Last Updated on November 27, 2025 by Bilal Hasdemir
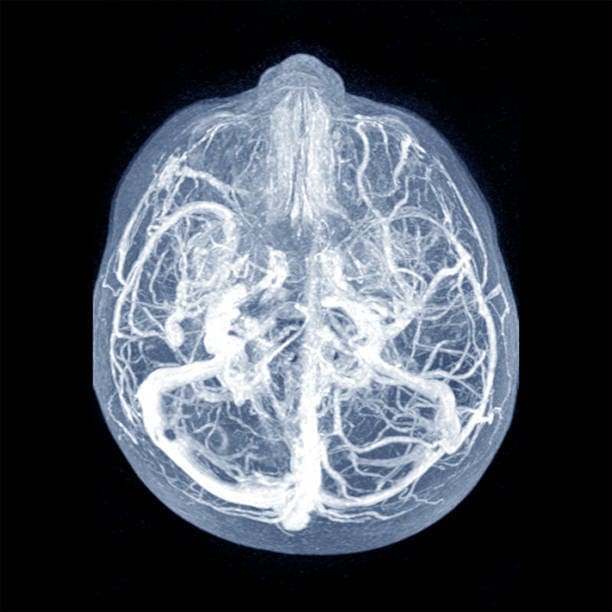
Radiologists have a big role in spotting serious aorta problems like aortic dissection and aneurysms with CT scans. At Liv Hospital, our skilled radiology teams use top-notch CT imaging to find aortic diseases right away. Early detection is key for quick and effective treatment.
CT scans help us see important aorta details, letting us quickly spot acute aortic syndromes. By looking at specific signs, radiologists can make choices that greatly help patients. Our aim is to help radiologists spot the key features that matter for diagnosis and treatment.
Key Takeaways
- CT scans are key for finding aortic diseases.
- Finding aortic problems early helps treatment work better.
- Radiologists should look for specific aorta signs on CT scans.
- Advanced CT imaging makes finding diseases more accurate.
- Liv Hospital’s radiology teams are trained to spot critical aorta signs.
The Critical Role of CT in Aortic Imaging
CT imaging has greatly improved how we diagnose and treat aortic diseases. The latest CT technology makes it a top choice for checking aortic health.
Evolution of CT Technology for Aortic Assessment
CT scans for the aorta have changed a lot over time. We’ve moved from old single-detector scanners to modern multidetector-computed tomography angiography (CTA). This new tech gives us fast, reliable, and non-invasive scans that are almost perfect.
Multidetector CT (MDCT) has been key in this progress. It lets us get clear images of the aorta and its branches.
Advantages of MDCT in Acute Aortic Syndromes
MDCT shines in emergency aortic cases. It quickly checks the aorta, which is vital in urgent situations. Its detailed images help spot intimal flaps, true vs. false lumens, and branch issues.
This is key for spotting aortic dissections and intramural hematomas.
| Advantages of MDCT | Clinical Implications |
|---|---|
| High-resolution imaging | Accurate diagnosis of aortic conditions |
| Rapid assessment | Critical in emergency situations |
| Visualization of intimal flaps and lumen differentiation | Essential for diagnosing aortic dissection and intramural hematoma |
MDCT has changed how we handle acute aortic issues. It gives doctors the tools for quick and precise diagnoses. As CT tech keeps getting better, we’ll see even more progress in treating aortic diseases.
Understanding Normal Aorta on CT Anatomy

CT scans show the aorta in detail. This helps doctors see its normal shape. Knowing what’s normal is key to spotting problems and making the right diagnosis.
Standard Dimensions and Variations
The size of the aorta can differ from person to person. The top part of the aorta is usually about 2.8 cm wide. The lower part is around 2.2 cm. These sizes can change based on age, sex, and body size.
It’s important to know these differences when looking at CT scans. This helps avoid mistaking normal changes for disease.
A study on aortic dimensions shows how knowing normal sizes helps in diagnosing aortic diseases.
- Normal ascending aortic diameter: approximately 2.8 cm
- Normal descending thoracic aortic diameter: approximately 2.2 cm
- Variations due to age, sex, and body size
Age-Related Changes in Aortic Appearance
As people get older, the aorta changes. These changes include a bigger diameter and the buildup of plaques. It’s important to know these changes to tell normal aging from disease.
In older adults, the aorta might look more twisted or have more plaque. These are normal signs of aging. But, big differences from what’s expected should lead to more tests.
Optimal CT Protocols for Aortic Evaluation
When we use CT scans to check the aorta, the protocol matters a lot. A good CT protocol helps us see aortic problems clearly. It also helps us decide the best treatment.
Contrast Administration Techniques
How we give contrast is key for aortic CT scans. We use a bolus tracking technique for the best contrast. This means we watch the contrast as it moves through the aorta. Then, we start the scan when it’s at its peak.
The contrast agent and how fast we inject it matter a lot. We usually use a high-flow rate (4-6 mL/s) for good aortic pictures. The amount of contrast we use depends on the patient’s size and the protocol.
Timing and Phase Considerations
A good CTA for the aorta has several phases: unenhanced, arterial, and delayed. The unenhanced phase shows calcifications and helps us see how well the contrast works.
The arterial phase captures the aorta at its best, showing the inside and branches clearly. The delayed phase is for spotting problems like endoleaks.
| Phase | Purpose | Timing |
|---|---|---|
| Unenhanced | Identify calcifications, baseline enhancement | Pre-contrast |
| Arterial | Visualize aortic lumen and branch vessels | Peak aortic enhancement |
| Delayed | Detect endoleaks or complications | Variable, post-contrast |
By fine-tuning our CT protocols, we get top-notch images for aortic checks. This includes how we give contrast and when we take the pictures.
Feature 1: Intimal Flap Visualization
CTA has changed how we diagnose aortic dissections. It lets us see the intimal flap and how far it goes. The intimal flap is key because it divides the true lumen from the false lumen in aortic dissections.
Characteristic Appearances and Variations
The intimal flap looks like a thin, straight line in the aortic lumen on CT scans. Its look can change based on how it’s lined up with the scan. If it’s straight with the scan, it looks like a clear line. But if it’s at an angle, it might look like a circle or oval.
It’s easy to confuse the intimal flap with other things or artifacts. So, we need to look at images from different angles and times carefully.
| Characteristics | Description | Imaging Findings |
|---|---|---|
| Orientation | Parallel or perpendicular to the imaging plane | Linear lucency or circular/oval structure |
| Location | Within the aortic lumen | Separates true and false lumens |
| Appearance | Thin, linear structure | Visible on CT images, specially with contrast |
Common Pitfalls in Identification
One big mistake is thinking the intimal flap is an artifact or a problem with the aortic wall. Motion artifacts can look like the intimal flap. We must look at images from different angles and use ECG gating to avoid these mistakes.
Another problem is when the false lumen is filled with blood clots. This can hide the intimal flap. In these cases, we need to closely examine the aortic wall and the areas around it.
Knowing how the intimal flap looks and the common mistakes helps us get better at spotting it on CT scans. This improves how we care for our patients.
Feature 2: True vs. False Lumen Differentiation
Being able to tell true from false lumens on CT scans is key for treating aortic dissection. Knowing which is which helps doctors decide the best course of action. This choice can greatly affect how well a patient does.
Diagnostic Criteria and Imaging Signs
There are several ways to tell true from false lumens on CT scans. These include:
- The beak sign: A flap that looks like a beak, forming a sharp angle with the false lumen.
- The cobweb sign: Thin, dark lines in the false lumen.
- The false lumen is usually bigger and more uneven than the true lumen.
- How the contrast material shows up can also help tell them apart.
It’s important for radiologists to know these signs when looking at CT scans of aortic dissections.
Clinical Implications of Accurate Differentiation
Knowing the difference between true and false lumens is very important. It helps doctors decide if they should use a stent-graft. They need to know which lumen to use for access and make sure the stent-graft is in the right place.
| Feature | True Lumen | False Lumen |
|---|---|---|
| Size | Typically smaller | Often larger |
| Shape | More regular | More irregular |
| Beak Sign | Absent | Present |
| Cobweb Sign | Absent | Present |
Being able to spot true and false lumens on CT scans is a big deal for managing aortic dissections. It helps not just in diagnosing but also in planning treatment. This can lead to better outcomes for patients.
Feature 3: Aortic Diameter Measurement Techniques
Measuring the aortic diameter accurately is key for making medical decisions. It helps spot aneurysms and track their growth.
Standardized Measurement Approaches
We follow set methods to measure the aortic diameter. CT scans with multiplanar reconstruction (MPR) help us get precise measurements. We measure the diameter straight across the aorta, avoiding any angles.
Key considerations for standardized measurement include:
- Using the outer-to-outer wall measurement technique
- Avoiding measurements during systole or diastole when the aorta is under different pressures
- Ensuring the measurement is taken at the correct anatomical location
Threshold Values for Intervention
Knowing when to intervene is vital for aortic aneurysm management. The size at which surgery is needed depends on the aorta’s location and the patient’s health.
An abdominal aortic aneurysm (AAA) might need repair at 5.5 cm in men and 5 cm in women. But, these sizes can change based on the patient’s risk factors and symptoms.
Clinical guidelines recommend:
| Location | Diameter Threshold |
|---|---|
| Abdominal Aorta | 5.5 cm (men), 5 cm (women) |
| Thoracic Aorta | Varies by segment; typically 6-7 cm |
By sticking to these measurement methods and knowing when to intervene, we can give the best care to patients with aortic aneurysms.
Feature 4: Mural Thrombus Assessment
We look closely at mural thrombus in aortic aneurysms. This blood clot inside the aneurysm sac is key to understanding risk and treatment. Its details greatly affect how well a patient will do.
Imaging Characteristics of Thrombus
CT scans show mural thrombus as a darker area inside the aneurysm. It often looks like a crescent or goes all the way around. We check its size, where it is, and what it looks like with CT scans.
The look of mural thrombus changes with age and type. Newer clots are more uniform and less dense. Older clots get more mixed up and might even get calcium deposits.
Prognostic Significance
The type and size of mural thrombus matter a lot for patients with aortic aneurysms. Research shows that how big and where the thrombus is can change the risk of rupture. It also affects how well endovascular repair might work.
| Thrombus Characteristic | Prognostic Implication |
|---|---|
| Large thrombus burden | Increased risk of rupture |
| Thrombus heterogeneity | Potential for embolic events |
| Thrombus calcification | Chronicity and stability |
By looking at mural thrombus with CT scans, we get a clearer picture of the risks. This helps us plan the best treatment. Knowing this is key to making good choices for patients and improving their chances of a good outcome.
Feature 5: Branch Vessel Involvement
Branch vessel involvement is a key part of checking aortic dissection and aneurysm on CT scans. It’s important to look at major aortic branches to see how severe the disease is. This helps decide the best treatment.
Evaluation of Major Aortic Branches
We focus on big aortic branches like the brachiocephalic trunk, left common carotid artery, and left subclavian artery. CT angiography of the aorta gives us clear images of these. This lets us see how they’re affected by aortic disease.
The condition of these branches is very important for treating aortic problems. For example, if the brachiocephalic trunk is involved, it could affect blood flow to the right arm and brain. This means we need to plan carefully for any treatment.
| Branch | Normal Function | Impact of Involvement |
|---|---|---|
| Brachiocephalic Trunk | Supplies right arm and head | Potential reduction in blood flow to right arm and brain |
| Left Common Carotid Artery | Supplies left side of the brain | Risk of cerebral ischemia or stroke |
| Left Subclavian Artery | Supplies left arm | Potential reduction in blood flow to left arm |
Impact on Management Decisions
The extent of branch vessel involvement greatly affects how we manage aortic disease. Accurate assessment is key to picking the right treatment. This could be surgery, endovascular repair, or just watching it closely.
For instance, if a dissection affects a branch, we might choose surgery or endovascular repair to fix it.
In summary, checking branch vessel involvement is vital in aortic CT imaging. By looking at major aortic branches and their role in disease, we can make better decisions for our patients.
Feature 6: Signs of Impending or Active Rupture
CT scans can show signs of aortic aneurysm or dissection rupture. These signs mean a patient needs urgent medical help. Spotting them early can save lives.
Direct and Indirect Signs of Rupture
Direct signs include contrast leaking out or a clear rupture spot. Indirect signs might show a bright crescent in the aortic wall. This could mean blood is leaking into the wall.
Direct Signs: Seeing contrast leaking out means a rupture is happening now. It’s a sign to act fast. A clear rupture spot also means quick action is needed.
Indirect Signs: A bright crescent in the aortic wall is a warning sign. Other signs include a draped aorta or a contained rupture.
Emergency Management Considerations
If a rupture sign is seen, act fast. Tell the surgery team right away. Get ready for possible surgery.
| Signs | Description | Management |
|---|---|---|
| Contrast Extravasation | Definitive indicator of active rupture | Immediate surgical intervention |
| High-Attenuating Crescent Sign | Indicates hemorrhage into the mural thrombus or wall | Urgent surgical consultation |
| Draped Aorta Sign | Suggests contained rupture | Emergency surgical evaluation |
Good communication between radiologists and doctors is key. It helps patients get the care they need quickly.
Feature 7: Advanced Aorta on CT Findings in Complex Cases
In complex aortic cases, advanced CT findings are key for accurate diagnosis and treatment planning. These imaging techniques help guide our clinical decisions.
Post-Surgical Appearances
After aortic surgery, CT imaging is vital for monitoring recovery and spotting complications. Post-surgical appearances can differ a lot based on the surgery type.
For example, after fixing an aortic dissection, CT scans can reveal the repaired aortic segment. They can also show leaks or other issues.
Inflammatory Aortic Conditions
Inflammatory conditions like aortitis can be hard to diagnose. Advanced CT imaging spots inflammatory changes in the aortic wall.
CT scans might show wall thickening, enhancement, or other signs of inflammation. Getting an accurate diagnosis is key for managing these conditions well.
Congenital Anomalies
Congenital anomalies of the aorta pose unique diagnostic challenges. Advanced CT imaging lets us see these anomalies in detail.
Common anomalies include coarctation of the aorta and right-sided aortic arch. Knowing about these anomalies is vital for planning the right treatment.
Recent Advances in Aortic CT Imaging Research
The field of aortic CT imaging is growing fast. New methods are making it easier to see how aortic diseases progress. These advancements are changing how we diagnose and treat aortic diseases.
Improved Accuracy in Lumen Differentiation
One key area of research is making lumen differentiation more accurate. This means being able to tell the true and false lumens apart in aortic dissections. Advanced CT scans, like dual-energy CT, are helping a lot here.
New imaging algorithms are also helping. They can spot and understand the intimal flap, a key sign of aortic dissections. With these tools and high-resolution scans, doctors can now see the aorta more clearly.
| Technique | Advantages | Clinical Impact |
|---|---|---|
| Dual-Energy CT | Enhanced contrast resolution, better tissue characterization | Improved diagnosis of aortic dissections and characterization of lumens |
| Advanced Imaging Algorithms | More accurate identification of intimal flaps and assessment of aortic wall | Better treatment planning and monitoring of disease progression |
Predictive Imaging Biomarkers for Disease Progression
Researchers are also working on finding biomarkers for disease progression. By looking at CT scans, they can spot signs that tell them how a disease will grow. This helps doctors plan treatments earlier and more precisely.
Now, CT scans can show more than just the aorta’s shape. They can also show how well the aorta is working. This includes checking if aortic stenosis is serious or if an aneurysm might burst. These biomarkers give doctors important clues about what might happen next.
As we keep improving aortic CT imaging, we’ll see even better tools. The use of artificial intelligence and machine learning in CT scans is very promising. It could make aortic imaging even more accurate and helpful.
Liv Hospital’s Approach to Excellence in Aortic Imaging
At Liv Hospital, we focus on multidisciplinary collaboration and innovation. We know that treating aortic conditions needs a mix of the latest tech and expert opinions. This approach helps us give the best care to our patients.
Multidisciplinary Collaboration in Aortic Disease Management
We believe teamwork is key for aortic disease treatment at Liv Hospital. Our team includes radiologists, cardiologists, and vascular surgeons. They work together to create treatment plans tailored for each patient.
Advanced imaging, like CT angiography aorta, is vital for us. It gives us clear images of the aorta. This helps us understand the disease better and decide on the best treatment.
Implementation of Academic Standards and Innovation
Liv Hospital aims for the highest standards in aortic imaging. We keep up with new research and education. This keeps us ahead in the field and allows us to use the latest tech.
Our goal is to offer accurate diagnoses and effective treatments. We use the latest technology to help our patients. Our mission is to provide top-notch healthcare to everyone, including international patients.
Conclusion: Integrating CT Findings into Clinical Practice
Accurate diagnosis of aortic diseases depends a lot on CT imaging. We’ve talked about how CT is key in aortic imaging. It’s important to know the aorta’s anatomy and the best CT protocols for checking the aorta.
There are seven key things radiologists should look for on a CT scan of the aorta. These include seeing the intimal flap, telling true from false lumen, measuring the aorta’s diameter, checking for mural thrombus, and looking at branch vessel involvement. They also need to spot signs of rupture and advanced findings in complex cases.
At Liv Hospital, we make sure CT findings are used in patient care. Our radiologists and clinicians work together to give the best care for aortic disease patients. We use the latest in CT imaging and a team approach to offer top-notch healthcare to our patients from around the world.
Using CT findings well helps us quickly spot serious issues like aortic dissection and aneurysm. This leads to better patient outcomes. We keep getting better at understanding aorta CT anatomy and interpreting CT scans of the aorta. This helps us excel in diagnosing and treating aortic diseases.
FAQ
What is the importance of CT imaging in diagnosing aortic diseases?
CT imaging is key in spotting aortic diseases. It gives clear images of the aorta and its branches. This helps find issues like aneurysms, dissections, and ruptures.
What are the 7 key features to look for when evaluating the aorta on CT scans?
When checking the aorta on CT scans, look for seven important things. These include seeing the intimal flap, telling true from false lumen, measuring the aorta’s diameter, and checking for mural thrombus. Also, look at branch vessel involvement, signs of rupture, and advanced aorta findings in complex cases.
How has CT technology evolved for aortic assessment?
CT technology has grown a lot for checking the aorta. Multi-detector CT (MDCT) now gives high-resolution images. This helps accurately diagnose acute aortic syndromes.
What are the advantages of MDCT in diagnosing acute aortic syndromes?
MDCT has many benefits for diagnosing acute aortic syndromes. It offers high spatial resolution and quick scanning. It can also image the whole aorta and its branches in one breath-hold.
What are the standard dimensions and variations of the normal aorta on CT scans?
The normal aorta’s diameter changes along its length. The ascending aorta is usually bigger than the descending aorta. Age can also change how the aorta looks on CT scans.
How should CT protocols be optimized for evaluating the aorta?
For the best CT scans of the aorta, consider how to give contrast. Think about timing and phase to see the aorta and its branches well.
What are the characteristic appearances and variations of the intimal flap on CT scans?
The intimal flap looks like a thin line on CT scans. It separates the true and false lumens. Its look changes based on where and how far the dissection is.
How can true and false lumens be differentiated on CT scans?
To tell true from false lumens on CT scans, look for certain signs. Check for intimal calcification, the lumen’s shape, and any thrombus.
What are the clinical implications of accurate differentiation between true and false lumens?
Knowing the difference between true and false lumens is very important. It helps decide the best treatment and if surgery is needed.
How is aortic diameter measured on CT scans?
Aortic diameter is measured in a standard way on CT scans. Use multi-planar reformations and measure the biggest diameter across the aorta.
What are the threshold values for intervention based on aortic diameter?
When to intervene depends on the aneurysm’s size and location. Symptoms also play a role. Generally, diameters over 5.5 cm might need intervention.
What is the prognostic significance of mural thrombus on CT scans?
Mural thrombus means a higher risk of blood clots and rupture. It’s a key finding on CT scans that needs attention.
How does branch vessel involvement impact management decisions?
Branch vessel involvement affects treatment plans. It might mean needing to fix or bypass blood vessels to keep organs supplied.
What are the signs of impending or active rupture on CT scans?
Signs of rupture include seeing contrast outside the aorta and a crescent sign. These show a high risk of rupture.
What are the advanced aorta on CT findings in complex cases?
In complex cases, look for post-surgical changes, inflammatory conditions, and congenital anomalies. These need careful review and matching with the patient’s history.
What recent advances have been made in aortic CT imaging research?
New research has improved at telling true from false lumens and finding predictive signs. These advances could help better diagnose and manage aortic diseases.
How does Liv Hospital approach excellence in aortic imaging?
Liv Hospital focuses on top-notch aortic imaging through teamwork and innovation. They aim for the highest quality care for aortic disease patients.
References
- Rajiah, P. (2013). CT and MRI in the evaluation of thoracic aortic diseases. International Journal of Vascular Medicine, 2013, 797189. https://doi.org/10.1155/2013/797189 PubMed
- Valente, T., Sica, G., Bocchini, G., Romano, F., Lassandro, F., Rea, G., Muto, E., Pinto, A., Iacobellis, F., & Crivelli, P. (2022). MDCT imaging of non-traumatic thoracic aortic emergencies. European Journal of Radiology Open, 9, 100396. https://doi.org/10.1016/j.ejro.2022.100396 PMC
- Valente, T., Sica, G., Bocchini, G., Romano, F., Lassandro, F., Rea, G., Muto, E., Pinto, A., Iacobellis, F., & Crivelli, P. (2016). MDCT evaluation of acute aortic syndrome. European Journal of Radiology Open, 3, 100-107. https://doi.org/10.1016/j.ejro.2016.02.002 Europe PMC
- Rajiah, P. (2013). CT and MRI in the evaluation of thoracic aortic diseases. International Journal of Vascular Medicine, 2013, 797189. https://doi.org/10.1155/2013/797189 Europe PMC
- Radiopaedia.org. (n.d.). CT abdominal aorta protocol and US. Retrieved October 23, 2025, from https://radiopaedia.org/articles/ct-abdominal-aorta-protocol-and-us