Last Updated on November 27, 2025 by Bilal Hasdemir

Getting a diagnosis of aortic valve calcification can be scary. We get it. At Liv Hospital, we’re here to help you understand this condition. We want you to know the latest and get the best care.
Aortic valve calcification gets worse over time. It makes the valve stiff and blocks blood flow. This can cause chest pain, trouble breathing, and feeling faint. Research shows that up to 25% of people over 65 have some aortic valve calcification. But not everyone will get to a severe blockage.
Key Takeaways
- Understanding aortic valve calcification is key to managing it.
- The condition gets worse and can cause severe blockage.
- Symptoms include chest pain, shortness of breath, and fainting.
- Early diagnosis is important for good management.
- Liv Hospital offers innovative, patient-focused care for aortic valve calcification.
What Happens to Your Heart with Aortic Valve Calcification
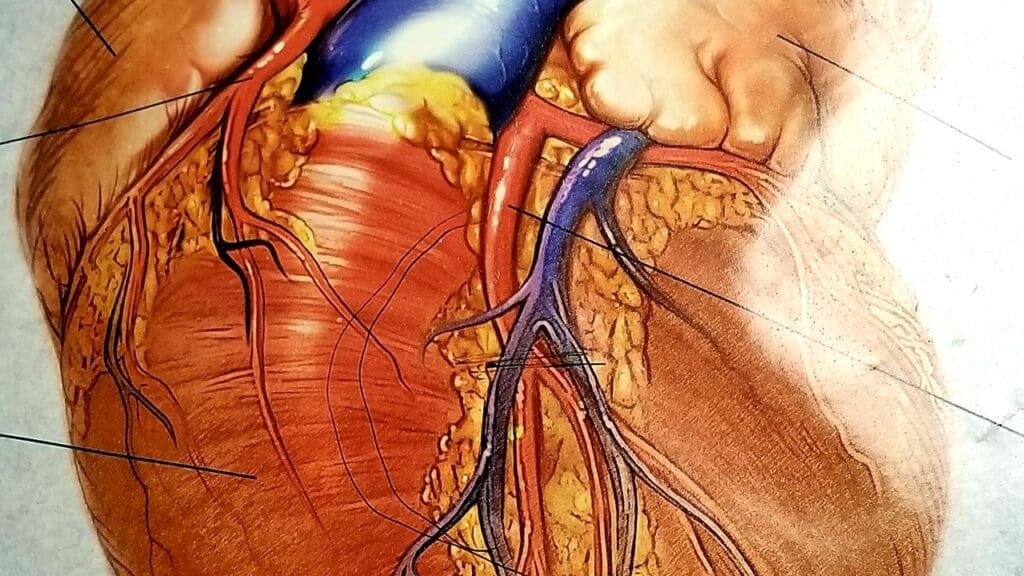
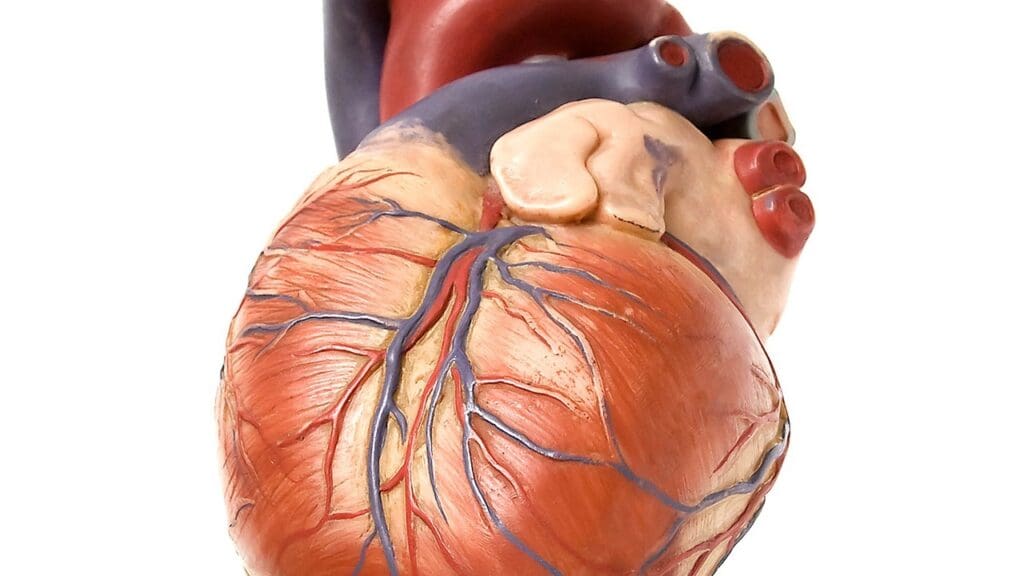
The aortic valve is key to heart health. Calcification can mess with this. It helps control blood flow from the left ventricle to the aorta, the biggest artery. When it works right, it makes sure blood flows only one way, keeping it out of the heart.
The Role of the Aortic Valve in Heart Function
The aortic valve is vital for blood circulation. It opens to let blood flow from the heart to the aorta and then closes to stop backflow. It has three cusps that work together for proper blood flow. In a healthy heart, it pumps blood efficiently all over the body.
How Calcification Disrupts Normal Blood Flow
Calcification happens when calcium builds up on the valve cusps, making them stiff. This makes the valve open and close poorly, causing impaired blood flow. The heart has to work harder, leading to symptoms like chest pain, shortness of breath, and fatigue. Severe calcification can cause serious heart problems if not treated.
Studies show that aortic valve calcification is more than just aging. Things like high blood pressure, chronic kidney disease, and high cholesterol can make it worse. Knowing this helps in managing and possibly slowing the disease.
Aortic Valve with Severe Aortic Calcification: The Progressive Nature
Aortic valve calcification can seriously harm heart function and overall health. We’ll look at how it goes from mild to severe, affecting the valve and heart health.
From Mild Thickening to Severe Obstruction
Calcification starts with the valve leaflets getting slightly thicker. Over time, it can get worse, causing severe obstruction of blood flow. Research shows this can raise the risk of heart problems.
Why Valve Flexibility Decreases Over Time
Calcium builds up on the valve, making it stiff and less flexible. This hampers the valve’s ability to open and close, leading to reduced valve flexibility and severe aortic stenosis.
The Impact on Your Cardiovascular System
As aortic valve calcification gets worse, it puts more strain on the heart. If not treated, it can lead to heart failure. Below is a table showing how calcification affects heart health.
| Stage of Calcification | Impact on Valve Function | Cardiovascular Implications |
|---|---|---|
| Mild Thickening | Minimal impact on valve function | Low risk of cardiovascular events |
| Moderate Calcification | Reduced valve flexibility | Increased risk of cardiovascular events |
| Severe Calcification | Significant obstruction of blood flow | High risk of heart failure and cardiovascular mortality |
It’s key to understand how aortic valve calcification progresses to manage heart health. Early detection and action can help reduce its impact and improve outcomes.
Key Fact #1: Prevalence and Demographics
Aortic valve calcification is common among older adults worldwide. As we get older, the risk of this condition grows. It’s a big health issue for this age group.
Statistics Among Older Adults
Studies show that about 25% of people over 65 have some calcification. This highlights the need to watch our heart health as we age.
Why 25% of People Over 65 Show Some Degree of Calcification
Several factors contribute to aortic valve calcification in older adults. These include aging, lifestyle choices, and other health issues. As we age, our aortic valve changes, leading to calcification.
Who Is Most at Risk for Progression to Severe Disease
Some people are more likely to see their calcification worsen. This includes those with high blood pressure, kidney disease, and high cholesterol. Knowing these risks helps us find who needs early care.
| Risk Factor | Description | Impact on Aortic Valve Calcification |
|---|---|---|
| Hypertension | High blood pressure | Increases stress on the aortic valve, accelerating calcification |
| Chronic Kidney Disease | Long-term kidney damage | Disrupts mineral metabolism, contributing to calcification |
| High Cholesterol | Elevated levels of cholesterol in the blood | Contributes to the development of atherosclerosis, which is associated with aortic valve calcification |
Knowing about aortic valve calcification helps us spot risks early. This way, we can take steps to slow its progression.
Key Fact #2: Beyond Normal Aging – The Science of Valve Calcification
Aortic valve calcification is more than just aging. It’s a complex process with many factors at play. We’ll look into what drives this condition, beyond the simple idea that it’s just age.
Inflammatory Processes Involved
An inflammatory response plays a big role in aortic valve calcification. Research shows that inflammatory cells and substances help create calcific lesions on the valve. This isn’t just a passive process; it’s an active biological response with many cellular and molecular pathways involved.
Cellular Mechanisms Behind Calcification
The process of aortic valve calcification involves many cell types, like valve interstitial cells and immune cells. These cells help calcify the valve through calcium deposition and the production of pro-calcific factors. Understanding these cellular processes is key to finding effective treatments.
For more details on these cellular mechanisms, check out studies in reputable medical journals. For example, this link offers insights into recent cardiology and valve calcification research.
The Difference Between Age-Related Changes and Pathological Calcification
Age can contribute to aortic valve calcification, but it’s important to tell normal aging apart from pathological calcification. Pathological calcification is an active disease process, not just normal wear and tear. Knowing the difference is key to finding the right treatment.
| Characteristics | Age-Related Changes | Pathological Calcification |
|---|---|---|
| Process | Gradual wear and tear | Active disease process |
| Inflammation | Minimal or absent | Present and significant |
| Cellular Involvement | Limited | Complex interplay of cells |
Key Fact #3: Recognizing the Warning Signs
It’s important to know the warning signs of aortic valve calcification. This is key for early diagnosis and treatment. As the condition gets worse, symptoms can really affect a person’s life.
Chest Pain and Angina
Chest pain, or angina, is a common symptom. It happens when the heart doesn’t get enough oxygen-rich blood. This can be caused by hard work or stress. Angina feels like a squeezing or pressure in the chest, and it can spread to the arms, back, or jaw.
Shortness of Breath and Reduced Exercise Tolerance
As the condition gets worse, breathing becomes harder and doing things gets more tiring. People might feel out of breath or very tired doing simple tasks. This is a sign that the heart is not working well.
Fainting Episodes and Their Significance
Fainting, or syncope, is a serious symptom that needs quick medical help. Severe calcification can cut down blood flow to the brain, causing dizziness or fainting. Fainting is a warning sign and needs a doctor’s check-up right away.
Subtle Symptoms Often Overlooked
Some symptoms are so mild, people might miss them. Feeling tired or just not feeling right can be signs of many things. It’s important to see a doctor to find out what’s really going on.
| Symptom | Description | Significance |
|---|---|---|
| Chest Pain/Angina | Squeezing or pressure sensation in the chest | Indicates reduced blood flow to the heart muscle |
| Shortness of Breath | Difficulty breathing during exertion or at rest | Signifies the heart’s reduced ability to meet the body’s needs |
| Fainting Episodes | Dizziness or loss of consciousness | Red flag for severe aortic valve calcification |
For more information on diagnosing and managing severe aortic stenosis, visit Valvular Emergencies: Diagnosis and Management of Severe Aortic.
Key Fact #4: The Spectrum from Mild to Severe Calcification
It’s important to understand the range of aortic valve calcification. This range goes from mild to severe, each with its own health impact. The severity of calcification affects treatment choices and outcomes.
Mildly Calcified Aortic Valve: What It Means
A mildly calcified aortic valve is in the early stages. The valve might work okay, but calcium deposits are starting to form. Monitoring is essential to watch how it progresses.
Mild Aortic Valve Sclerosis and Its Implications
Mild aortic valve sclerosis shows early signs of thickening and calcification. It might not block blood flow much at first. But, it could lead to more serious valve disease. We need to watch for signs of worsening.
Moderate Calcification: The Turning Point
Moderate calcification is a key moment. The valve starts to work less well. The leaflets are heavily calcified, causing symptoms and changes in blood flow. Careful evaluation is needed to decide the best course of action.
Severe Calcification: When Intervention Becomes Necessary
Severe calcification blocks the valve a lot and causes symptoms like chest pain and shortness of breath. At this point, replacing the valve is often needed. Surgical or transcatheter aortic valve replacement might be considered, depending on the patient’s health.
Everyone’s aortic valve calcification progresses differently. Regular checks and a tailored management plan are key to the best results.
Key Fact #5: Risk Factors You Can and Cannot Control
Aortic valve calcification is caused by both things you can and can’t control. Knowing these factors is key to managing the condition well.
Hypertension and Blood Pressure Management
High blood pressure, or hypertension, is a big risk for aortic valve calcification. By managing blood pressure through lifestyle changes and medicine, you can slow the condition’s progress.
Chronic Kidney Disease Connection
Chronic kidney disease increases the risk of aortic valve calcification. The link between kidney health and valve health shows why managing kidney disease is vital for heart health.
Cholesterol Levels and Valve Health
Cholesterol levels affect the development and growth of aortic valve calcification. Keeping cholesterol levels healthy through diet, exercise, and medicine (if needed) helps your valve stay healthy.
Genetic Factors in Aortic Valve Calcification
While some risks can be managed, genetic factors also influence aortic valve calcification. Knowing your family’s health history and genetic predisposition helps in early detection and management.
The main risk factors for aortic valve calcification are:
- Hypertension
- Chronic kidney disease
- High cholesterol levels
- Genetic predisposition
By managing these risks through lifestyle changes and medical treatments, you can slow the growth of aortic valve calcification.
Key Fact #6: Diagnosis and Monitoring Methods
Healthcare providers use many ways to manage aortic valve calcification. Accurate diagnosis is key to knowing how severe it is and what treatment is needed.
Physical Examination Findings
A physical exam is often the first step in diagnosing aortic valve calcification. Doctors listen for heart murmurs, like a systolic ejection murmur, which can show aortic stenosis. They also look for a slow or delayed pulse and differences in blood pressure between arms.
Echocardiography: The Gold Standard
Echocardiography is the top choice for diagnosing aortic valve calcification. It gives detailed images of the heart, letting doctors see how the valve is doing and how severe the stenosis is. Doppler echocardiography also checks blood flow across the valve.
CT Scans and Calcium Scoring
CT scans and calcium scoring help measure calcification. These tests show how much calcium is in the aortic valve. This info helps doctors decide on treatment.
Follow-up Protocols for Different Severity Levels
Follow-up plans change based on how severe the aortic valve calcification is. For mild cases, yearly echocardiograms might be needed. For more severe cases, check-ups could be every 6-12 months. Regular check-ups help catch any changes and adjust treatment plans.
By using these methods, doctors can fully understand a patient’s condition. This helps them give care that’s just right for each person.
Key Fact #7: Treatment Options and Their Outcomes
Treatment for aortic valve calcification has grown a lot. Now, patients have many choices based on their needs. It’s key to know the good and bad of each option.
Medical Management Strategies
For those with mild to moderate calcification, doctors often start with medical management. This method aims to control symptoms and slow the disease’s growth. Keeping blood pressure and cholesterol in check is vital to ease heart strain and slow calcification.
Surgical Valve Replacement
For severe calcification, surgery is often the best choice. It involves swapping the old valve with a new one. This surgery has a proven track record of improving life quality and outcomes.
Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a less invasive option for those at high surgical risk. It uses a catheter to install a new valve. TAVR offers a quicker recovery and lower risk of complications.
Choosing the Right Intervention for Your Situation
Choosing the right treatment depends on many factors. These include how severe the calcification is, your overall health, and what you prefer. A thorough review by a healthcare team is needed to find the best treatment. This way, doctors can help patients choose the most effective option for them.
Living Well with Aortic Valve Calcification
Aortic valve calcification can be tough, but many people live active lives with the right approach. Getting a diagnosis can feel overwhelming. Yet, with the right lifestyle changes and medical care, people can greatly improve their life quality.
Lifestyle Modifications That Make a Difference
Healthy lifestyle choices are key in managing aortic valve calcification. Regular physical activity, a balanced diet, and stress management are essential. Research shows these changes can help manage the condition and related heart diseases.
Exercise Guidelines for Different Severity Levels
The severity of aortic valve calcification affects the type and intensity of exercise. For mild cases, aerobic exercises like walking or cycling are good. In more severe cases, it’s important to talk to a healthcare provider for a personalized exercise plan.
Dietary Approaches to Support Heart Valve Health
Eating a heart-healthy diet full of fruits, vegetables, and whole grains is beneficial. It’s also important to limit sodium intake and avoid excessive alcohol consumption.
Managing Related Cardiovascular Conditions
People with aortic valve calcification often have other heart conditions like high blood pressure or high cholesterol. Effective management of these conditions through medication and lifestyle changes is critical.
By following these strategies, individuals with aortic valve calcification can live more fulfilling lives. It’s about making smart choices and working with healthcare providers to manage the condition well.
Conclusion
Understanding aortic valve calcification is key to managing and treating it. We’ve looked at important facts about this condition. This includes how common it is in older adults and the treatment options available.
Studies show that a detailed approach to managing aortic valve calcification can greatly help patients. By spotting early signs, knowing the risks, and using the right tests, we can act quickly. This can slow down the disease’s progress.
Managing aortic valve calcification well means using many strategies. This includes making lifestyle changes, using medicine, and sometimes surgery or a new valve. This approach can greatly improve life for those with this condition.
Aortic valve calcification is a complex issue that needs careful handling. By staying up-to-date and working with doctors, people can get through treatment well. This leads to the best possible results.
What is aortic valve calcification?
Aortic valve calcification is when calcium builds up on the aortic valve. This can make it hard for blood to flow properly. It can cause symptoms and lead to serious health issues.
How does aortic valve calcification affect heart function?
It makes the valve stiff, which can disrupt blood flow. This can cause chest pain, shortness of breath, and fainting. These are signs that the valve is not working right.
What are the risk factors for aortic valve calcification?
Risk factors include high blood pressure, high cholesterol, and kidney disease. Some, like high blood pressure, can be managed. Others, like genetics, can’t.
How is aortic valve calcification diagnosed?
Doctors use physical exams, echocardiograms, CT scans, and calcium scores to diagnose it. The right tool depends on how severe it is and the patient’s health.
What are the treatment options for aortic valve calcification?
Mild cases might be treated with medication. But severe cases might need surgery or a procedure called TAVR. The choice depends on how bad it is and the patient’s health.
Can lifestyle modifications help manage aortic valve calcification?
Yes, making healthy lifestyle choices can help. This includes eating right, exercising, and managing heart conditions. It can improve heart health.
What is the difference between age-related changes and pathological calcification of the aortic valve?
Age-related changes are just wear and tear. But pathological calcification is an abnormal process. It involves inflammation and can severely damage the valve.
How often should I have follow-up check-ups for aortic valve calcification?
How often depends on how severe it is. Regular check-ups are key to tracking the condition and deciding if treatment is needed.
Is aortic valve calcification common among older adults?
Yes, many people over 65 have some degree of calcification. About 25% have noticeable calcification.
What are the symptoms of severe aortic valve calcification?
Symptoms include chest pain, shortness of breath, and fainting. These are signs that the valve is severely damaged and needs medical attention.
Can mild aortic valve calcification progress to severe disease?
Yes, mild calcification can get worse over time. This is more likely if risk factors are not managed. Regular monitoring is important to track this.
References
- Vinmec International Hospital (Heart Valve Calcification) : https://www.vinmec.com/en/blog/heart-valve-calcification-symptoms-and-treatment-en
- AHA Journals (Circulation) : https://www.ahajournals.org/doi/circulationaha.104.486738
- Dr. Yavuz Beşoğul (Heart Valve Calcification) : https://dryavuzbesogul.com/kalp-kapakcigi-kireclenmesi-curumesi
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC4888946
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC6873465