Last Updated on November 27, 2025 by Bilal Hasdemir

Aortic stenosis is a serious condition that affects many adults over 65. It’s found in up to 9% of this age group. Knowing the treatment options is key to managing it well.
At Liv Hospital, we focus on patient-centered care. We use the latest medical evidence and international standards. Our treatment for aortic stenosis includes a detailed look at the newest medical treatments and procedures.
We keep up with the latest in aortic stenosis management. This guide will show you the current medical options for treating this condition.
Key Takeaways
- Understanding the prevalence and impact of aortic stenosis on adults over 65.
- Overview of the current medical treatments available for aortic stenosis.
- The role of Liv Hospital in providing patient-centered care for aortic stenosis.
- Importance of staying updated with the latest advancements in aortic stenosis management.
- Comprehensive evaluation of treatment options for effective management.
Understanding Aortic Stenosis: A Progressive Valve Condition

It’s important to understand aortic stenosis to manage its progression. This condition makes the aortic valve narrow. This narrowing blocks blood flow from the heart to the rest of the body.
What Happens in Aortic Stenosis
The narrowing of the valve is usually due to calcification. Calcium builds up on the valve, making it stiff. This makes it hard for the valve to open fully. The heart then has to work harder, which can lead to thickening of the heart muscle and reduced function over time.
Prevalence and Risk Factors
Aortic stenosis is more common in older adults. It becomes more prevalent with age. Risk factors include congenital heart defects, age-related wear and tear, and a history of rheumatic fever.
Other factors like high blood pressure, high cholesterol, and smoking also increase the risk. These factors contribute to the development of aortic stenosis.
Symptoms and Disease Progression
Symptoms of aortic stenosis include chest pain, fainting, and shortness of breath. As the condition gets worse, these symptoms can get worse too. If left untreated, it can lead to heart failure.
Early detection and management are key. They help slow down the disease’s progression and improve outcomes for patients.
The Limitations of Medical Therapy in Aortic Stenosis

Medical therapy for aortic stenosis has made progress, but it’s not perfect. Aortic stenosis is a condition where the aortic valve gets narrower. Current medicines can help manage symptoms but can’t stop the disease from getting worse.
Why Medications Cannot Reverse Valve Narrowing
Medicines for aortic stenosis aim to ease symptoms like chest pain and shortness of breath. But they can’t fix the main problem: the narrowing of the aortic valve. This narrowing is caused by calcification and fibrosis, which can’t be reversed by today’s medicines.
Goals of Medical Management
The main goals of medical treatment for aortic stenosis are to ease symptoms and improve life quality. Doctors tailor treatment plans based on each patient’s needs. They consider how severe symptoms are and any other heart risks.
Importance of Symptom Control
Managing symptoms is key in treating aortic stenosis. It not only makes patients feel better but also helps track how the disease is progressing. Below is a table that highlights the importance of symptom control.
| Symptom | Management Strategy | Benefit |
|---|---|---|
| Chest Pain (Angina) | Beta-blockers, Nitrates | Reduces myocardial oxygen demand |
| Shortness of Breath | Diuretics | Reduces fluid overload |
| Fatigue | Optimization of heart failure medications | Improves cardiac output |
By knowing the limits of medical therapy and focusing on symptom control, doctors can give the best care to patients with aortic stenosis.
Drugs for Aortic Stenosis: Symptom Management Approach
The main goal of drug therapy for aortic stenosis is to ease symptoms and enhance life quality. Medications can’t fix the valve issue, but they’re key in managing symptoms and bettering patient results.
Diuretics for Fluid Overload
Diuretics are used to handle fluid overload in aortic stenosis patients. They help reduce fluid, easing symptoms like shortness of breath and tiredness. For more on managing aortic stenosis symptoms, check out the American Heart Association’s guide.
Beta-Blockers: Benefits and Limitations
Beta-blockers are used in aortic stenosis management. They control heart rate and lessen heart workload. But, their use needs careful watch, as they might worsen symptoms in some by reducing heart compensation.
Antihypertensive Medications
Antihypertensive meds are for high blood pressure in aortic stenosis patients. Keeping blood pressure in check is vital for disease progression and heart health. The right medication depends on the patient’s specific situation and other health issues.
Understanding these medications helps doctors create a detailed treatment plan. This plan aims to manage symptoms and improve life quality for those with aortic stenosis.
ACE Inhibitors and ARBs in Aortic Stenosis Management
ACE inhibitors and ARBs are useful for managing symptoms in aortic stenosis patients. They are mainly used for high blood pressure and heart failure. But, they also play a role in aortic stenosis care.
Appropriate Use of ACE Inhibitors
ACE inhibitors are used with caution in aortic stenosis, mainly in severe cases. They are helpful for those with high blood pressure or heart failure. Starting with low doses and watching for signs of low blood pressure or kidney problems is key.
Precautions and Monitoring
Monitoring is critical when using ACE inhibitors or ARBs for aortic stenosis. We check kidney function, electrolytes, and blood pressure regularly. Regular check-ups help adjust treatment plans as needed.
Benefits for Coexisting Conditions
ACE inhibitors and ARBs help with conditions like high blood pressure, heart failure, or diabetes. They improve patient outcomes and quality of life. Benefits include:
- Lowering blood pressure
- Slowing heart failure
- Protecting the kidneys
Statins and Lipid-Lowering Therapy
Statins are often given to lower heart risk in patients with heart issues, like aortic stenosis. We look into their part in managing this serious valve problem.
Research on Statins in Aortic Stenosis
Many studies have looked into statins’ benefits for aortic stenosis patients. Statins are good at lowering cholesterol, but their effect on aortic stenosis is debated.
A meta-analysis of trials showed statins don’t slow aortic stenosis much. But, they do lower heart event risks.
Cardiovascular Risk Reduction
Patients with aortic stenosis often have other heart issues. Statins are key in managing these by lowering LDL cholesterol and heart risk.
Current Guidelines for Statin Use
Guidelines suggest statins for aortic stenosis patients at high or moderate heart risk. Starting statins depends on the patient’s risk level.
| Guideline | Recommendation |
|---|---|
| ACC/AHA Guidelines | Statin therapy is recommended for patients with aortic stenosis who have high or moderate cardiovascular risk. |
| ESC Guidelines | Statins are recommended for patients with aortic stenosis and high cardiovascular risk. |
Looking into statins’ role in aortic stenosis, they help heart health even if they don’t stop valve narrowing.
Managing Heart Failure Symptoms in Aortic Stenosis Patients
Heart failure is a big problem for people with aortic stenosis. It makes them short of breath, tired, and swollen. We must manage these symptoms well to help them feel better.
Recognizing Heart Failure in Aortic Stenosis
We look for signs of heart failure in aortic stenosis patients. Key indicators include trouble breathing when active, needing to breathe while lying down, and sudden shortness of breath at night. Watching for these signs helps us act fast.
Medication Adjustments for Heart Failure
Changing medications is key in treating heart failure in aortic stenosis. We use diuretics to get rid of extra fluid. ACE inhibitors or ARBs help lower blood pressure. It’s important to adjust these medicines carefully to keep the heart working right.
Balancing Cardiac Output and Preload
It’s important to balance the heart’s output and preload. We want to keep the preload right while making sure the heart pumps enough. Here’s how we do it:
| Parameter | Goal | Intervention |
|---|---|---|
| Cardiac Output | Maintain adequate CO | Inotropes or vasodilators |
| Preload | Optimize preload | Diuretics or fluid resuscitation |
By managing heart failure symptoms and adjusting medicines, we can make aortic stenosis patients’ lives better.
Medical Management for Mild Aortic Stenosis
Patients with mild aortic stenosis often follow a conservative management plan. This plan involves watching the condition closely and managing symptoms. It avoids immediate surgery.
Conservative Approach for Asymptomatic Patients
Patients without symptoms are closely monitored. Regular echocardiograms track the valve’s narrowing. Early detection of symptoms or disease progression helps adjust treatment plans.
Risk Factor Modification
Changing risk factors is key in managing mild aortic stenosis. We suggest lifestyle changes like a healthy diet and exercise. Quitting smoking is also important. Managing high blood pressure and cholesterol is vital.
Activity Recommendations and Restrictions
We advise an active lifestyle for patients with mild aortic stenosis. Moderate exercise is best. It keeps the heart healthy without too much strain.
When Drugs Are Not Enough: Indicators for Intervention
When aortic stenosis symptoms don’t improve with medicine, it’s time for more action. We watch how well patients with aortic stenosis do with their treatment closely.
Symptom Progression Despite Medical Therapy
Even with the best medicine, aortic stenosis symptoms can get worse. Symptoms like chest pain, shortness of breath, and fatigue can get more severe. This means we need to change the treatment plan.
Echocardiographic Markers of Severe Disease
Echocardiography is key in figuring out how bad aortic stenosis is. Echocardiographic markers like valve area and mean gradient show how severe it is. If these markers show severe disease, we need to think about more than just medicine.
Risk Stratification for Intervention
Figuring out who needs intervention is important. We look at clinical assessment, echocardiography, and other tests to decide. This helps us find out who needs surgery or a new valve.
By watching symptoms, echocardiographic markers, and risk, we find the best time for treatment. This way, patients get the right care for their aortic stenosis.
Surgical Aortic Valve Replacement: The Gold Standard
For those with severe aortic stenosis, surgical aortic valve replacement is the top choice. This method replaces the old valve with a new one. It boosts the heart’s function and overall health.
Types of Surgical Valves
There are different types of surgical valves. Mechanical valves last long but need lifelong blood thinner use. Bioprosthetic valves, made from animal tissue, have less clot risk but may need replacing sooner.
Surgical Approach and Techniques
Surgical methods for aortic valve replacement have improved. The old way was a big chest cut. Now, minimally invasive techniques use smaller cuts for quicker healing.
Recovery and Rehabilitation
Recovering from this surgery needs careful watching and rehab. Patients often stay in the hospital for days. They may need weeks to fully get better. A good rehab plan can help and lower risks.
Long-term Outcomes and Medication Requirements
The results of this surgery are usually good, with better symptoms and life expectancy. But, patients might need ongoing meds. The type of valve and the patient’s health affect long-term needs.
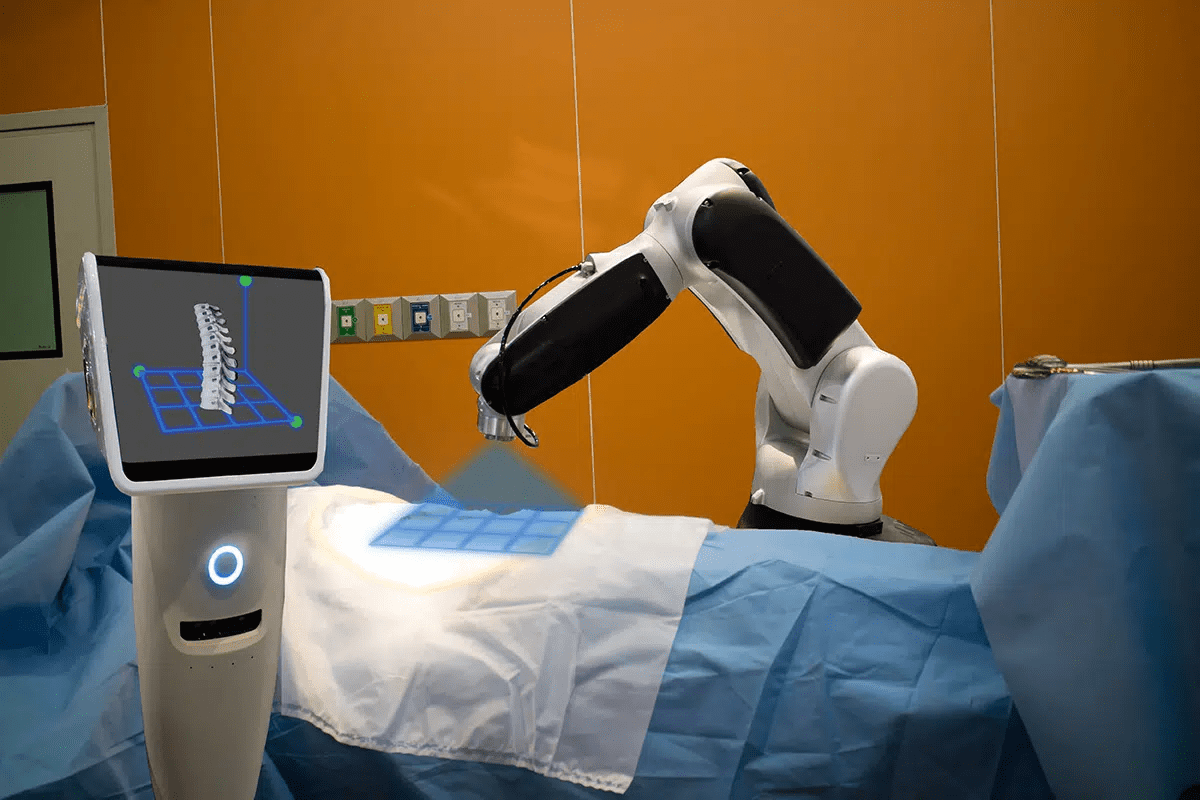
Transcatheter Aortic Valve Implantation (TAVI): Minimally Invasive Option
Transcatheter Aortic Valve Implantation (TAVI) has changed how we treat aortic stenosis. It’s a less invasive option for some patients. It’s great for those at high risk for surgery or who can’t have traditional surgery.
Patient Selection for TAVI
Choosing the right patient for TAVI is key. We look at the patient’s health, how severe their aortic stenosis is, and any other health issues. We use tests like echocardiography and CT scans to decide if TAVI is right for them.
Procedure Overview
The TAVI procedure uses a small incision, usually in the groin or chest. A catheter is inserted to put in a new valve. The new valve opens, improving blood flow. The whole thing is done under general anesthesia or sedation, depending on the patient.
Advantages Over Traditional Surgery
TAVI has big advantages over traditional surgery. It’s safer, with less pain and a quicker recovery. This makes TAVI a good choice for those at high risk for surgery.
Post-Procedure Medication Protocol
After TAVI, patients take antiplatelet therapy to prevent clots. The type and length of treatment depend on the valve and patient’s risk. We watch patients closely to adjust their meds and handle any issues.
Special Considerations in Aortic Stenosis Treatment
When we talk about treating aortic stenosis, we must think about special needs. Not all patients are the same, and treatment plans need to be tailored. This is true for elderly patients, those with many health issues, and pregnant women.
Elderly Patients and Frailty Assessment
Elderly patients face unique challenges with aortic stenosis. It’s important to assess their frailty to choose the right treatment. Frailty assessment tools help doctors pick the best option for each patient.
A study in the Journal of the American College of Cardiology showed frailty’s impact. It found that frailty increases the risk of death and poor outcomes after TAVI.
Managing Comorbidities
Patients with aortic stenosis often have other health issues. It’s key to manage these conditions well to improve outcomes.
| Comorbidity | Management Strategy |
|---|---|
| Hypertension | Antihypertensive medications, lifestyle modifications |
| Diabetes | Glycemic control through medication and lifestyle changes |
| Coronary Artery Disease | Antiplatelet therapy, revascularization when necessary |
Pregnancy and Aortic Stenosis
Pregnancy is risky for women with aortic stenosis. It’s important to plan and manage care carefully.
Medication Safety During Pregnancy
Choosing the right medications for aortic stenosis during pregnancy is critical. Beta-blockers are used, but they need close monitoring.
“The management of aortic stenosis in pregnancy requires a multidisciplinary approach, involving cardiologists, obstetricians, and other specialists to ensure the best possible outcomes.”
Delivery Planning
Planning for delivery in women with aortic stenosis is detailed. Vaginal delivery is preferred, but sometimes a cesarean section is needed.
Conclusion: Integrated Approach to Aortic Stenosis Treatment
We’ve looked into aortic stenosis, a serious valve problem. It needs a mix of treatments to manage it well. This includes medicine, lifestyle changes, and sometimes surgery.
Using a team approach is vital for better results. Doctors use drugs to ease symptoms and help patients change their lifestyle. They also consider surgery or a new valve when needed. This way, care fits each patient’s needs, improving their life and chances of living longer.
With a detailed plan, we can better help those with aortic stenosis. This plan covers their physical and emotional health. It’s essential for giving top-notch care that focuses on the patient.
FAQ
What is aortic stenosis and how does it affect the heart?
Aortic stenosis is a condition where the aortic valve gets narrower. This blocks blood flow from the heart. Symptoms include chest pain, shortness of breath, and feeling tired.
What are the primary goals of medical management for aortic stenosis?
The main goals are to control symptoms and improve life quality. Doctors use medicines to help, but they can’t fix the valve narrowing.
What medications are used to manage symptoms of aortic stenosis?
Diuretics help with fluid buildup. Beta-blockers control heart rate. Antihypertensive meds manage blood pressure. ACE inhibitors and ARBs are used with caution.
Can statins help in the treatment of aortic stenosis?
Statins help lower heart risk. But their role in treating aortic stenosis is being studied. Current guidelines suggest using them for heart risk reduction.
How is heart failure managed in patients with aortic stenosis?
Heart failure symptoms are managed with medication. This balances heart output and preload. Diuretics, vasodilators, and other meds are used.
What is the conservative management approach for asymptomatic patients with mild aortic stenosis?
Patients with mild aortic stenosis are managed with lifestyle changes and monitoring. This approach aims to prevent disease worsening and manage other conditions.
When is surgical intervention necessary for aortic stenosis?
Surgery is needed when symptoms worsen despite medicine, or if echocardiograms show severe disease. Risk assessment determines the need for surgery.
What are the surgical options for treating aortic stenosis?
The best option is surgical valve replacement. For some, a minimally invasive TAVI is available.
What are the special considerations in treating aortic stenosis in elderly patients?
Elderly patients need careful management of their health. Treatment plans are tailored to their overall health and life expectancy.
How is aortic stenosis managed during pregnancy?
Pregnancy with aortic stenosis requires close monitoring. Treatment is tailored to the patient’s risk and symptoms.
What is the role of Liv Hospital in treating aortic stenosis?
Liv Hospital offers modern care for aortic stenosis. We provide various treatments, including surgery and minimally invasive options. Our team creates personalized plans for each patient.
What is the importance of an integrated approach to treating aortic stenosis?
An integrated approach combines medicine, lifestyle changes, and surgery as needed. This strategy aims to improve patient outcomes and quality of life.
References
-
- AAFP (Aortic Stenosis) : https://www.aafp.org/pubs/afp/issues/2016/0301/p371.html
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC7729185