Last Updated on November 27, 2025 by Bilal Hasdemir

At Liv Hospital, we know how vital accurate diagnosis is for treating heart issues. Aortic stenosis is a heart disease where the aortic valve gets narrower. This blocks blood flow from the left ventricle to the aorta.
To diagnose severe aortic stenosis, we look at important values like the aortic valve area, mean pressure gradient, and peak velocity. Echocardiography is our main tool for checking how severe this condition is.
Knowing the 7 essential parameters is key for making treatment plans and better patient care. Our focus is on the patient, making sure every diagnosis meets global standards and keeps patients safe.
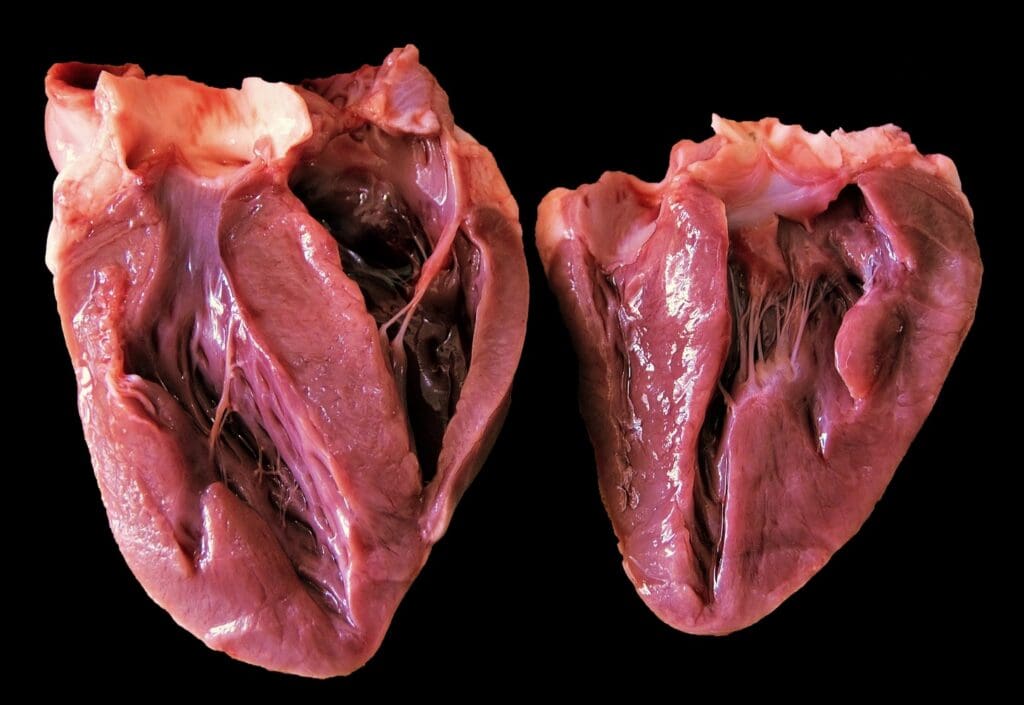
Aortic stenosis is a serious heart condition. It happens when the aortic valve gets narrower. This makes it harder for blood to flow and can lead to left ventricular hypertrophy.
The narrowing of the aortic valve is caused by calcification and fibrosis. This forces the heart to work harder to pump blood. If not treated, it can lead to heart failure. A study on NCBI shows that valvular calcification plays a big role in this process.
The progression of aortic stenosis varies from person to person. Some may stay symptom-free for years, while others experience quick worsening. Studies show that once symptoms appear, the disease can progress rapidly.
Knowing what affects disease progression is key. It helps doctors manage patients better and decide when to intervene.

To diagnose severe aortic stenosis, we use many echocardiographic parameters. We look at primary measurements and supporting findings. This helps us understand how severe the stenosis is.
Key measurements for severe aortic stenosis include aortic valve area (AVA), mean pressure gradient, and peak velocity. These tell us a lot about the stenosis’s severity.
Other echocardiographic findings help diagnose severe aortic stenosis. These include left ventricular function, valve morphology, and other hemodynamic parameters.
| Parameter | Value | Significance |
|---|---|---|
| Aortic Valve Area (AVA) | <1.0 cm² | Severe stenosis |
| Mean Pressure Gradient | >40 mmHg | Significant obstruction |
| Peak Velocity | >4.0 m/s | Severe stenosis |
As noted by
“The assessment of aortic stenosis severity is complex and requires integration of multiple echocardiographic parameters.”
— Baumgartner et al.
Diagnosing severe aortic stenosis follows guidelines from top cardiology groups. These rules have changed with new evidence and tech, helping doctors make accurate diagnoses and treatments.
How we diagnose severe aortic stenosis has changed a lot. At first, doctors looked for symptoms. But now, with better imaging, we also look at specific numbers like the valve area and pressure.
Both American and European cardiology groups have set rules for diagnosing severe aortic stenosis. They agree on the key role of echocardiography. This includes looking at the valve area, pressure gradient, and peak velocity.
| Parameter | American Guidelines | European Guidelines |
|---|---|---|
| Aortic Valve Area (cm²) | <1.0 | <1.0 |
| Mean Pressure Gradient (mmHg) | >40 | >40 |
| Peak Velocity (m/s) | >4.0 | >4.0 |
It’s key for doctors to know these guidelines to treat severe aortic stenosis well. By sticking to these rules, doctors can give patients the best care based on the latest research and expert advice.
Measuring the aortic valve area (AVA) is key to figuring out how severe aortic stenosis is. The AVA helps doctors decide on the best treatment. We’ll look at how to calculate AVA, why it matters, and what can go wrong.
The continuity equation is the main way to find AVA. It uses the blood flow speed through the valve and the left ventricle. The formula is: AVA = (LVOT area × LVOT VTI) / Aortic valve VTI. Getting the left ventricle’s size and blood flow right is important for a correct AVA.
Let’s say the left ventricle is 2.0 cm wide, its VTI is 20 cm, and the valve’s VTI is 100 cm. Then, AVA = (π × (2.0/2)² × 20) / 100 = 0.63 cm². This shows severe aortic stenosis.
| Parameter | Value | Unit |
|---|---|---|
| LVOT Diameter | 2.0 | cm |
| LVOT VTI | 20 | cm |
| Aortic Valve VTI | 100 | cm |
| AVA | 0.63 | cm² |
An AVA under 1.0 cm² means severe aortic stenosis. Many guidelines, like the European Society of Cardiology, agree. People with this AVA need careful watching and might need treatment.
“The assessment of aortic stenosis severity should be based on a complete evaluation, including symptoms, echocardiographic parameters, and other clinical findings.”
European Society of Cardiology Guidelines
There are many ways to mess up AVA measurements. Wrong left ventricle size, bad Doppler setup, and wrong angles are common mistakes. To avoid these, it’s vital to use the best imaging techniques and train sonographers well.
Knowing how to calculate AVA, its importance, and what can go wrong helps doctors better manage aortic stenosis patients.
The mean pressure gradient is key in checking how severe aortic stenosis is. It shows how much blood flow is blocked by the aortic valve.
A mean pressure gradient over 40 mmHg usually means severe aortic stenosis. This level is important because it shows a higher risk of serious problems like heart failure and death.
Clinical Implications: People with gradients over this level need to be watched closely. They might need surgery or a new valve put in.
The mean pressure gradient changes based on blood flow and heart function. So, it’s important to look at these factors when checking the gradient.
In cases where the heart doesn’t pump well, the gradient might seem lower. But, if there’s too much blood flow, the gradient can go up.
Getting the mean pressure gradient right is very important. It needs careful attention to detail. Doppler echocardiography is the main way to measure it.
Key Technical Considerations:
| Parameter | Normal/ Mild | Moderate | Severe |
|---|---|---|---|
| Mean Pressure Gradient (mmHg) | <20 | 20-40 | >40 |
| Clinical Implication | Monitoring | Close Monitoring | Intervention Considered |
In diagnosing severe aortic stenosis, peak velocity is key. It gives us vital info through Doppler echocardiography. We use this to check how severe the condition is and decide what to do next.
Velocities over 4.0 m/sec show severe aortic stenosis. This is a big deal because it means the valve is very narrow. This can lead to serious symptoms and even heart failure or death.
To get accurate peak velocity readings, we must align the Doppler right. Getting it right means the ultrasound beam and blood flow are almost in line. This helps avoid underestimating the peak velocity. We use different views to find the best signal.
The Velocity Time Integral (VTI) is also key. It shows the total blood flow over time. When looking at VTI with severe aortic stenosis, we consider it with peak velocity. This gives us a full picture of the disease’s severity.
The indexed aortic valve area gives a more personal look at aortic stenosis. It considers the patient’s body size. This is key for accurate diagnosis, mainly for those with smaller frames.
To find the indexed aortic valve area, we divide the valve area by the body surface area. The result is in cm²/m². Values above 0.85 cm²/m² are normal. But, values under 0.6 cm²/m² show severe aortic stenosis.
An indexed AVA under 0.6 cm²/m² means severe aortic stenosis. It shows the valve is too narrow for the body size. This is a key sign for needing treatment.
For those with smaller frames, adjusting the aortic valve area is vital. It makes the diagnosis more accurate. This way, they get care that fits their needs perfectly.
There’s a critical point beyond severe aortic stenosis that greatly affects patient outcomes. Critical aortic stenosis is marked by an aortic valve area (AVA) of less than 0.7 cm². This shows a more severe blockage than the usual severe stenosis criteria.
An AVA of less than 0.7 cm² means the aortic valve is severely narrowed. This is key for diagnosing critical aortic stenosis. It directly impacts the patient’s hemodynamic changes.
The reduced AVA in critical aortic stenosis causes big changes in blood flow. These include higher pressure gradients and left ventricular hypertrophy. As “the presence of a high gradient across the aortic valve is a hallmark of critical aortic stenosis” (reference not provided).
These changes can lead to symptoms like chest pain, shortness of breath, and syncope.
Patients with critical aortic stenosis show severe symptoms that need quick medical check-ups. They might have signs of heart failure, angina, or syncope. As
“the clinical presentation of critical aortic stenosis is often dramatic, with patients experiencing severe and potentially life-threatening symptoms”
. Quick action is key to avoid serious outcomes, like death.
We stress that critical aortic stenosis needs urgent care because of its high risk of serious illness and death. It’s vital for healthcare providers to understand its definition, effects on blood flow, and symptoms. This helps in managing the condition well.
Diagnosing low-flow, low-gradient aortic stenosis is tough. It has complex hemodynamic traits. Traditional echocardiographic measures often don’t show the real stenosis severity.
Paradoxical low-flow severe aortic stenosis is when patients have a normal heart function but severe stenosis. This condition is linked to a poor prognosis and needs careful diagnosis and treatment. It’s important to understand its pathophysiology to spot these patients.
Dobutamine stress echocardiography is key in evaluating low-flow, low-gradient aortic stenosis. This test helps tell true severe aortic stenosis from pseudo-severe by checking the valve’s response to dobutamine. It reveals the real stenosis severity by boosting flow across the valve.
Telling true severe aortic stenosis from pseudo-severe is vital for treatment. Dobutamine stress echocardiography is essential in this, as it spots patients who might need valve surgery. Accurate diagnosis is key to giving the right treatment.
In summary, diagnosing low-flow, low-gradient aortic stenosis is hard. Understanding paradoxical low-flow severe AS and using dobutamine stress echocardiography helps identify those who need valve intervention.
The left ventricle faces a big challenge when the aortic valve narrows. It must work harder to keep blood flowing. This leads to left ventricular hypertrophy.
At first, the left ventricle gets bigger and changes shape to handle the extra pressure. This helps it keep pumping blood. But, it can also cause diastolic dysfunction and make the heart work too hard.
As aortic stenosis gets worse, signs of heart failure may show up. These include shortness of breath, feeling tired, and not being able to exercise as well. Echocardiograms can also show if the left ventricle is not working right.
When the left ventricle doesn’t work well in severe aortic stenosis, it’s a big warning sign. People with low LVEF need help sooner. The table below shows important signs for how well a patient might do.
| Prognostic Indicator | Normal Value | Abnormal Value |
|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | >55% | |
| Left Ventricular End-Diastolic Diameter (LVEDD) | >5.5 cm | |
| Mean Pressure Gradient | >40 mmHg |
It’s key to understand how the left ventricle reacts to severe aortic stenosis. Knowing how it adapts and when it starts to fail helps doctors help patients better.
Symptomatic severe aortic stenosis is a serious issue that needs quick action to save lives. When symptoms show up, it’s a big warning sign. Doctors must carefully check the patient to decide the best treatment.
Knowing the risk is key in treating severe aortic stenosis. Echocardiograms are very important. They show how bad the stenosis is and how well the heart is working.
Important echo details include aortic valve area, mean pressure gradient, and peak velocity. These help doctors figure out the risk of serious problems. They help decide when and how to treat the patient.
Choosing the right time and method for treatment is very important. Doctors can use surgery or a less invasive procedure called TAVR. The choice depends on the patient’s health and what they prefer.
A multidisciplinary heart team discussion helps decide the best treatment plan for each patient.
Patients without symptoms but with severe aortic stenosis need regular checks. They usually get echocardiograms and check-ups to watch for any changes. How often they need these checks depends on their risk and how severe their stenosis is.
Using echocardiographic criteria is key for managing severe aortic stenosis well. It helps doctors make better decisions and improves patient care. We talked about important factors like aortic valve area, mean pressure gradient, and peak velocity.
Getting a correct diagnosis and knowing how severe the stenosis is is very important. Echocardiography helps a lot in this area. It lets doctors find out who needs treatment and keep an eye on those who don’t show symptoms.
Knowing the echocardiographic criteria for severe aortic stenosis helps doctors plan better care. As cardiology keeps getting better, using these criteria will always be important for the best patient care.
To diagnose severe aortic stenosis, doctors look at seven key factors. These include the aortic valve area, mean pressure gradient, and peak velocity. They also consider the indexed aortic valve area, velocity time integral, left ventricular function, and valve morphology.
Severe aortic stenosis is defined by a few criteria. An aortic valve area under 1.0 cm² is one sign. A mean pressure gradient over 40 mmHg and a peak velocity above 4.0 m/sec are also indicators.
The aortic valve area is calculated using the continuity equation. This equation considers the velocity time integral of the left ventricular outflow tract and the aortic valve.
An AVA under 1.0 cm² means severe aortic stenosis. It’s a serious condition that needs immediate medical attention. This might include surgery or a transcatheter procedure.
Critical aortic stenosis is when the AVA is under 0.7 cm². This is a severe case that requires urgent medical care due to its serious effects on blood flow.
A mean pressure gradient over 40 mmHg suggests severe aortic stenosis. But, it’s important to consider the flow to ensure accurate diagnosis.
Peak velocities over 4.0 m/sec indicate severe aortic stenosis. It’s important to align the Doppler correctly for precise measurement.
Indexed aortic valve area adjusts for body size. An indexed AVA below 0.6 cm²/m² suggests severe aortic stenosis, mainly in smaller patients.
Low-flow, low-gradient aortic stenosis is a challenging diagnosis. It requires dobutamine stress echocardiography to distinguish between true severe AS and pseudo-severe AS.
Left ventricular dysfunction worsens the prognosis of severe aortic stenosis. Quick intervention is needed to prevent further decline.
Deciding on treatment for symptomatic severe aortic stenosis involves several steps. These include assessing risk, timing of intervention, and choosing between surgery or a transcatheter approach.
Asymptomatic patients with severe aortic stenosis need regular monitoring. This includes echocardiography to track disease progression and determine the best time for treatment.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!