At Liv Hospital, we get it. You might worry about cardiac stents and how they affect your heart. These small, mesh tubes help open up narrowed or blocked arteries. This lets blood flow better to your heart.
There’s no strict limit on how many stents you can have. It really depends on how severe your coronary artery disease is. We look at many factors, like your heart’s shape and the location of the blockages, to provide the best care. Many patients wonder, “how many cardiac stents can you have?” — the number varies for each individual, and doctors decide based on your overall heart health and long-term safety.
Key Takeaways
- The safety of having multiple cardiac stents depends on several factors, including the severity of coronary artery disease.
- Cardiac stents are used to improve blood flow to the heart by opening blocked or narrowed arteries.
- Personalized care at Liv Hospital involves assessing individual anatomy and blockage complexity.
- The decision to place multiple stents is made on a case-by-case basis, considering overall heart health.
- Advanced medical treatments and support services are available for international patients.
Understanding Cardiac Stents and Their Purpose
Cardiac stents are small, mesh-like tubes that help keep arteries open. They ensure healthy blood circulation. A heart stent, or coronary stent, is placed in arteries that supply blood to the heart.
What Are Cardiac Stents?
Cardiac stents are made from metal mesh. They can be compressed into a small size for insertion. Once in place, they expand to a larger size to keep the artery open.
The main job of a cardiac stent is to:
- Keep the artery open after angioplasty
- Improve blood flow to the heart muscle
- Reduce symptoms of coronary artery disease, such as chest pain
How Stents Work to Treat Coronary Artery Disease
Coronary artery disease happens when arteries narrow or block due to plaque buildup. Stents help by:
- Being inserted into the narrowed or blocked artery
- Expanding to push aside the plaque and stretch the artery open
- Remaining in place to keep the artery open, improving blood flow
Knowing how stents work helps patients understand their benefits and outcomes. This treatment is key in managing coronary artery disease.
The Basics of Stent Placement Procedures
Cardiac stent placement is a key part of modern heart care. It’s a minimally invasive method that has changed how we treat heart issues. We’ll explain the steps and the various stent types available.
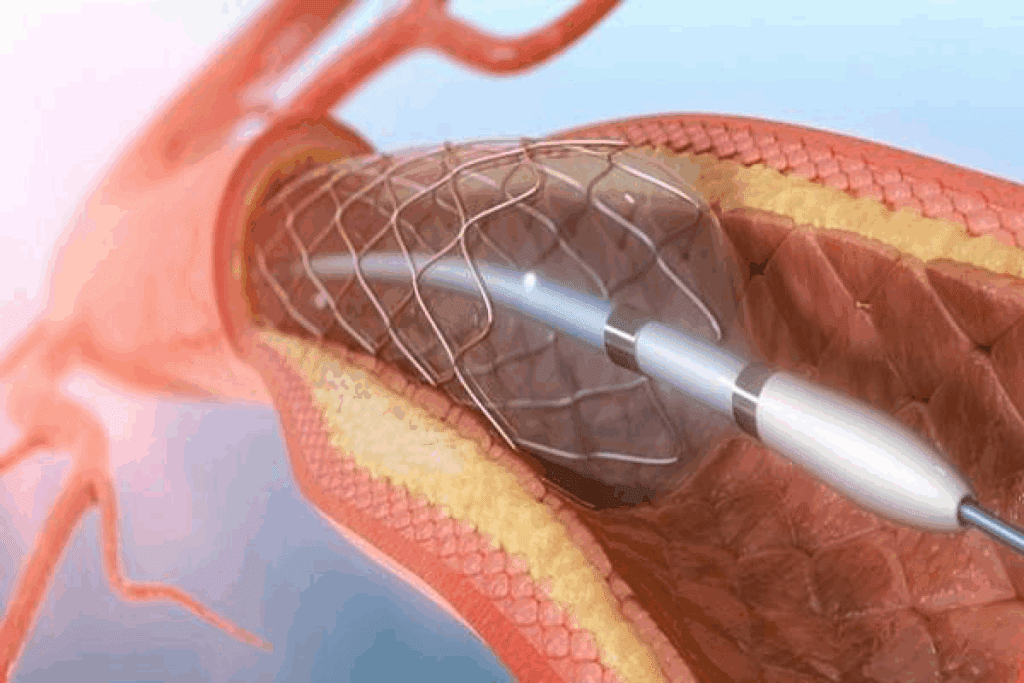
Angioplasty and Stent Insertion Process
Stent placement often happens during an angioplasty. A thin tube, or catheter, with a balloon and stent, is inserted into an artery. This is usually done through the wrist or groin and guided to the heart.
Once in place, the balloon is inflated. This expands the stent against the artery walls. This improves blood flow.
The procedure is done under local anesthesia. Patients are often awake. It can take from 30 minutes to several hours, depending on the case.
Types of Cardiac Stents Available
There are many cardiac stents, each with its own benefits.
| Stent Type | Description | Benefits |
| Bare-Metal Stents | Made from metal mesh | Less expensive, easier to insert |
| Drug-Eluting Stents | Coated with medication to prevent restenosis | Reduced risk of artery re-narrowing |
| Bioresorbable Stents | Made from materials that dissolve over time | Reduces long-term complications, restores natural artery function |
Knowing about the different stents and how they’re placed helps patients make better choices. Our medical team is here to guide and care for you every step of the way.
How Many Cardiac Stents Can You Have?
It’s important to know how many cardiac stents you can have. This depends on your heart disease, your body’s shape, and your heart health.
Medical Perspective on Stent Quantity
Doctors can’t predict exactly how many stents you’ll need. Some people might only need one, while others might need several.
Doctors look at many things to decide how many stents you need. They consider where and how bad the blockages are, your overall health, and your medical history.
Documented Cases from 2 to 35+ Stents
There are records of people having 2, 3, 4, 5, or even more than 6 stents. Some cases show patients with up to 35 stents.
| Number of Stents | Typical Patient Profile | Considerations |
| 1-2 Stents | Patients with localized blockages | Minimally invasive procedure, quick recovery |
| 3-5 Stents | Patients with multiple blockages | More complex procedure, higher risk of complications |
| 6+ Stents | Patients with severe coronary artery disease | High-risk procedure requires careful monitoring and follow-up |
Typical Scenarios for Multiple Stent Patients
People needing many stents often have serious heart disease. They might also have high blood pressure or other heart problems.
In some cases, doctors might place stents in stages. This means doing it in separate times to lower risks.
Factors That Determine the Number of Stents Needed
Many things decide how many stents a patient needs. The disease’s complexity, the patient’s body shape, and their heart health are all important. These factors help doctors figure out how many stents are needed.
Severity and Location of Coronary Blockages
The size and where blockages in the heart’s arteries matter a lot. Patients with many blockages or tricky ones might need more stents. This ensures blood flows well.
Key considerations include:
- The number of blocked arteries
- The severity of the blockages
- The location of the blockages within the coronary arteries
For example, someone with blockages in different arteries might need several stents. This helps fix each blockage well.
Individual Anatomy Considerations
Every person’s heart is different, affecting how many stents they need. Things like artery size and any heart shape issues can change stent placement.
Knowing these differences helps doctors plan treatments that fit each patient’s needs.
Overall Cardiovascular Health
A patient’s heart health is also key in deciding on stents. Conditions like high blood pressure, diabetes, and high cholesterol can make heart disease more complex. This might mean more stents are needed.
| Cardiovascular Health Factor | Impact on Stent Number |
| Hypertension | May require more stents due to increased disease severity |
| Diabetes | Can lead to more complex coronary artery disease |
| High Cholesterol | May necessitate additional stents to manage blockages |
Doctors consider these factors to create a treatment plan that meets each patient’s needs. This approach aims to improve outcomes.
Common Multiple Stent Scenarios
Many patients face the reality of needing multiple stents. This is often due to widespread coronary artery disease. We’ll look at the scenarios for patients with 2-3, 4-5, and 6 or more stents. We’ll discuss the outcomes and what to consider in each case.
Patients with 2-3 Stents: Outcomes and Considerations
Getting 2-3 stents is common for treating coronary artery disease. These patients usually see big improvements in symptoms and quality of life. Studies have shown a decrease in angina symptoms and better heart function.
For those with 2-3 stents, it’s important to:
- Stick to medication to prevent clots and restenosis
- Make lifestyle changes like diet, exercise, and quitting smoking
- Go to regular check-ups to watch the stent’s health and heart condition
Patients with 4-5 Stents: What to Expect
Requiring 4-5 stents is more complex. Yet, many patients see good outcomes. It’s essential for them to work closely with their healthcare team.
Key points for patients with 4-5 stents include:
- Watch for complications like restenosis or stent thrombosis
- Optimize medical therapy to control symptoms and stop disease growth
- Discuss the pros and cons of staged versus simultaneous stent placement
Cases with 6 or More Stents: Special Considerations
Having 6 or more stents is rare but can happen in severe cases. Special considerations are needed for these patients, as risks are higher.
For patients with 6 or more stents, it’s vital to:
- Regularly review and adjust their treatment plan as needed
- Be aware of the increased risk of restenosis and other complications
- Consider alternative treatments or hybrid approaches with their cardiologist
Placement Patterns: How Stents Are Distributed in the Heart
Coronary artery disease treatment often means placing stents in different heart arteries. The stent placement depends on the blockage’s location and how severe it is.
Stent Placement in Different Coronary Arteries
The heart has three main arteries: the left anterior descending (LAD), the left circumflex (LCx), and the right coronary artery (RCA). Stents go in these arteries based on where blockages are. For example, a big blockage in the LAD might be treated with a stent to improve blood flow.
Each artery supplies different heart parts. So, stents are spread out to make sure the heart gets enough blood. Doctors decide where to put stents based on what they see in angiograms and the patient’s symptoms.
Multiple Stents in a Single Artery
Sometimes, a single artery needs more than one stent because of multiple blockages or long disease segments. This is key for complex lesions that can’t be fixed with one stent.
Putting multiple stents in one artery needs careful planning. It’s important to make sure the stents fit right together and cover the area well to avoid restenosis. The length and complexity of the blockage, along with the patient’s heart anatomy, play big roles in this decision.
Maximum Stents Per Artery: Safety Considerations
There’s no hard limit on stents in one artery, but safety matters. The total stented length, lesion complexity, and patient health are all important. These factors help decide if it’s safe to use more stents.
More stents mean a higher risk of problems like restenosis or stent thrombosis. So, doctors carefully weigh the benefits of opening up blocked arteries against the risks. They use advanced imaging and tests to help make these tough choices.
Safety Considerations with Multiple Stents
Understanding the safety of multiple stents is key for both patients and doctors. More stents are used to treat heart disease. This raises questions about their safety.
Short-Term Risks of Multiple Stent Procedures
Using more stents can lead to short-term problems. These include:
- Bleeding or hematoma at the catheter site
- Allergic reactions to the stent material or medications used during the procedure
- Acute stent thrombosis, a condition where a blood clot forms inside the stent
But these risks can be lowered. This is done through careful patient choice, precise procedure, and good care after the procedure.
Long-Term Outcomes with Multiple Stents
The long-term safety of multiple stents is a big worry. Studies show that patients with more stents face higher risks of:
- Restenosis, or the re-narrowing of the arteries
- Stent failure, requiring additional interventions
But new stent technologies, like drug-eluting stents, have helped. They lower the chance of restenosis.
Comparing Safety Profiles: Few vs. Many Stents
The safety of multiple stents versus fewer is complex. More stents can make procedures more complex and riskier. Yet, they might be needed for the best heart disease treatment.
Patients with more heart disease might need more stents. It’s important to weigh the benefits of treating all heart disease against the risks.
Key findings include:
- The risk of complications increases with the number of stents placed.
- Careful patient selection and personalized treatment plans can help minimize risks.
- Ongoing monitoring and follow-up care are key for managing patients with multiple stents.
Healthcare providers can better advise patients on the safety of multiple stents. This ensures patients make informed choices and get the best care.
The Risk of Restenosis with Multiple Stents
Using multiple stents can lead to restenosis, a big worry. Restenosis is when arteries narrow again after a stent is placed. This can make the stent less effective.
Understanding Restenosis
Restenosis happens when the artery grows new tissue around the stent. This can narrow the artery again. Many things can affect this, like the stent type, where it’s placed, and the patient’s health.
Types of Restenosis: There are two main types. In-stent restenosis happens inside the stent. Edge restenosis happens at the stent’s edges.
Research on Restenosis Rates with 3-5 Stents vs. 1-2 Stents
Studies show patients with 3 to 5 stents face a higher restenosis risk. They are 2.2 times more likely to experience stent restenosis than those with 1 or 2 stents.
Comparative studies stress the need to watch patients with multiple stents for restenosis signs.
Preventive Measures for Patients with Multiple Stents
To lower restenosis risk, several steps can be taken. These include:
- Lifestyle changes like diet and exercise
- Medicines to stop clots and lower restenosis risk
- Regular check-ups to watch the stents
We stress the need for a detailed care plan for patients with multiple stents. Knowing the risks and taking early steps can help improve outcomes and lower complication chances.
Simultaneous vs. Staged Stent Placement
Choosing between placing multiple stents at once or in stages is a big decision. It depends on the patient’s health, the blockages’ severity and location, and the arteries’ shape.
Benefits and Risks of Placing Multiple Stents at Once
Putting in multiple stents at once has its perks. It means fewer procedures, which can lower risks. It also means a quicker recovery, as you only need to go through one procedure.
But there are downsides. The procedure might take longer and be more complicated. This could raise the risk of problems. There’s also a bigger chance of kidney damage from the dye used.
Key Considerations for Simultaneous Stent Placement:
- Patient’s overall cardiovascular health
- Number and location of blockages
- Complexity of the procedure
Advantages of Staged Procedures Over Time
Staged stent placement means doing each stent in a separate visit. This way, doctors can check how each stent works before adding more. It’s a safer, more controlled method.
One big plus is the lower risk of problems from longer procedures. It also helps manage dye better, cutting down on kidney risks.
“Staged procedures provide a more controlled environment for managing complex coronary artery disease, allowing for adjustments based on the patient’s response to each intervention.”
When Doctors Choose Each Approach
Doctors pick between simultaneous and staged stent placement based on several things. These include the patient’s condition, the arteries’ complexity, and the doctor’s experience.
| Factor | Simultaneous Placement | Staged Placement |
| Procedure Complexity | Higher complexity | Lower complexity per session |
| Recovery Time | Single recovery period | Multiple recovery periods |
| Risk of Complications | Potentially higher | Potentially lower |
In the end, the choice between simultaneous and staged stent placement is made for each patient. It’s based on their unique situation and needs.
Alternative Treatments When Multiple Stents May Not Be Ideal
In some cases, using multiple stents isn’t the best option. For patients with complex heart disease, other treatments might be better.
Bypass Surgery as an Alternative
Coronary artery bypass grafting (CABG) is a surgery for complex heart issues. CABG creates a new path for blood to flow around blocked areas. This helps the heart muscle get the blood it needs.
We suggest CABG for patients with:
- Multiple blockages in key areas
- Complex heart anatomy
- Diabetes and heart disease in multiple vessels
Medical Management Options
For some, a mix of medicines and lifestyle changes is best. Medical management aims to control symptoms and slow disease growth. It includes:
- Antiplatelet therapy
- Medicines to lower cholesterol
- Managing blood pressure
- Changes in diet, exercise, and quitting smoking
Hybrid Approaches: Combining Stents with Other Treatments
At times, a hybrid method is used. This combines stents with other treatments like CABG or medicines. This method tailors treatment to each patient’s needs. For instance, a stent might be used for a critical blockage, while CABG is done for other blockages.
We look at hybrid treatments for patients with:
- Complex heart disease in multiple vessels
- Blockages after previous CABG
- High risk for stents or CABG alone
Exploring these alternatives helps us create a care plan that fits each patient’s unique situation. This is true whether they have 5 stents in their heart or are at risk for needing more.
Conclusion: What Patients Should Know About Multiple Stents
Knowing how many stents a heart can safely hold is key to managing heart disease. The number of stents needed varies a lot. It depends on the blockages and the person’s heart health.
We’ve looked at what affects the decision to use more than one stent. It’s not the same for everyone. The number of stents depends on the blockages, the heart’s shape, and the person’s health.
Having more than one stent is a big decision. It needs careful thought and care tailored to each person. Studies show that using multiple stents can be safe and effective for many patients.
In short, the number of stents a heart can have depends on many things. It’s important to think about each person’s situation and the doctor’s advice. This way, patients can make smart choices about their treatment.
FAQ
How many cardiac stents can a person have?
The number of stents a person can have varies. It depends on their disease severity, anatomy, and health. We look at these factors to decide the right number for each patient.
What determines the number of stents needed?
The number needed depends on the blockage’s severity and location, anatomy, and health. We evaluate these to choose the best number of stents for each patient.
Can you have multiple stents in one artery?
Yes, multiple stents can be placed in one artery. But we carefully consider the risks, like restenosis, before doing so.
How many stents can be placed at one time?
The number placed at once varies. It depends on the procedure’s complexity and the patient’s health. We weigh the risks and benefits to decide the best approach.
What are the risks associated with having multiple stents?
Multiple stents carry short-term and long-term risks. These include procedure complications and restenosis. We talk about these risks and take steps to prevent them.
Is it safe to have 4 or 5 stents in the heart?
Having 4 or 5 stents can be safe if planned carefully. We consider individual factors and closely monitor patients for the best outcomes.
What are the alternatives to having multiple stents?
Alternatives include bypass surgery, medical management, and hybrid treatments. We discuss these options with patients to find the best treatment plan.
Can you have 6 or more stents in your heart?
Having 6 or more stents is possible but requires careful planning. We assess individual factors and consider alternatives for the best outcome.
How do stents work to treat coronary artery disease?
Stents keep arteries open to ensure blood flow to the heart. They treat coronary artery disease by restoring blood flow and reducing symptoms.
What are the different types of cardiac stents available?
There are bare-metal stents and drug-eluting stents available. We discuss these options with patients to find the most suitable stent for their needs.
References
- Suh, J., et al. (2010). The Relationship and Threshold of Stent Length With Mortality: A Multicenter Registry Study. American Journal of Cardiology, 106(12), 1767-1773. https://www.sciencedirect.com/science/article/pii/S1936879810001408





