
When every second counts, recognizing the signs and symptoms of a heart attack can be lifesaving. At Liv Hospital, we understand the importance of prompt treatment for myocardial infarction to reduce morbidity and mortality. Our mission is to provide world-class healthcare with complete support for international patients.
Heart attack symptoms often include chest pain, shortness of breath, nausea, sweating, and radiating pain to the arms, jaw, or back. We will guide you through the 10 essential signs and symptoms, as well as modern therapy options available.
Key Takeaways
- Recognizing heart attack symptoms is crucial for timely treatment.
- Myocardial infarction is often caused by coronary artery disease.
- Prompt medical attention can significantly improve patient outcomes.
- Liv Hospital provides internationally respected care for heart attack patients.
- Understanding treatment options is vital for patients and their families.
What Is Myocardial Infarction: Definition and Pathophysiology

Understanding myocardial infarction is crucial for early diagnosis and effective treatment, as it involves the interruption of blood flow to the heart muscle, leading to damage or death of the heart tissue. Myocardial infarction, commonly referred to as a heart attack, is a serious medical emergency that requires immediate attention.
The Mechanism Behind Heart Attacks
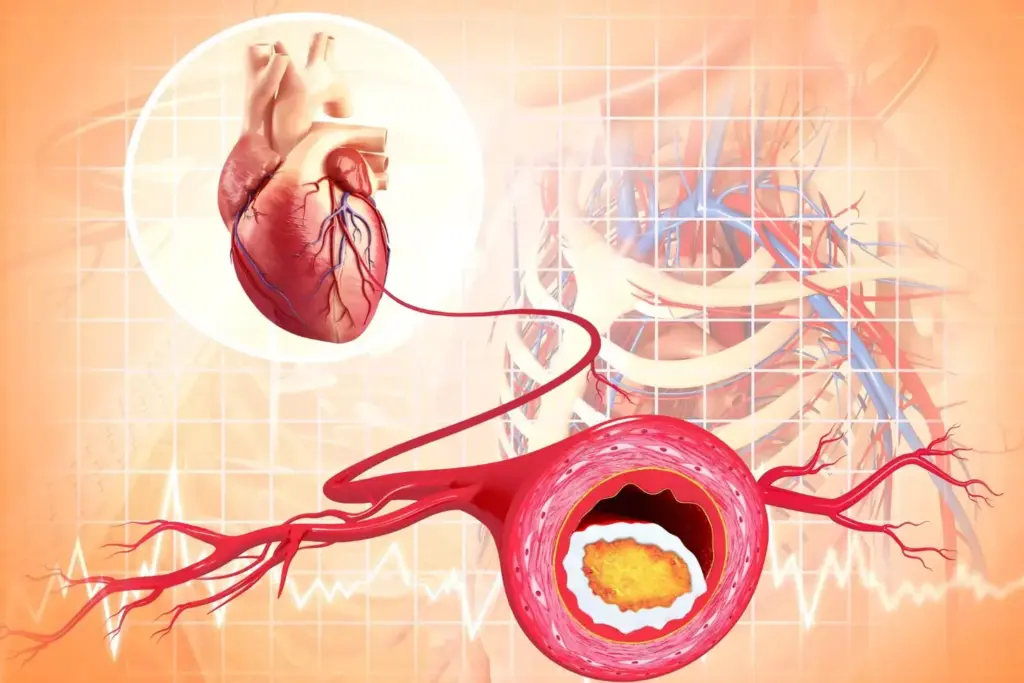
The mechanism behind heart attacks involves a complex interplay of factors that ultimately lead to the obstruction of blood flow to the heart muscle. Coronary artery disease is the primary culprit, where plaque buildup in the arteries leads to their narrowing or complete blockage.
“The most common cause of myocardial infarction is the rupture of an atherosclerotic plaque, leading to acute thrombosis and occlusion of a coronary artery,” as emphasized by cardiovascular research.
Coronary Artery Disease as the Primary Cause
Coronary artery disease (CAD) is the underlying cause of most myocardial infarctions. CAD involves the narrowing or blockage of the coronary arteries due to atherosclerosis, which is the buildup of plaque composed of fat, cholesterol, and other substances.
The progression of CAD can lead to reduced blood flow to the heart, causing angina or, if severe, a myocardial infarction. Understanding the risk factors for CAD is crucial for prevention, as it allows for early intervention and management.
Types of Myocardial Infarction
Myocardial infarctions are classified based on the electrocardiogram (ECG) findings and biomarkers. The two main types are:
- ST-Elevation Myocardial Infarction (STEMI): Characterized by a complete blockage of a coronary artery, indicated by ST elevation on an ECG.
- Non-ST Elevation Myocardial Infarction (NSTEMI): Involves a partial blockage, without ST elevation on the ECG.
Recognizing these types is essential for guiding treatment decisions and improving outcomes.
Risk Factors and Prevention of Myocardial Infarction
The occurrence of myocardial infarction is linked to several risk factors, some of which can be modified to reduce the risk of a heart attack. Understanding these factors is crucial for both individuals and healthcare professionals to develop effective prevention strategies.
Modifiable Risk Factors
Modifiable risk factors are conditions or behaviors that can be changed to reduce the risk of myocardial infarction. According to the American Heart Association, managing these factors can significantly lower the risk of heart disease. Some of the key modifiable risk factors include:
- Hypertension: High blood pressure is a major risk factor for heart disease. Managing hypertension through lifestyle changes and medication can reduce the risk of MI.
- Smoking: Smoking is a significant risk factor for cardiovascular disease. Quitting smoking can greatly reduce the risk of myocardial infarction.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque buildup in arteries, increasing the risk of MI.
- Diabetes: Diabetes mellitus is a risk factor for cardiovascular disease. Managing blood sugar levels is crucial for reducing the risk of MI.
- Obesity and Physical Inactivity: Being overweight or obese and leading a sedentary lifestyle are risk factors for heart disease. Regular physical activity and maintaining a healthy weight can reduce these risks.
“Making healthy lifestyle choices can help prevent heart disease, and in some cases, even reverse it.”
Non-modifiable Risk Factors
While some risk factors cannot be changed, understanding them can help in managing overall risk. Non-modifiable risk factors include:
- Age: The risk of myocardial infarction increases with age. Men over 45 and women over 55 are at higher risk.
- Family History: A family history of heart disease can increase an individual’s risk.
- Gender: Men are generally at higher risk of MI than women, although the risk for women increases after menopause.
Preventive Strategies
Preventing myocardial infarction involves a combination of lifestyle changes and, when necessary, medical interventions. Some effective preventive strategies include:
- Dietary Changes: Adopting a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce the risk of MI.
- Regular Exercise: Engaging in regular physical activity can help maintain a healthy weight, lower blood pressure, and improve overall cardiovascular health.
- Stress Management: Chronic stress can contribute to the risk of heart disease. Practicing stress-reducing techniques such as meditation or yoga can be beneficial.
- Medical Check-ups: Regular health check-ups can help identify risk factors early, allowing for timely interventions.
By understanding and addressing both modifiable and non-modifiable risk factors, individuals can take proactive steps to reduce their risk of myocardial infarction. Healthcare professionals can also play a crucial role in educating patients and developing personalized prevention plans.
5 Classic Signs and Symptoms of Myocardial Infarction
Understanding the typical symptoms of myocardial infarction can significantly impact patient outcomes and survival rates. Myocardial infarction, commonly known as a heart attack, occurs when the blood flow to the heart is severely blocked, causing damage to the heart muscle. Recognizing the classic signs and symptoms is essential for timely medical intervention.
Chest Pain and Discomfort
Chest pain or discomfort is one of the most common symptoms of myocardial infarction. This pain is often described as a feeling of pressure, tightness, or heaviness in the chest that may radiate to other areas. The discomfort can be persistent or may come and go.
Radiation of Pain to Arms, Jaw, and Back
The pain associated with myocardial infarction can radiate to other parts of the body, including the arms, jaw, and back. This radiation of pain occurs because the nerves that supply the heart also supply these other areas, making it feel like the pain is spreading.
Shortness of Breath
Shortness of breath, or dyspnea, is another classic symptom of myocardial infarction. This can occur even at rest and may be accompanied by fatigue or weakness. Shortness of breath is a sign that the heart is not functioning properly.
Nausea and Vomiting
Nausea and vomiting are also common symptoms of myocardial infarction, particularly in women. These symptoms can be accompanied by other signs such as dizziness or lightheadedness.
The following table summarizes the classic signs and symptoms of myocardial infarction:
| Symptom | Description |
|---|---|
| Chest Pain/Discomfort | Feeling of pressure, tightness, or heaviness in the chest |
| Radiation of Pain | Pain spreading to arms, jaw, and back |
| Shortness of Breath | Difficulty breathing, even at rest |
| Nausea and Vomiting | Feeling queasy or vomiting, particularly in women |
5 Lesser-Known Signs of MI That Shouldn’t Be Ignored
Beyond the typical chest pain, myocardial infarction can manifest through a range of lesser-known symptoms. Being aware of these signs can help prevent delayed diagnosis and treatment. Studies have identified several atypical presentations of MI that are crucial for early detection.
1. Unexplained Fatigue and Weakness
One of the lesser-known signs of MI is unexplained fatigue and weakness. This symptom can occur due to the heart’s reduced ability to pump blood effectively, leading to a decrease in physical performance. Patients often report feeling unusually tired or weak without a clear reason.
2. Dizziness and Lightheadedness
Dizziness and lightheadedness are other atypical symptoms that can indicate MI. These sensations occur when the brain does not receive enough blood flow, potentially leading to a feeling of impending fainting. It’s essential to recognize these symptoms, especially if they are accompanied by other signs.
3. Anxiety and Sense of Doom
Some individuals experiencing MI report feelings of anxiety and a sense of doom. This psychological distress can be a manifestation of the body’s response to the cardiac event. Recognizing these feelings as potential MI symptoms can be lifesaving.
4. Indigestion or Heartburn-Like Symptoms
Indigestion or heartburn-like symptoms can sometimes be mistaken for gastrointestinal issues but can also be a sign of MI. These symptoms occur due to the heart’s distress signals being misinterpreted as gastrointestinal discomfort.
| Lesser-Known Signs | Description |
|---|---|
| Unexplained Fatigue and Weakness | Feeling unusually tired or weak without a clear reason due to reduced heart function. |
| Dizziness and Lightheadedness | Sensations occurring when the brain does not receive enough blood flow, potentially leading to fainting. |
| Anxiety and Sense of Doom | Feelings of anxiety or a sense of impending doom as a response to the cardiac event. |
| Indigestion or Heartburn-Like Symptoms | Symptoms mistaken for gastrointestinal issues but can be a sign of MI due to the heart’s distress signals. |
By being aware of these lesser-known signs of MI, individuals can seek medical attention promptly, potentially improving outcomes. It’s crucial for both patients and healthcare professionals to recognize these atypical presentations to provide timely interventions.
Clinical Manifestations of Myocardial Infarction in Special Populations
Recognizing the diverse clinical manifestations of myocardial infarction (MI) in various populations is vital for healthcare providers to deliver targeted care. Certain groups, such as diabetics and older adults, may present with atypical symptoms, making diagnosis more challenging.
Silent Myocardial Infarctions
Silent myocardial infarctions, which occur without noticeable symptoms, are more common in certain populations, such as those with diabetes. Diabetes mellitus is known to affect pain perception, potentially leading to silent MIs. We must be vigilant in diagnosing MI in diabetic patients, even in the absence of typical chest pain.
Gender Differences in MI Presentation
Research has shown that there are gender differences in the presentation of myocardial infarction. Women are more likely to experience atypical symptoms such as fatigue, shortness of breath, and nausea, whereas men typically present with chest pain. Understanding these differences is crucial for timely diagnosis and treatment.
Age-Related Variations in Symptoms
Older adults often present with atypical symptoms, including confusion, dizziness, or stroke-like symptoms. Age-related variations in MI presentation can complicate diagnosis, emphasizing the need for a high index of suspicion in elderly patients.
Diabetes and Atypical Presentations
Diabetes is associated with an increased risk of atypical MI presentations. Patients with diabetes may experience symptoms such as unexplained fatigue or nausea rather than chest pain. We should be aware of these atypical presentations to provide prompt and appropriate care.
Emergency Response: Critical Actions When MI Is Suspected
Understanding the critical actions to take when myocardial infarction is suspected can save lives. When someone experiences signs of MI, prompt emergency response is crucial. We will discuss the key steps to follow, ensuring that patients receive timely medical intervention.
Recognizing the Warning Signs
The first step in responding to a myocardial infarction is recognizing its warning signs. Common signs include chest pain or discomfort, shortness of breath, nausea, and fatigue. It’s essential to be aware of these symptoms, as timely recognition can significantly impact treatment outcomes.
| Signs of MI | Description |
|---|---|
| Chest Pain | Discomfort or pain in the chest, often radiating to the arms, back, or jaw |
| Shortness of Breath | Difficulty breathing or feeling winded even at rest |
| Nausea and Vomiting | Feeling queasy or vomiting, which can be a sign of MI, especially in women |
Immediate Actions and Calling Emergency Services
Upon recognizing the signs of MI, it’s vital to call emergency services immediately. In the United States, calling 911 is the quickest way to get help. While waiting for medical personnel to arrive, it’s helpful to keep the patient calm and comfortable. If the patient is conscious, having them chew an aspirin (if not allergic) can help prevent further clotting.
The Golden Hour: Time-Sensitive Treatment Window
The golden hour refers to the first hour after the onset of MI symptoms, during which timely medical intervention can significantly improve outcomes. Studies emphasize that early treatment, particularly within this hour, can reduce mortality and improve the chances of survival. Prompt treatment for myocardial infarction during this window can make a critical difference in patient outcomes.
By understanding the importance of the golden hour and taking immediate action when signs of MI appear, we can ensure that patients receive the timely treatment for myocardial infarction they need.
Diagnosis of Myocardial Infarction: From ER to Confirmation
When a patient presents with symptoms of myocardial infarction, a swift and accurate diagnosis is crucial. We understand that the diagnostic process for myocardial infarction is multifaceted, involving both initial assessment and subsequent diagnostic tests.
Initial Assessment and History Taking
The first step in diagnosing myocardial infarction is a thorough initial assessment and history taking. Accurate diagnosis is essential for effective treatment, and this begins with evaluating the patient’s symptoms, medical history, and risk factors for coronary artery disease. We consider factors such as age, gender, and the presence of conditions like diabetes, which can affect the presentation of myocardial infarction.
During the initial assessment, healthcare providers look for classic signs and symptoms of myocardial infarction, including chest pain, shortness of breath, and nausea. However, we also recognize that some patients, particularly women and those with diabetes, may present with atypical symptoms.
Diagnostic Tests and Procedures
Following the initial assessment, a series of diagnostic tests are conducted to confirm the diagnosis of myocardial infarction. These tests include electrocardiography (ECG), blood tests for cardiac biomarkers such as troponin, and imaging studies like echocardiography or coronary angiography.
The ECG is a critical tool in the diagnosis of myocardial infarction, providing information on the electrical activity of the heart and potential areas of ischemia or infarction. Blood tests for cardiac biomarkers are also crucial, as elevated levels of troponin can indicate myocardial damage.
In some cases, additional imaging studies may be necessary to assess cardiac function and identify potential complications. We use these diagnostic tests to guide treatment decisions and ensure that patients receive appropriate care for myocardial infarction.
Myocardial Infarction Treatments: Current Approaches and Innovations
As our understanding of myocardial infarction deepens, so too does our arsenal of effective treatments, ranging from immediate pharmacological interventions to advanced surgical options. Effective treatment options for myocardial infarction are crucial for improving patient outcomes, and recent advancements have significantly enhanced our ability to manage this condition.
Immediate Pharmacological Interventions
Upon diagnosis of myocardial infarction, immediate pharmacological interventions are initiated to reduce morbidity and mortality. These interventions include:
- Aspirin therapy to prevent further clotting
- P2Y12 inhibitors (e.g., clopidogrel) to reduce platelet aggregation
- Anticoagulants (e.g., heparin) to prevent new clot formation
- Beta-blockers to reduce myocardial oxygen demand
- ACE inhibitors or ARBs to reduce blood pressure and decrease the heart’s workload
These medications are crucial in the acute management of myocardial infarction and have been shown to improve outcomes when administered promptly.
Reperfusion Strategies
Reperfusion strategies are critical in restoring blood flow to the affected myocardium. The two primary reperfusion strategies are:
- Percutaneous Coronary Intervention (PCI): A minimally invasive procedure where a catheter is used to open the occluded artery.
- Fibrinolytic Therapy: Administration of drugs that dissolve the clot causing the myocardial infarction.
Studies have shown that timely reperfusion therapy, including PCI and fibrinolytic therapy, significantly improves outcomes in patients with myocardial infarction.
Surgical Options for Severe Cases
In some cases, surgical intervention may be necessary for patients with myocardial infarction. Surgical options include:
- Coronary Artery Bypass Grafting (CABG): A procedure where a graft is used to bypass the occluded segment of the coronary artery.
- Other surgical interventions may be required to address complications such as ventricular septal defect or mitral regurgitation.
These surgical options are typically reserved for severe cases or when other treatments have failed, and are tailored to the individual patient’s needs.
Post-MI Care: Medication Regimens for MI Disease Treatment
Effective post-myocardial infarction (MI) care is crucial for improving patient outcomes and reducing morbidity. We emphasize the importance of a comprehensive treatment plan that includes medication regimens, follow-up care, and strategies for managing complications.
Essential Medications After Myocardial Infarction
After an MI, patients are typically prescribed a combination of medications to manage their condition. These may include:
- Antiplatelet agents to prevent blood clots
- Beta-blockers to reduce heart rate and blood pressure
- ACE inhibitors to lower blood pressure and reduce strain on the heart
- Statins to lower cholesterol levels
A study published in the Journal of Patient-Centered Research in Review highlights the significance of these medications in improving post-MI outcomes institutional repository.
| Medication Class | Primary Use | Examples |
|---|---|---|
| Antiplatelet agents | Prevent blood clots | Aspirin, Clopidogrel |
| Beta-blockers | Reduce heart rate and blood pressure | Metoprolol, Atenolol |
| ACE inhibitors | Lower blood pressure and reduce heart strain | Lisinopril, Enalapril |
Follow-up Care and Monitoring
Regular follow-up appointments are vital for monitoring patient progress and adjusting treatment plans as necessary. We recommend:
- Regular check-ups with a cardiologist
- Monitoring of blood pressure and cholesterol levels
- Adjustments to medication as needed
Managing Complications After MI
Despite best efforts, complications can arise after an MI. We must be prepared to manage these complications effectively, which may include:
- Heart failure
- Arrhythmias
- Further cardiovascular events
By providing comprehensive post-MI care, we can improve patient outcomes and reduce the risk of further complications. Effective management of MI disease treatment is key to enhancing the quality of life for myocardial infarction survivors.
Treatment for Myocardial Infarction: Rehabilitation and Lifestyle Modifications
Myocardial infarction treatment doesn’t end with the initial medical intervention; it continues with a robust rehabilitation and lifestyle modification program. We recognize that recovering from a heart attack involves not just healing the heart, but also adopting habits that promote long-term cardiovascular health.
Rehabilitation and lifestyle changes are vital for improving outcomes after myocardial infarction. Studies have shown that comprehensive rehabilitation programs can significantly reduce morbidity and mortality, enhancing the quality of life for survivors.
Cardiac Rehabilitation Programs
Cardiac rehabilitation is a medically supervised program designed to improve cardiovascular health in patients who have experienced heart conditions, including myocardial infarction. These programs typically include:
- Exercise Training: Supervised exercise sessions tailored to the patient’s fitness level and health status.
- Education: Information on heart-healthy living, including diet, exercise, and stress management.
- Support: Counseling and support to help patients cope with the emotional aspects of heart disease.
By participating in cardiac rehabilitation, patients can achieve significant improvements in their physical function and overall well-being.
Dietary Changes and Nutritional Support
Adopting a heart-healthy diet is crucial for myocardial infarction survivors. We recommend focusing on:
- Fruits and Vegetables: Rich in vitamins, minerals, and antioxidants.
- Whole Grains: High in fiber, helping to lower cholesterol levels.
- Lean Proteins: Sources include poultry, fish, and legumes.
- Healthy Fats: Found in nuts, seeds, avocados, and olive oil.
Nutritional counseling can help patients make informed choices about their diet, supporting their overall cardiovascular health.
Physical Activity Guidelines for MI Survivors
Regular physical activity is essential for maintaining cardiovascular health after a myocardial infarction. We advise:
- Aerobic Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week.
- Resistance Training: Incorporate muscle-strengthening activities on two or more days a week.
- Flexibility and Balance: Include exercises that improve flexibility and balance to prevent falls.
It’s essential to consult with a healthcare provider before starting any new exercise program.
Stress Management and Mental Health Support
Managing stress and maintaining mental health are critical components of the recovery process. Techniques such as meditation, yoga, and cognitive-behavioral therapy can be beneficial. We also recommend:
- Support Groups: Joining a support group to connect with others who have experienced similar challenges.
- Mental Health Professionals: Seeking help from mental health professionals if needed.
By addressing both physical and emotional health, patients can achieve a more comprehensive recovery.
Conclusion: Advances in MI Care and Future Directions
We have seen significant advancements in the treatment and management of myocardial infarction, improving patient outcomes and reducing cardiovascular risk. The introduction of oral semaglutide, a GLP-1 receptor agonist, has been a notable development, demonstrating a 14% relative risk reduction in major adverse cardiovascular events (MACE) in high-risk type 2 diabetes patients. As reported, the SOUL trial showed that nonfatal myocardial infarction was 26% less likely with semaglutide compared to placebo. For more information on this development, visit the AJMC article on the FDA’s expansion of semaglutide’s label.
As we move forward, it is essential to stay updated with the latest research and guidelines on myocardial infarction treatments, signs, and symptoms. By understanding the risk factors, recognizing the signs and symptoms of myocardial infarction, and implementing effective treatment strategies, we can provide optimal care for patients with MI. We continue to evolve our approach to MI care, incorporating new insights and innovations to improve patient outcomes.
What is myocardial infarction?
Myocardial infarction, commonly known as a heart attack, occurs when the blood flow to the heart is severely blocked, causing damage to the heart muscle due to lack of oxygen.
What are the primary causes of myocardial infarction?
The primary cause of myocardial infarction is coronary artery disease, where the coronary arteries become narrowed or blocked due to atherosclerosis, leading to reduced blood flow to the heart.
What are the classic signs and symptoms of myocardial infarction?
Classic signs and symptoms include chest pain or discomfort, pain radiating to the arms, jaw, or back, shortness of breath, nausea, and vomiting. Recognizing these symptoms is crucial for prompt medical attention.
Are there any lesser-known signs of myocardial infarction?
Yes, lesser-known signs include unexplained fatigue, dizziness, anxiety, and indigestion or heartburn-like symptoms. Being aware of these can help in early diagnosis and treatment.
How does myocardial infarction present in special populations?
In special populations, such as diabetic patients or the elderly, myocardial infarction can present atypically, sometimes without chest pain, making diagnosis more challenging.
What are the critical actions to take when myocardial infarction is suspected?
Critical actions include recognizing warning signs, calling emergency services immediately, and understanding the importance of timely treatment within the golden hour.
How is myocardial infarction diagnosed?
Diagnosis involves initial assessment, history taking, electrocardiogram (ECG), blood tests to check for cardiac biomarkers, and imaging tests such as echocardiography or coronary angiography.
What are the current treatment approaches for myocardial infarction?
Treatments include immediate pharmacological interventions like antiplatelet therapy and anticoagulation, reperfusion strategies such as thrombolysis or percutaneous coronary intervention (PCI), and surgical options for severe cases.
What is the role of rehabilitation after myocardial infarction?
Cardiac rehabilitation programs play a crucial role in helping patients recover, including supervised exercise, education on heart-healthy living, and stress management.
What lifestyle modifications are recommended after myocardial infarction?
Recommended modifications include dietary changes, regular physical activity tailored to the individual’s condition, stress management, and smoking cessation to improve long-term health and reduce the risk of further cardiac events.
How can the risk of myocardial infarction be reduced?
Risk can be reduced by managing modifiable risk factors such as hypertension, high cholesterol, diabetes, and smoking, through lifestyle changes and, when necessary, medication.
What is the importance of the golden hour in treating myocardial infarction?
The golden hour refers to the critical first hour after the onset of myocardial infarction symptoms, during which timely medical intervention can significantly improve outcomes by restoring blood flow to the heart.























