of smell and other brain problems.
Treating these tumors often needs a team effort from neurosurgery, radiation oncology, and more. High-tech imaging is key for planning and doing the treatment.
Spinal Meningiomas: Often Overlooked
Spinal meningiomas are rare but can really affect a person’s life. They often show up in the thoracic area and can cause back pain, weakness, and other nerve issues.
Getting a correct diagnosis and treating them quickly is very important. Surgery is usually the main treatment, and it often works well.
| Location | Common Symptoms | Treatment Approaches |
|---|---|---|
| Parasagittal and Falx | Headaches, seizures, cognitive changes | Surgical resection, consideration of adjacent structures |
| Sphenoid Ridge | Vision changes, eye movement disturbances | Multidisciplinary approach, including surgery and radiation |
| Olfactory Groove | Loss of smell, neurological deficits | Advanced imaging, surgical planning, potentially radiation |
| Spinal | Back pain, weakness, sensory disturbances | Surgical removal |
Key Fact #4: How Meningioma Tumor Location Affects Symptoms
Knowing how meningioma location affects symptoms is key for correct diagnosis and treatment. The spot where a meningioma grows greatly impacts symptoms. This is because different parts of the brain and spinal cord handle different functions.
Location-Specific Neurological Manifestations
Meningiomas in different spots can lead to various neurological symptoms. For example, those near the optic nerve can cause vision issues like double vision or loss of side vision. Meningiomas near motor control areas can lead to weakness or paralysis in certain limbs.
On the other hand, meningiomas in quiet brain spots might not show symptoms until they grow big enough to press on nearby areas. This shows why detailed diagnostic checks are so important.
When Symptoms Might Be Subtle or Absent
In some cases, meningiomas can grow big before causing noticeable symptoms, if they’re in quiet brain spots. These “silent” meningiomas might only be found by chance during scans for other reasons.
But, even if symptoms are mild or not there, it’s important to keep an eye on them. This is to catch any signs of growth or other problems.
Red Flags That Warrant Immediate Medical Attention
Certain symptoms need quick medical check-ups, even with a known meningioma. Sudden severe headaches, seizures, or big changes in vision or movement are urgent signs. They mean you need to see a doctor right away.
Also, if symptoms get worse over time, you should get medical advice. This could mean the tumor is growing or there’s another issue that needs help.
Key Fact #5: Diagnostic Approaches Vary by Location
Diagnosing meningiomas isn’t the same for every tumor. It changes a lot based on where the tumor is in the brain or spine. This is because different areas are easier or harder to see and reach.
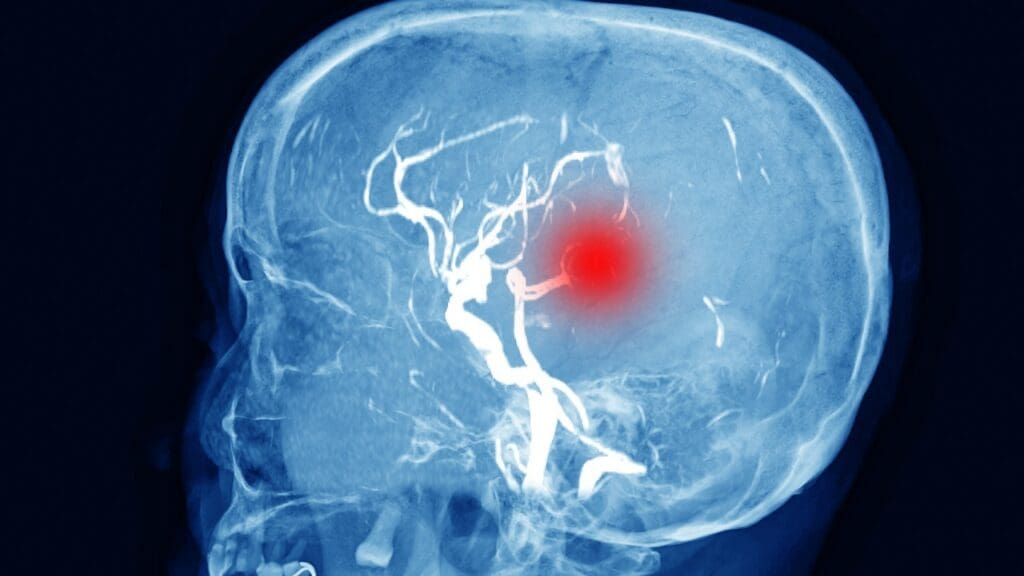
Advanced Imaging Techniques for Different Locations
MRI (Magnetic Resonance Imaging) is key for spotting meningiomas. It’s great because it shows soft tissues well. For tumors near important parts, like the back of the brain or big blood vessels, MR Angiography helps a lot.
When it comes to the spine, CT (Computed Tomography) scans are helpful. They’re good for seeing how tumors affect bones. Doctors pick between MRI and CT scans based on where the tumor is and what they need to plan treatment.
The Role of Biopsy in Diagnosis
Even with imaging, a biopsy is the best way to confirm meningiomas. It takes a piece of the tumor for lab tests. Whether to do a biopsy depends on where the tumor is and the risks.
For tumors that are easy to get to, a biopsy is simple. But for hard-to-reach ones, the risks might be too high. Then, doctors rely more on what imaging shows.
Differentiating Meningiomas from Other Brain Tumors
Telling meningiomas apart from other brain tumors is important for treatment. Meningiomas have special signs on MRI, like a dural tail. MR Spectroscopy can also give clues about the tumor’s makeup.
In short, finding meningiomas needs a plan based on where they are. Using advanced imaging, careful checks, and sometimes biopsy, doctors can accurately diagnose and treat meningiomas.
Key Fact #6: Treatment Strategies Depend on Tumor Location
Treatment for meningioma changes based on where the tumor is in the brain or spine. Different locations mean different treatments, like surgery or radiation. Sometimes, doctors just watch and wait.
Surgical Accessibility Considerations
How easy it is to get to the tumor is key in planning treatment. Tumors in easy-to-reach spots, like the brain’s outer surface, are simpler to remove. But tumors in tricky spots, like the back of the brain or the skull base, are harder.
Surgical Challenges by Location:
| Tumor Location | Surgical Challenges |
|---|---|
| Convexity | Generally accessible, but size and adherence to brain surface can complicate removal. |
| Posterior Fossa | Difficult due to proximity to critical brainstem structures. |
| Base of Skull | Complex anatomy and proximity to vital structures complicate surgery. |
Radiation Therapy Options for Different Locations
Radiation therapy is a good choice for meningiomas that can’t be fully removed or are in hard-to-reach spots. The type of radiation used depends on the tumor’s size and where it is.
Radiation Therapy Techniques:
- Stereotactic radiosurgery (SRS) for precise targeting of small to medium-sized tumors.
- Fractionated stereotactic radiotherapy (FSRT) for larger tumors or those near critical structures.
When Watchful Waiting Is Appropriate
Not every meningioma needs to be treated right away. Small, harmless tumors in older patients or those with health issues might just be watched. This means regular checks to see if the tumor grows.
Every patient is different, and the decision to wait and watch is made carefully. Doctors consider the tumor’s size, location, and the patient’s health.
Key Fact #7: Understanding Meningioma Terminology and Variants
It’s important for patients to know the terms related to meningiomas. These tumors are the most common in the brain. Knowing the different terms helps patients and doctors talk clearly and understand each other.
Common Spelling Variations
People sometimes spell meningiomas differently, like “menigiomas” or “maningioma.” These changes come from different sources, like old words or typing mistakes. Knowing these variations helps when looking up information or talking to doctors.
Medical Terminology Explained
Medical words for meningiomas tell us where they are, how serious they are, and what kind they are. For example, “convexity meningioma” tells us where in the brain it is. Knowing these words helps patients understand their diagnosis and treatment.
Key terms include:
- Meningioma grade: Shows how serious the tumor is, with Grade I being the least serious and Grade III being the most.
- Location-specific terms: Like “sphenoid wing meningioma” or “olfactory groove meningioma,” which tell us where the tumor is.
Why Accurate Terminology Matters for Patient Education
Using the right words is key for patient education. It helps patients understand their diagnosis and treatment. If the words are not clear, patients might get confused or worried. Doctors need to explain these terms well so patients can make informed choices.
“Clear communication about meningioma diagnosis and treatment options is essential for patient-centered care.” – Expert in Neuro-Oncology
By learning about meningioma terms, patients can better understand their care. They can make smarter choices and work better with their healthcare team.
Excellence in Meningioma Treatment: Multidisciplinary Approaches
At Liv Hospital, we aim for the best in diagnosing and treating meningiomas. We use the latest methods and work together as a team. This ensures our patients get the best care.
Specialized Care Centers
Specialized care centers are key for meningioma treatment. They have the latest technology and teams with lots of experience. This focus on expertise leads to better results for patients.
Benefits of Specialized Care Centers:
- Access to advanced diagnostic and treatment modalities
- Multidisciplinary teams with specialized expertise
- Participation in clinical trials and research studies
- Standardized care protocols based on the latest evidence
Liv Hospital’s Protocols and Patient Outcomes
Liv Hospital is dedicated to top-notch care for meningioma patients. We create a treatment plan for each patient. This plan is made by a team of experts.
| Treatment Approach | Patient Outcomes |
|---|---|
| Surgical resection | High success rate with minimal complications |
| Radiation therapy | Precise targeting with advanced technology |
| Watchful waiting | Regular monitoring to ensure timely intervention |
A leading expert says, “The key to treating meningiomas is teamwork. Neurosurgeons, radiation oncologists, and others work together for the best care.”
“The use of new diagnostic tools and treatments has changed meningioma care. It gives hope to patients all over the world.”
Latest Advances in Location-Specific Treatments
Treatment for meningiomas has improved a lot. This is thanks to new location-specific therapies. For example, treatments for convexity and posterior fossa meningiomas are more precise now.
Our team keeps up with these new developments. We use the latest research and technology in our care. This means our patients get the best treatment available.
Conclusion: Navigating Meningioma Diagnosis and Treatment
Understanding meningioma diagnosis and treatment is key. We’ve looked at where meningioma tumors usually grow. This knowledge helps doctors diagnose and treat better.
The spot where a meningioma grows affects symptoms and treatment. At Liv Hospital, we use the latest imaging and team work to help patients. This approach ensures top-notch care for meningioma patients.
If you have a meningioma diagnosis, getting help from experts is vital. We offer full support to international patients. By grasping the details of meningioma care, we can achieve the best results together.
FAQ
What is the most common location for meningioma tumors?
Meningioma tumors most often occur in the brain’s left frontal area. This location makes up 20-37% of all cases.
What are posterior fossa meningiomas, and how common are they?
Posterior fossa meningiomas are found in the brain’s back part. They make up 6-15% of meningioma cases. Their location makes treatment challenging.
What are the symptoms of meningioma, and how do they vary by location?
Symptoms of meningioma depend on where the tumor is. Some symptoms might be specific to the location. Look out for severe headaches, seizures, and any neurological issues.
How are meningiomas diagnosed, and what diagnostic approaches are used?
Diagnosing meningiomas involves different methods based on the tumor’s location. MRI and CT scans are often used. A biopsy might also be needed to confirm the diagnosis.
What are the treatment options for meningiomas, and how do they depend on tumor location?
Treatment for meningiomas depends on the tumor’s location. Options include surgery, radiation therapy, or monitoring. The choice depends on how easily the tumor can be reached and the best radiation therapy.
What are some common spelling variations of the term “meningioma”?
“Meningioma” is often misspelled in many ways. Some common errors include meningiomi, meninjioma, and menangioma. Other variations include meninggioma, meniingioma, and meninginoma.
Why is accurate terminology important for patient education and awareness?
Using the right words is key for patient education. It helps ensure clear communication between doctors and patients. Knowing the correct terms helps patients understand their condition and treatment.
What is the significance of specialized care centers in treating meningiomas?
Specialized care centers are vital for meningioma treatment. They offer tailored treatments and care. Places like Liv Hospital have specific protocols for meningioma patients.