
Being told you have a calcified aortic valve can worry you about your heart. At Liv Hospital, we offer clear advice and caring support. A calcified aortic valve happens when calcium builds up on the valve, making it stiff and thick. This can block blood flow.
Getting a aortic valve calcification diagnosis can be scary. Our team is here to help you, with the newest treatments for mild calcification. We aim to keep your heart healthy by understanding this condition.
Key Takeaways
- Knowing why aortic valve calcification happens is key to managing it.
- Mild calcification needs careful watching and maybe some prevention steps.
- Liv Hospital focuses on caring for your heart valve health.
- We follow the best practices for calcified aortic valve care.
- Spotting and treating it early can greatly improve your outcome.
The Aortic Valve: Normal Structure and Function
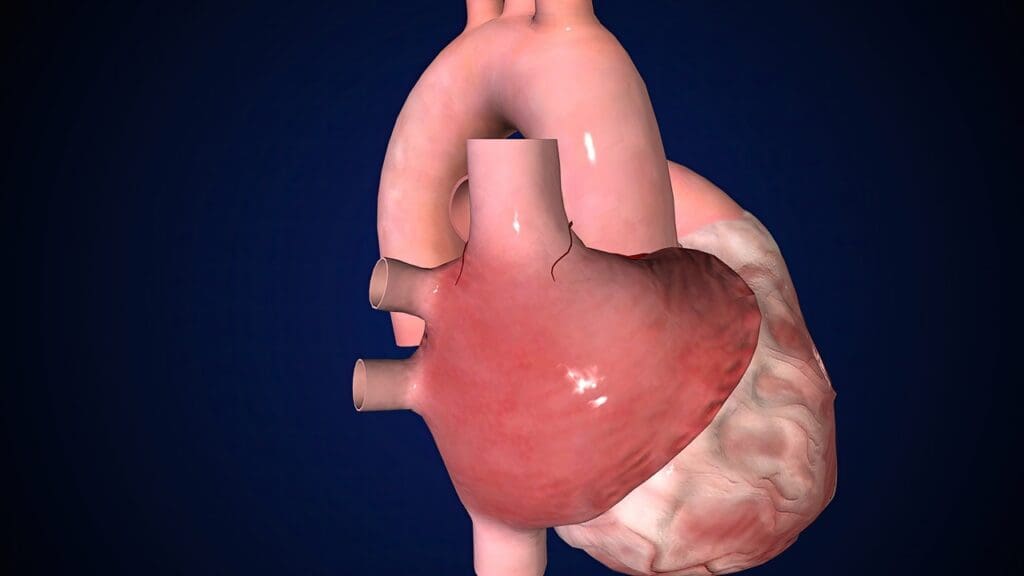
Knowing how the aortic valve works is key to treating heart problems. It’s a vital part of the heart, making sure blood moves right from the heart to the body.
Anatomy of a Healthy Aortic Valve
A healthy aortic valve has three delicate, flexible cusps. These cusps are attached to the aortic root. They open and close with each heartbeat, letting blood flow only one way, from the left ventricle to the aorta.
How the Aortic Valve Regulates Blood Flow
The aortic valve controls blood flow by opening during systole. This lets blood pump from the left ventricle into the aorta. It closes during diastole, stopping blood from flowing back into the ventricle. This control is essential for keeping blood pressure right and ensuring tissues get enough oxygen.
Understanding the aortic valve’s role in heart health is important. Knowing how it works helps us see the impact of problems like aortic valve calcification.
What Is an Aortic Valve Calcified? The Pathophysiology
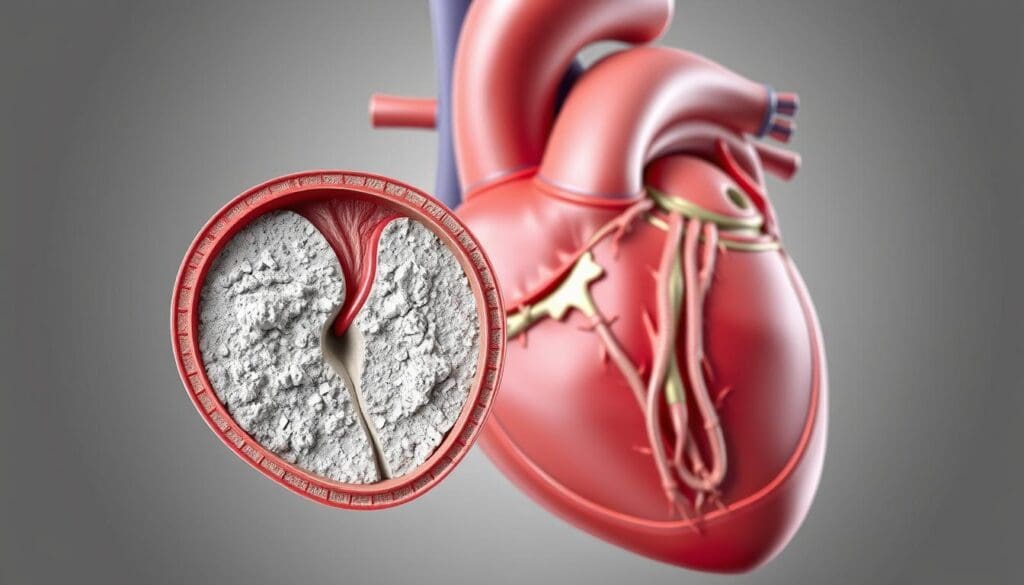
Understanding aortic valve calcification is key to managing it well. This condition involves a mix of processes that lead to calcium buildup on the valve leaflets.
The Process of Calcium Deposition
Calcium buildup on the aortic valve is a complex process. Recent studies show that inflammation and lipid buildup are key in starting and growing calcification.
Valve Thickening and Stiffening
As calcification grows, the valve leaflets get thicker and stiffer. This makes it hard for them to work right. It causes mechanical changes and hemodynamic effects that make things worse.
Mechanical Changes
The mechanical changes include less leaflet movement and more stiffness. This can cause aortic stenosis.
Hemodynamic Effects
The hemodynamic effects come from changed blood flow patterns. This can lead to higher pressure gradients across the valve.
Difference Between Sclerosis and Stenosis
It’s important to know the difference between aortic valve sclerosis and stenosis. Sclerosis means the valve gets thick and calcified but doesn’t block much. Stenosis is when the valve gets so narrow it blocks a lot of blood flow.
Causes and Risk Factors for Aortic Valve Calcification
It’s important to know what causes aortic valve calcification. This knowledge helps in early detection and treatment. We will look at the different factors that lead to this condition.
Age-Related Degeneration
As we get older, our aortic valve naturally wears out. This can cause calcification. Other health issues can make this process worse.
Medical Conditions That Accelerate Calcification
Some medical conditions can make calcification happen faster. These include:
- Chronic Kidney Disease
- Hypertension
- Hyperlipidemia
Chronic Kidney Disease
Chronic kidney disease speeds up aortic valve calcification. This is because kidney problems affect mineral balance.
Hypertension
Hypertension, or high blood pressure, strains the heart and valves. This can make calcification happen faster.
Hyperlipidemia
High cholesterol or triglycerides in the blood can lead to aortic valve calcification.
Congenital Anomalies and Genetic Factors
Certain birth defects and genetic factors can increase the risk of aortic valve calcification. These can cause abnormal valve structure or function, raising the risk of calcification.
Understanding Mild Aortic Valve Calcification
Mild aortic valve calcification is a condition that needs careful watching. It’s important to understand its effects on heart health.
Defining Mild Aortic Valve Sclerosis
Mild aortic valve sclerosis is the early stage of calcification on the aortic valve. It shows a mildly thickened aortic valve. This might not block blood flow much but shows the start of a serious problem.
Echocardiographic Findings
Echocardiography is key in spotting mild aortic valve calcification. It can show:
- Thickening of the valve leaflets
- Mild calcification on the valve
- Normal or slightly reduced valve mobility
These signs help figure out how serious the condition is and what to do next.
Natural History and Progression Rates
The way mild aortic valve calcification changes can differ from person to person. Some might stay the same for years, while others could get worse.
Factors That Influence Progression
Several things can make mild aortic valve calcification get worse, including:
- Age and overall heart health
- Having other health issues like high blood pressure or diabetes
- How you live, like your diet and exercise
Timeframe for Possible Changes
How fast mild aortic valve calcification can change varies a lot. It’s key to keep an eye on it with regular echocardiograms to catch any changes.
We stress the need for personalized care and regular check-ups for mild aortic valve calcification. Knowing what can make it worse helps us create better plans for each person.
Symptoms and Clinical Presentation
It’s important to know the symptoms of aortic valve calcification to get help early. We’ll look at the different stages of symptoms, from when you might not feel anything to when symptoms get worse.
Asymptomatic Phase of Mild Calcification
In the early stages, you might not feel any symptoms. This can go on for years. You might find out about it when you go for a check-up for something else.
Early Warning Signs
As the calcification gets worse, you might start to feel some signs. These can be small things like feeling tired or a bit out of breath when you’re active. It’s key to tell your doctor if you notice these changes.
Advanced Symptoms as Calcification Progresses
When the calcification gets more serious, symptoms can get worse. You might experience:
Chest Pain
Chest pain, or angina, happens when your heart muscle doesn’t get enough oxygen. It can happen when you’re active or stressed, and it usually goes away when you rest.
Shortness of Breath
Feeling short of breath, or dyspnea, is another symptom. It’s because your heart can’t pump blood well. You might feel it when you’re active or even when you’re sitting or lying down.
Syncope and Heart Failure
In the worst cases, you might faint or have heart failure. Heart failure means your heart can’t pump enough blood. This can make you feel tired, swell up, and have other problems.
For more info on aortic valve stenosis, a related issue, check out
| Symptom | Description |
|---|---|
| Chest Pain | Angina or discomfort in the chest due to insufficient oxygen-rich blood to the heart muscle. |
| Shortness of Breath | Dyspnea or difficulty breathing due to the heart’s reduced efficiency in pumping blood. |
| Syncope | Fainting or loss of consciousness due to reduced blood flow to the brain. |
| Heart Failure | A condition where the heart is unable to pump enough blood to meet the body’s needs. |
Diagnostic Approaches for Aortic Valve Calcifications
We use different methods to find and treat aortic valve calcifications. Knowing the exact cause is key to choosing the right treatment.
Echocardiography: The Gold Standard
Echocardiography is the top choice for checking aortic valve calcification. It shows detailed pictures of the valve’s shape and how it works.
Transthoracic Echocardiography
Transthoracic echocardiography (TTE) is a safe way to look at the aortic valve. It’s easy to get and gives lots of info on the valve’s health.
Transesophageal Echocardiography
Transesophageal echocardiography (TEE) gives clearer images of the aortic valve than TTE. It’s best when you need a closer look.
Additional Imaging Techniques
Other imaging tools also help in diagnosing and treating aortic valve calcification.
CT Scanning
Computed Tomography (CT) scans measure how much calcification there is. They also check the heart’s overall shape and size.
MRI Evaluation
Magnetic Resonance Imaging (MRI) shows detailed heart pictures without radiation. It helps see how calcification affects the heart’s work.
Laboratory Assessment
Labs test for reasons behind aortic valve calcification. They also keep an eye on the heart’s health.
| Diagnostic Test | Purpose |
|---|---|
| Echocardiography | Assess valve structure and function |
| CT Scanning | Quantify calcification extent |
| MRI | Evaluate cardiac structure and function |
| Laboratory Tests | Identify underlying causes and monitor health |
Management Strategies for Mild Aortic Valve Calcification
Patients with mild aortic valve calcification need a plan to stop it from getting worse. We’ll talk about how to monitor, change your lifestyle, and lower heart disease risk.
Monitoring Protocols
Keeping an eye on your condition is key. This means:
- Regular echocardiograms to check how the valve is doing.
- Doctor visits to watch for symptoms and heart health.
Frequency of Follow-up
How often you see a doctor and get an echocardiogram depends on your risk. Usually, it’s every 2-3 years for mild calcification.
What Changes Warrant Concern
If you feel new or worse symptoms like chest pain or shortness of breath, get help right away.
Lifestyle Modifications
Changing your lifestyle is important for managing mild aortic valve calcification. These changes include:
Dietary Approaches
Eating well is key. Focus on fruits, veggies, whole grains, and lean meats. Cut down on fats, cholesterol, and salt.
Exercise Recommendations
Stay active with exercises like walking or swimming. Talk to your doctor about the best plan for you.
Smoking Cessation
Quitting smoking is a must for heart health. We offer help to stop smoking.
Cardiovascular Risk Reduction
Lowering heart disease risk is vital for patients with mild aortic valve calcification.
Blood Pressure Management
Keeping blood pressure in check is important. Use lifestyle changes and meds if needed.
Lipid Control
Manage cholesterol with diet, exercise, and statins if needed.
Diabetes Management
For those with diabetes, controlling blood sugar is key to avoid heart problems.
By following these strategies, patients can lower their risk of heart problems. We help each patient create a plan that fits their needs and risk.
Treatment Options When Calcification Progresses
When aortic valve calcification gets worse, we need a strong plan to treat it. This plan includes both medicine and surgery. We move from just watching the condition to actively treating it to stop it from getting worse and to ease symptoms.
Medical Management Approaches
First, we try to control symptoms and slow the disease with medicine. We use drugs to handle high blood pressure, heart failure, and other issues. We also suggest changing your diet and starting to exercise to lower heart risks.
Surgical Interventions
If medicine doesn’t work, we might need surgery. Aortic Valve Replacement (AVR) is a common surgery for this.
Aortic Valve Replacement
AVR means replacing the old valve with a new one. The new valve can be mechanical or bioprosthetic. We choose based on your age, lifestyle, and health.
Candidate Selection
AVR is for people with severe aortic stenosis or bad symptoms. We decide if surgery is right for you based on your health and the risks.
Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a less invasive option for those at high risk for surgery.
Procedure Overview
TAVR puts a new valve in your heart through a catheter, usually from your leg. It’s less invasive than open-heart surgery and you might recover faster.
Benefits and Risks
TAVR has fewer risks and quicker recovery. But, it can cause stroke, vascular problems, and leaks around the valve.
Emerging Therapies and Clinical Trials
We’re always looking for new ways to treat aortic valve calcification. This includes medicines that might slow or stop the disease.
| Treatment Option | Description | Benefits |
|---|---|---|
| Medical Management | Control symptoms and slow disease progression | Non-invasive, can be used in early stages |
| Aortic Valve Replacement (AVR) | Replace diseased valve with mechanical or bioprosthetic valve | Effective for severe aortic stenosis, improves survival |
| Transcatheter Aortic Valve Replacement (TAVR) | Less invasive valve replacement via catheter | Reduced risk of complications, faster recovery |
Cardiovascular Risk and Long-term Prognosis
Mild aortic valve calcification might seem harmless, but it’s not. It affects your heart health and future well-being. Knowing the risks and outcomes is key.
Increased Cardiovascular Risk with Mild Calcification
Mild calcification on the aortic valve is not just a normal part of aging. It raises your chance of heart problems. Research shows it can signal widespread atherosclerosis, increasing risks of heart disease and stroke.
Seeing calcification on the aortic valve means you might have more atherosclerosis. This is bad for your heart health. So, managing risk factors is very important.
Factors Affecting Disease Progression
How fast aortic valve calcification gets worse depends on several things. These include age, high blood pressure, high cholesterol, and smoking. Knowing these factors helps predict how the disease will progress and how to treat it.
Keeping an eye on the calcification and changing risk factors is key. This can slow down the calcification and lower heart disease risk.
Life Expectancy and Quality of Life
The effect of mild aortic valve calcification on life expectancy and quality of life varies. Some people stay symptom-free for years, while others see it worsen quickly. This might mean they need closer monitoring or more aggressive treatment.
It’s important to have a care plan that fits the individual. This plan should consider their health, any other health issues, and the details of their calcification.
When to Consider More Aggressive Intervention
Deciding when to take a more serious approach to treating aortic valve calcification is complex. It depends on how fast the disease is getting worse, if symptoms are present, and the patient’s overall heart health risk.
If the calcification is getting worse fast or causing symptoms, more intense treatments might be needed. This could include advanced tests, more frequent check-ups, or even surgery like TAVR.
Understanding the risks and outcomes of aortic valve calcification helps doctors give better care. This can lead to better health and quality of life for patients.
Conclusion: Living with a Calcified Aortic Valve
We’ve talked about the complex issues of aortic valve calcification. This includes its causes and how to manage it. To live with it, you need to watch your health closely, make lifestyle changes, and lower your heart disease risk.
If you have mild aortic valve calcification, eating right and exercising are key. You should also control high blood pressure and high cholesterol. We believe in a team effort to manage your condition well.
Mild thickening of the aortic valve can lead to worse problems. It’s important to keep an eye on it and act fast to stop it from getting worse. By knowing the risks and acting early, you can lessen the effects on your life.
We aim to offer top-notch healthcare to patients from around the world. We’re here to help you deal with the challenges of aortic valve calcification. We want to make sure you get the best care and advice every step of the way.
What is aortic valve calcification?
Aortic valve calcification is when calcium builds up on the aortic valve. This makes the valve stiff and thick, which can slow blood flow from the heart.
What are the causes of aortic valve calcification?
It can happen due to age, certain health conditions like kidney disease and high blood pressure, and some birth defects.
How is mild aortic valve calcification diagnosed?
Doctors use echocardiography to spot mild calcification. This test shows how much calcium is there and how well the valve works.
What are the symptoms of aortic valve calcification?
At first, you might not feel anything. But as it gets worse, you could have chest pain, trouble breathing, and fainting.
How is mild aortic valve calcification managed?
Doctors keep an eye on it and suggest lifestyle changes. This includes eating right, exercising, and managing blood pressure and diabetes.
What are the treatment options when aortic valve calcification progresses?
If it gets worse, treatments include medicine, surgery, or a new valve put in through a catheter. The choice depends on how bad it is.
Can lifestyle changes help manage aortic valve calcification?
Yes, making healthy choices can help. Eating well, exercising, quitting smoking, and controlling blood pressure and diabetes can slow it down.
What is the difference between aortic valve sclerosis and stenosis?
Sclerosis means the valve is thick and calcified but blood flow isn’t blocked much. Stenosis is when the valve narrows a lot and blocks blood flow.
How does aortic valve calcification affect life expectancy and quality of life?
It depends on how bad it is. Severe cases can shorten life and lower quality of life. But catching it early and treating it can help a lot.
When should more aggressive intervention be considered for aortic valve calcification?
You should think about more serious treatments if symptoms get worse or if the valve isn’t working right. Tests like echocardiography can show this.
References
- Penn Medicine (Aortic Valve Stenosis) : https://www.pennmedicine.org/conditions/aortic-valve-stenosis
- Dr. Yavuz Beşoğul (Heart Valve Calcification) : https://dryavuzbesogul.com/en/kalp-kapakcigi-kireclenmesi-curumesi
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC4888946
- AHA Journals (Circulation) : https://www.ahajournals.org/doi/10.1161/circulationaha.104.486738
- Vinmec International Hospital (Heart Valve Calcification) : https://www.vinmec.com/eng/blog/heart-valve-calcification-symptoms-and-treatment-en








