At Liv Hospital, we know how vital it is to pick the right treatment for aortic aneurysms. Two common treatments are Thoracic Endovascular Aortic Repair and Endovascular Aneurysm Repair. Both are less invasive, but they treat different conditions in different ways.
We will look at the main differences between these two methods. This will help you decide which one is right for you. Our goal is to give you the best care and advice every step of the way.
Key Takeaways
- Understanding the difference between TEVAR and EVAR Chickenpox Thrombocytopenia: Negative Link Explainedis key for effective treatment.
- Each procedure targets different types of aortic aneurysms.
- The choice between TEVAR and EVAR depends on the aneurysm’s location and size.
- Liv Hospital is committed to providing personalized care for patients with aortic aneurysms.
- Minimally invasive procedures like TEVAR and EVAR offer quicker recovery times.
Understanding Aortic Aneurysms and Endovascular Repair
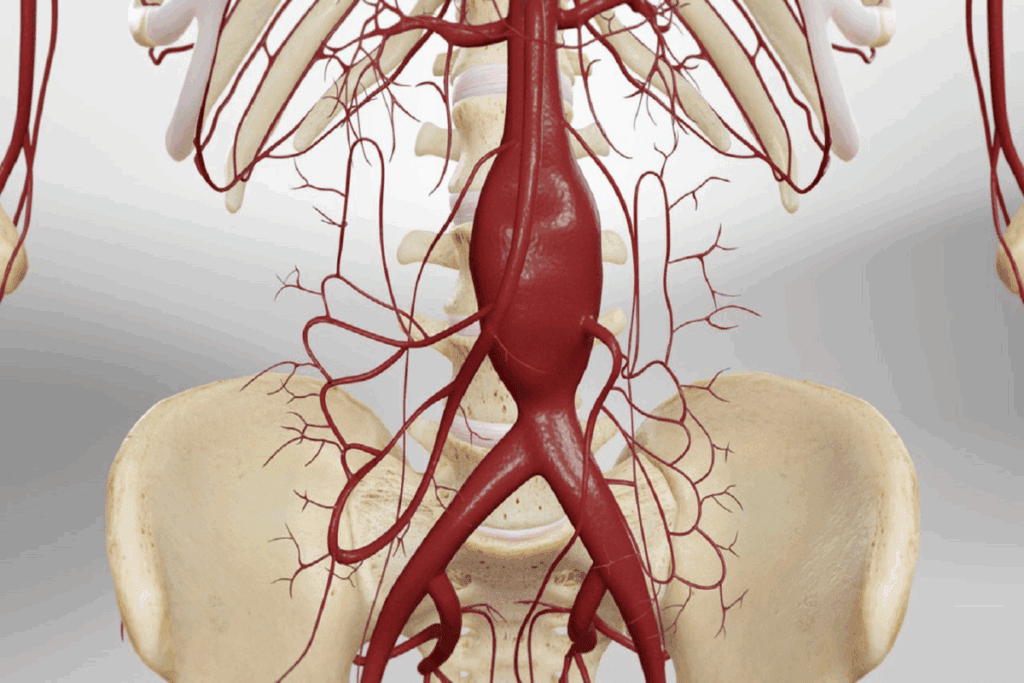
It’s important to know about aortic aneurysms to understand the value of endovascular repair. An aortic aneurysm happens when the aorta, the main artery, weakens and bulges. This can cause serious problems if not treated right.
What Are Aortic Aneurysms?
An aortic aneurysm is when the aorta gets too big. It can happen anywhere along the aorta, from the heart to the abdomen. Often, there are no symptoms, so regular check-ups are key.
Things like smoking, high blood pressure, and family history can increase your risk. Knowing these can help prevent and catch aortic aneurysms early.
Evolution of Endovascular Repair Techniques
Endovascular repair is now the top choice for treating aortic aneurysms. It’s minimally invasive. A stent-graft is put in through small cuts in the groin and guided to the aneurysm site. It then blocks blood flow to the aneurysm.
The better technology and imaging in endovascular repair have made it safer and more effective. This has greatly improved outcomes for patients with aortic aneurysms.
| Technique | Description | Benefits |
| Endovascular Aneurysm Repair (EVAR) | Minimally invasive procedure involving stent-graft placement | Reduced recovery time, lower risk compared to open surgery |
| Thoracic Endovascular Aortic Repair (TEVAR) | Similar to EVAR but focused on thoracic aortic aneurysms | Effective for treating aneurysms in the chest region |
Benefits of Minimally Invasive Approaches
Minimally invasive methods likeendovascular aneurysm repair have many advantages. They lead to shorter hospital stays, less pain, and faster recovery than open surgery.
These advantages make endovascular repair a good choice for those at high risk for open surgery complications. It can improve patients’ quality of life by reducing risks.
What is EVAR? Abdominal Aortic Aneurysm Repair Explained
EVAR, or Endovascular Aortic Aneurysm Repair, is a modern medical procedure. It treats abdominal aortic aneurysms without open surgery. This method is safer and allows for quicker recovery times.
Definition and Purpose of EVAR
EVAR fixes an abdominal aortic aneurysm (AAA) by placing a stent graft in the aorta. It aims to stop the aneurysm from bursting, which can be deadly. EVAR strengthens the aortic wall, lowering the risk of rupture and death.
“EVAR is more common now because it’s less invasive and recovery is faster,” says a top vascular surgeon. This change shows the progress in medical tech and the focus on better patient care.
The AAA EVAR Medical Abbreviation Explained
“AAA EVAR” stands for Abdominal Aortic Aneurysm Endovascular Aneurysm Repair. It’s about using EVAR to treat abdominal aortic aneurysms. Knowing this term is key for doctors and patients looking into aortic aneurysm treatments.
The EVAR Procedure Step-by-Step
The EVAR procedure has several steps:
- Accessing the aorta through small incisions in the groin.
- Guiding a stent graft through the blood vessels to the aneurysm site.
- Deploying the stent graft to strengthen the aorta’s weak spot.
- Checking that the stent graft is firmly in place to avoid leaks or movement.
Ideal Candidates for EVAR
EVAR is best for those at high risk for open surgery or with complex anatomy. Ideal candidates have:
- Aneurysms that fit for endovascular repair.
- Major health issues that raise open surgery risks.
- Anatomy that allows for stent graft placement.
Knowing about EVAR helps patients and doctors choose the best treatment for abdominal aortic aneurysms.
What is TEVAR? Thoracic Endovascular Aortic Repair Explained
The TEVAR procedure is a modern way to fix thoracic aortic aneurysms without open surgery. It’s a less invasive method that has changed how we treat these conditions. It offers a safer option compared to traditional surgery.
Definition and Purpose of TEVAR
TEVAR means Thoracic Endovascular Aortic Repair. It’s a procedure to treat thoracic aortic aneurysms by putting a stent graft in the aorta. The main goal is to stop an aortic aneurysm from bursting by strengthening the aorta’s weak spot.
TEVAR Medical Abbreviation and Terminology
In medical terms, TEVAR is about fixing the thoracic aorta through endovascular repair. Knowing this terminology helps both patients and doctors talk clearly about the procedure and its effects.
The TEVAR Procedure Step-by-Step
The TEVAR procedure has several important steps:
- Accessing the aorta through small incisions in the groin.
- Guiding a stent graft through the blood vessels to the thoracic aorta.
- Deploying the stent graft to reinforce the weakened area of the aorta.
- Ensuring the stent graft is properly positioned and functioning.
This detailed process ensures a precise and effective treatment for thoracic aortic aneurysms.
Ideal Candidates for TEVAR
TEVAR is best for patients at high risk for open surgery or with complex aortic structures. The best candidates have:
- Thoracic aortic aneurysms or dissections.
- Significant comorbidities that increase surgical risk.
- Aortic anatomies that are suitable for endovascular repair.
By knowing what TEVAR is, why it’s done, and how it’s done, patients can make better choices about their treatment.
TEVAR vs EVAR: The 7 Key Differences
It’s important to know the differences between TEVAR and EVAR for treating aortic aneurysms. Both are endovascular techniques, but they are better for different aneurysms and patients. Each has unique features.
1. Anatomical Target Areas: Thoracic vs Abdominal
TEVAR targets the thoracic aorta in the chest. EVAR treats the abdominal aorta in the belly. This difference is key in choosing the right treatment.
- TEVAR is for thoracic aortic aneurysms.
- EVAR is for abdominal aortic aneurysms.
2. Symptom Presentation and Diagnosis
TEVAR and EVAR have different symptoms and diagnosis methods. Thoracic aneurysms might cause back pain or difficulty swallowing. Abdominal aneurysms often don’t show symptoms until they burst.
“The presentation of aortic aneurysms can vary significantly depending on their location, highlighting the need for precise diagnostic imaging.” –
Aortic Aneurysm Treatment Guidelines
3. Procedural Techniques and Access Points
TEVAR and EVAR have different approaches. Both start with the femoral artery in the groin. But, TEVAR’s stent graft must navigate the aortic arch, which is more challenging.
- Both procedures use femoral artery access.
- TEVAR requires more complex stent graft navigation.
4. Risk Profiles and Possible Complications
TEVAR and EVAR are both safe, but they have different risks. TEVAR might lead to stroke due to its closeness to the brain. EVAR’s risks include kidney complications.
Knowing these differences helps manage patient expectations and make informed care decisions.
Common Complications in Endovascular Aortic Repairs
Endovascular aortic repair, like TEVAR and EVAR, has changed how we treat aortic aneurysms. But, these procedures come with their own set of complications. Knowing about these issues is key to taking good care of patients.
Endoleaks: Types and Management
Endoleaks are a big problem with endovascular aortic repair. They happen when blood leaks into the aneurysm sac around the stent graft. There are different types of endoleaks, each needing its own way to manage them.
- Type I: Leak at the attachment site of the stent graft
- Type II: Retrograde flow from branches into the aneurysm sac
- Type III: Leak through a defect in the stent graft
- Type IV: Graft porosity causing leakage
- Type V: Endotension, where the sac expands without visible leak
Dealing with endoleaks often means watching the patient with imaging and sometimes doing more, likeembolization or adding more stent grafts.
| Endoleak Type | Description | Management |
| Type I | Leak at attachment site | Additional stent grafting or ballooning |
| Type II | Retrograde flow from branches | Surveillance or embolization |
| Type III | Leak through graft defect | Additional stent grafting |
Graft Migration Concerns
Graft migration is a big worry. It happens when the stent graft moves from where it was placed. This can cause endoleaks or make it hard to keep the aneurysm sac closed. Things that can make graft migration happen include the wrong size, not fitting right, and blood pressure.
Preventing graft migration means picking the right size and fit for the stent graft. It also means keeping an eye on it over time to make sure it stays in place.
Procedure-Specific Complications
TEVAR and EVAR each have their own complications. TEVAR can cause stroke or spinal cord problems because of where the thoracic aorta is. EVAR might lead to problems with the access vessels, like injury or blockage of the femoral artery.
It’s important to know about these procedure-specific complications to make the best choices for patients and get them the best results.
Patient Selection Criteria: Who Qualifies for EVAR vs TEVAR
Choosing between EVAR and TEVAR depends on a patient’s medical history, body needs, and health issues. We look at many factors to make sure the treatment fits the patient’s health and needs.
Anatomical Requirements
The shape and size of the aneurysm and the patient’s blood vessels are key. EVAR needs a good spot for the stent graft and easy access to the iliac arteries. The aorta should not be too twisted.
- Aneurysm Size and Location: The size and where the aneurysm is matter a lot for EVAR or TEVAR.
- Vascular Anatomy: We check the blood vessels for any blockages or narrowing to ensure the stent graft can be safely placed.
- Landing Zone: A good spot for the stent graft is vital to avoid leaks or the graft moving.
TEVAR needs a long enough section of the aorta for the stent graft and good access points. It’s often used for aortic aneurysms, dissections, or injuries in the chest.
Age and Comorbidity Considerations
Age and health problems are big factors in choosing EVAR or TEVAR. These procedures are safer for older patients or those with many health issues compared to open surgery.
“The decision to proceed with EVAR or TEVAR should be based on a thorough assessment of the patient’s overall health, including their age, comorbidities, and anatomical suitability.”
— Society for Vascular Surgery Guidelines
We look at these health issues when deciding on EVAR or TEVAR:
- Cardiac Disease: Patients with heart problems need careful checks and preparation before surgery.
- Pulmonary Disease: Lung conditions like COPD can make it hard for patients to handle the procedure.
- Renal Function: Kidney problems are important because they can lead to kidney damage from the contrast used in the procedure.
Contraindications for Each Procedure
EVAR and TEVAR are good for treating aortic aneurysms, but each has its own no-go list. Knowing these helps pick the best treatment.
Things that make EVAR not work include:
- Insufficient Landing Zone: Not enough space at the ends of the aneurysm can lead to leaks or the graft moving.
- Significant Iliac Artery Disease: Bad iliac arteries can make it hard to get to the stent graft.
Things that make TEVAR not work include:
- Aortic Arch Pathology: Complex problems in the aortic arch might need different treatments.
- Severe Aortic Tortuosity: Very twisted aortas can make it tough to put in the stent graft.
By carefully looking at these points, we can choose the best treatment for each patient. This ensures the best results for those having EVAR or TEVAR.
Recovery and Follow-up After Endovascular Procedures
Recovery and follow-up care are key for the success of EVAR and TEVAR. Understanding post-procedure care is vital for the best patient outcomes.
Hospital Stay Duration Comparison
The time in the hospital after EVAR and TEVAR varies. Both procedures are shorter than open surgery. EVAR patients usually stay 1 to 3 days. TEVAR patients might stay a bit longer due to the thoracic aortic repair’s complexity.
“The minimally invasive nature of these procedures allows for quicker recovery times,” say vascular surgeons. This shorter stay reduces the risk of infections and complications.
Post-Procedure Pain Management
Managing pain is key in recovery. EVAR patients often feel less pain than those with open repair. TEVAR might need a mix of meds and other methods for thoracic pain.
- Medications: A mix of opioids and non-opioids is used for pain.
- Monitoring: Pain levels are checked regularly to adjust treatment.
- Patient Education: Patients learn to manage pain at home.
Long-term Monitoring Requirements
Long-term follow-up is vital for EVAR and TEVAR success. Regular imaging checks the stent graft and watch for complications. Patients get CT scans at 1, 6, and 12 months, then yearly.
| Timeframe | EVAR Monitoring | TEVAR Monitoring |
| 1 Month | CT Scan | CT Scan |
| 6 Months | CT Scan | CT Scan |
| 1 Year | CT Scan | CT Scan |
Lifestyle Modifications After EVAR and TEVAR
Changing your lifestyle is important for recovery and long-term success. Patients should eat well, exercise, and avoid smoking for vascular health.
“A heart-healthy lifestyle can greatly impact EVAR and TEVAR success,” says a vascular specialist.
Patients should also know the signs of complications and when to seek help. By making these lifestyle changes and following up, patients can improve their outcomes and lower future vascular risks.
Advanced Variants: FEVAR vs TEVAR vs Standard EVAR
Endovascular techniques are getting better, thanks to new methods like FEVAR and branched endografts. These new ways help fix complex aortic aneurysms. They are key for patients with tough aortic shapes.
Fenestrated EVAR (FEVAR) Explained
Fenestrated EVAR, or FEVAR, is a new way to treat aortic aneurysms near important blood vessels. It keeps blood flowing to vital organs. This is because it has small holes in the stent graft.
Key benefits of FEVAR include:
- Preservation of blood flow to critical branch vessels
- Expanded treatment options for patients with complex aortic aneurysms
- Potential for improved outcomes in patients with challenging anatomies
Branched Endografts and Complex Anatomies
Branched endografts are another big step forward in treating complex aortic aneurysms. They have special branches for major blood vessels. This makes repairs more precise and lasting. They work best for aortic aneurysms that span the thoracic and abdominal areas.
| Feature | Standard EVAR | FEVAR | Branched Endografts |
| Anatomical Suitability | Limited to straightforward abdominal aortic aneurysms | Suitable for aneurysms involving critical branch vessels | Ideal for complex thoracoabdominal aortic aneurysms |
| Preservation of Branch Vessels | No | Yes, through fenestrations | Yes, through branches |
Technological Advancements in Stent Graft Design
Stent grafts have gotten a lot better, thanks to new tech. They’re stronger, more flexible, and fit the aorta better. They’re made from advanced materials that last longer. New ways to make them have led to more complex designs, like fenestrated and branched grafts.
“The evolution of stent graft technology has been instrumental in expanding the indications for endovascular aortic repair, enabling us to treat a wider range of patients with complex aortic pathologies.”
— Vascular Surgeon
Imaging and Navigation Improvements
New imaging and navigation tools have helped a lot. High-resolution images, like cone-beam CT, show the aorta and stent graft in detail. Better navigation systems help place stent grafts exactly right, cutting down on risks.
These new tools and stent graft designs have made endovascular repairs better. As tech keeps getting better, we’ll see even more progress in treating complex aortic aneurysms.
Conclusion: The Future of Endovascular Aortic Repair
The field of endovascular aortic repair is changing fast. This is thanks to new technology and techniques. EVAR and TEVAR have made treating aortic aneurysms easier and less invasive than old surgery methods.
Patient results have gotten better, with quicker recoveries and fewer problems. The future looks bright for endovascular aortic repair. We’re seeing more work on better stent grafts, better imaging, and treating more complex cases.
As these new developments keep coming, EVAR and TEVAR will get even better. This means more people will have access to these life-saving treatments. It’s great news for patients all over the world.
FAQ
What is the difference between TEVAR and EVAR?
TEVAR and EVAR are both minimally invasive treatments for aortic aneurysms. TEVAR treats thoracic aortic aneurysms. EVAR treats abdominal aortic aneurysms.
What is EVAR used for?
EVAR treats abdominal aortic aneurysms (AAAs). It uses a stent graft to reinforce the aorta. This prevents further expansion and rupture.
What is TEVAR used for?
TEVAR treats thoracic aortic aneurysms. It places a stent graft in the thoracic aorta. This excludes the aneurysm from blood flow, preventing rupture.
What are the benefits of EVAR and TEVAR compared to open surgery?
EVAR and TEVAR have many benefits over open surgery. They have smaller incisions, less blood loss, and shorter hospital stays. Recovery times are also quicker.
What are the common complications associated with EVAR and TEVAR?
Common complications include endoleaks and graft migration. Endoleaks happen when blood leaks into the aneurysm sac. Graft migration is when the stent graft moves from its original position.
How are endoleaks managed?
Endoleaks are managed based on their type and severity. Some may resolve on their own. Others may need additional interventions, like embolization or additional stent grafts.
What are the criteria for selecting patients for EVAR and TEVAR?
Patient selection criteria include anatomical requirements, age, and comorbidities. Ideal candidates have suitable aortic anatomy and are at high risk for open surgery.
What lifestyle modifications are recommended after EVAR and TEVAR?
Patients should maintain a healthy lifestyle. This includes a balanced diet, regular exercise, smoking cessation, and adherence to prescribed medications. This ensures the best outcomes.
What is FEVAR, and how does it differ from EVAR and TEVAR?
FEVAR is an advanced variant of EVAR. It treats complex aortic aneurysms involving branch vessels. It uses custom-made stent grafts with fenestrations to accommodate these vessels.
What advancements are being made in endovascular aortic repair?
Advances include better stent graft design, imaging navigation, and procedural techniques. These improvements enable the treatment of more complex aortic aneurysms and improve patient outcomes.
Reference
- National Center for Biotechnology Information. (2022). TEVAR and EVAR, the unknown knowns…
https://pmc.ncbi.nlm.nih.gov/articles/PMC9468223