Last Updated on November 27, 2025 by Bilal Hasdemir

At Liv Hospital, we prioritize the latest academic protocols and international standards in cardiovascular care. The 4th Universal Definition of Myocardial Infarction (MI) provides a clear and updated classification system for myocardial infarction, which is crucial for diagnosis and management. Understanding the different types of MI is essential for providing optimal patient care and outcomes.
According to the 4th Universal Definition, there are five main types of myocardial infarction. By understanding these definitions, healthcare providers can offer more precise and targeted care to patients. We follow the latest guidelines to ensure that our patients receive the best possible treatment.
Key Takeaways
- Understanding the 5 types of myocardial infarction is crucial for optimal patient care.
- The 4th Universal Definition provides a clear classification system for MI.
- Liv Hospital follows the latest academic protocols and international standards.
- Accurate diagnosis and management of MI are critical for patient outcomes.
- The 4th Universal Definition enables healthcare providers to offer targeted care.
Understanding What is Medical Term MI
Understanding the medical term MI is crucial for patients and healthcare providers alike, as it signifies a heart attack that can have severe consequences if not treated promptly. Myocardial infarction (MI) is a serious medical condition characterized by the death of heart muscle cells due to inadequate blood supply.
Definition and Pathophysiology of Myocardial Infarction
Myocardial infarction, commonly referred to as a heart attack, occurs when the blood flow to a part of the heart is blocked for a long enough time that part of the heart muscle is damaged or dies. This blockage is typically caused by a blood clot that forms on a patch of atherosclerosis (plaque) inside a coronary artery. The pathophysiology of myocardial infarction involves a complex interplay between the coronary arteries, the heart muscle, and the blood’s clotting mechanisms.
We will delve into the definition of myocardial infarction and its pathophysiology, explaining how it leads to significant morbidity and mortality globally. The medical term MI refers to myocardial infarction, defined as acute myocardial injury with evidence of myocardial ischemia.
Clinical Significance and Global Burden
Myocardial infarction is a major cause of morbidity and mortality worldwide. According to global health statistics, MI is one of the leading causes of death and disability. The clinical significance of understanding MI lies in its impact on patient outcomes and the healthcare system as a whole.
We recognize the importance of timely diagnosis and treatment of MI to improve patient outcomes. The global burden of MI underscores the need for continued research, prevention strategies, and effective management protocols. By understanding the clinical significance and global burden of MI, we can better address the challenges it poses to healthcare systems worldwide.
Evolution of Myocardial Infarction Definitions
The definition and classification of myocardial infarction have evolved substantially, driven by new evidence and clinical practices. This evolution reflects our growing understanding of the pathophysiology of MI and the development of more sophisticated diagnostic tools.
Historical Perspective on MI Classification
Historically, the classification of myocardial infarction was based on clinical presentation and electrocardiographic changes. Over time, the introduction of cardiac biomarkers, such as troponin, has significantly improved the diagnosis of MI. The incorporation of these biomarkers into the definition has allowed for earlier and more accurate detection of myocardial infarction.
The earlier definitions of MI were often based on a combination of clinical symptoms, ECG changes, and enzyme levels. However, as our understanding of the molecular mechanisms underlying MI has grown, so too has the complexity of its definition.
Development of the Universal Definition System
The Universal Definition System was introduced to standardize the diagnosis and classification of myocardial infarction globally. This system has undergone several revisions to incorporate new evidence and improve clinical practice. The fourth universal definition represents the latest consensus, providing a clear distinction between myocardial infarction and myocardial injury.
The development of the Universal Definition System has been crucial in improving the diagnosis and management of MI. By standardizing the criteria for MI, it has facilitated more accurate clinical research and enhanced patient care.
The table below summarizes the key developments in the evolution of MI definitions:
| Year | Definition/Classification System | Key Features |
|---|---|---|
| 2000 | Initial Universal Definition | Introduced standardized criteria for MI diagnosis |
| 2007 | Second Universal Definition | Incorporated cardiac biomarkers, clarified MI types |
| 2012 | Third Universal Definition | Further refined MI classification, emphasized troponin |
| 2018 | Fourth Universal Definition | Distinguished between MI and myocardial injury, updated criteria |
The evolution of myocardial infarction definitions reflects our ongoing commitment to improving patient outcomes through more accurate diagnosis and management. As we continue to advance our understanding of MI, the Universal Definition System will remain a critical tool in clinical practice and research.
The 4th Universal Definition of Myocardial Infarction
The 4th Universal Definition provides a refined understanding of myocardial infarction, incorporating the latest medical advancements. This definition is crucial for clinicians and researchers alike, as it standardizes the diagnosis and classification of myocardial infarction (MI).
One of the significant advancements in the 4th Universal Definition is the incorporation of high-sensitivity cardiac troponin assays. These assays have improved the detection of myocardial injury and infarction, allowing for more precise diagnosis and treatment.
Key Updates from Previous Definitions
The 4th Universal Definition has introduced several key updates from previous definitions. One of the most notable changes is the emphasis on the role of cardiac troponin in diagnosing MI. The new definition highlights the importance of using high-sensitivity cardiac troponin assays to detect myocardial injury and infarction.
Another significant update is the clarification of the criteria for diagnosing different types of MI. The 4th Universal Definition provides clear guidelines for distinguishing between Type 1, Type 2, and other forms of MI, which is essential for appropriate management and treatment.
| Update | Description |
|---|---|
| High-Sensitivity Cardiac Troponin Assays | Improved detection of myocardial injury and infarction |
| Clarification of MI Types | Clear guidelines for diagnosing different types of MI |
| Emphasis on Cardiac Troponin | Importance of cardiac troponin in diagnosing MI |
Distinguishing Myocardial Injury from Infarction
Distinguishing between myocardial injury and infarction is critical for appropriate patient management. The 4th Universal Definition provides clear criteria for making this distinction. According to the definition, myocardial infarction is characterized by the presence of myocardial injury with evidence of acute myocardial ischemia.
“Myocardial infarction is a clinical event that is distinct from myocardial injury, and the distinction is critical for appropriate patient management.” –
The use of high-sensitivity cardiac troponin assays has been instrumental in this distinction. These assays allow clinicians to detect even minor elevations in troponin levels, which can indicate myocardial injury or infarction.
In conclusion, the 4th Universal Definition of Myocardial Infarction has refined the diagnosis and classification of MI, incorporating the latest advancements in medical technology. By understanding the key updates and the distinction between myocardial injury and infarction, clinicians can provide more accurate and effective care for patients.
Diagnostic Criteria for Myocardial Infarction
The diagnostic process for myocardial infarction has evolved significantly with advancements in cardiac biomarkers and imaging modalities. Accurate diagnosis is crucial for timely and effective treatment, which can significantly improve patient outcomes.
Role of High-Sensitivity Cardiac Troponin Assays
High-sensitivity cardiac troponin assays have revolutionized the diagnosis of myocardial infarction. These assays can detect very low levels of troponin, enabling early diagnosis and intervention. The use of high-sensitivity troponin assays has been shown to improve diagnostic accuracy and reduce the time to diagnosis.
Key benefits of high-sensitivity cardiac troponin assays include:
- Early detection of myocardial infarction
- Improved diagnostic accuracy
- Reduced time to diagnosis and treatment
Electrocardiographic Changes in MI
Electrocardiography (ECG) remains a cornerstone in the diagnosis of myocardial infarction. ECG changes can indicate the presence and location of MI. Common ECG changes include ST-segment elevation, ST-segment depression, and Q-wave formation.
ECG interpretation requires careful analysis to identify subtle changes that may indicate MI.
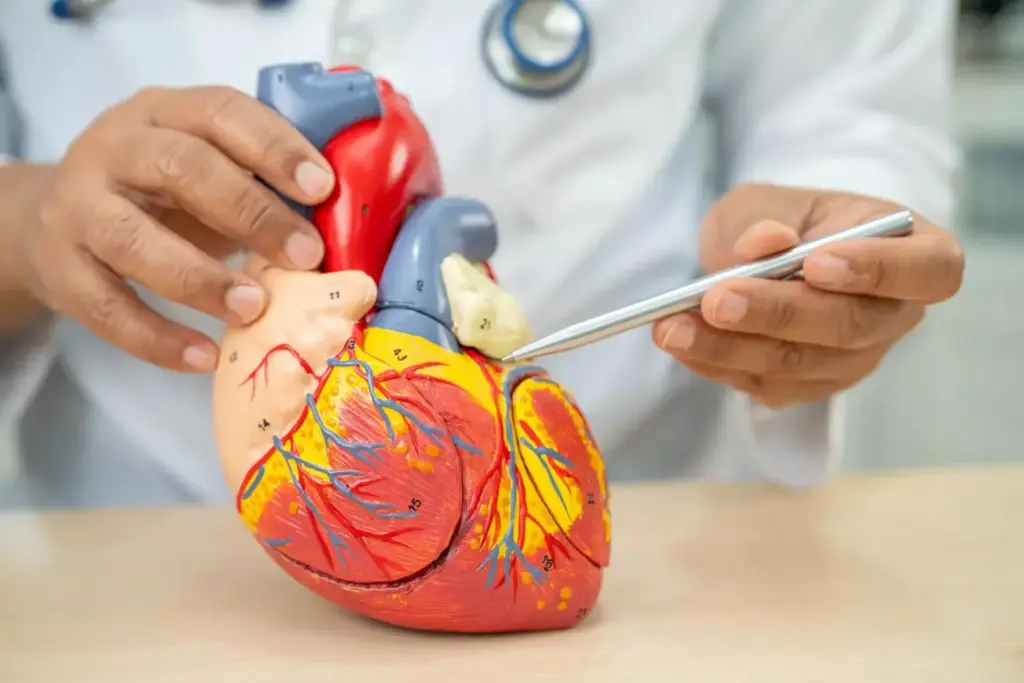
Imaging Techniques for MI Diagnosis
Imaging techniques play a vital role in the diagnosis and management of myocardial infarction. Modalities such as echocardiography, cardiac magnetic resonance imaging (MRI), and coronary angiography provide valuable information on cardiac structure and function.
Imaging techniques can help:
- Assess cardiac function and structure
- Identify areas of ischemia or infarction
- Guide treatment decisions
By combining high-sensitivity cardiac troponin assays, electrocardiographic changes, and imaging techniques, healthcare professionals can make accurate diagnoses and develop effective treatment plans for patients with myocardial infarction.
Type 1 Myocardial Infarction: Spontaneous Coronary Event
A spontaneous coronary event leading to thrombosis is the defining feature of Type 1 myocardial infarction. This condition is characterized by the rupture of an atherosclerotic plaque, leading to acute thrombosis and subsequent occlusion of a coronary artery.
Pathophysiology and Atherothrombosis
Type 1 MI is primarily caused by atherothrombosis, which occurs when an atherosclerotic plaque ruptures, exposing highly thrombogenic lipid-rich material to the bloodstream. This triggers the formation of a thrombus, which can occlude the coronary artery, leading to myocardial infarction.
“The rupture of an atherosclerotic plaque is a critical event in the pathophysiology of Type 1 MI,” as noted by experts in the field. Atherothrombosis is a complex process involving inflammation, endothelial dysfunction, and platelet activation.
Clinical Presentation and Symptoms
The clinical presentation of Type 1 MI typically includes chest pain or discomfort, often described as a squeezing or pressure sensation. Other symptoms may include shortness of breath, nausea, and fatigue.
Patients with Type 1 MI often present with symptoms that are similar to those of other acute coronary syndromes. Prompt recognition and diagnosis are crucial for effective management.
Management Strategies and Outcomes
The management of Type 1 MI involves immediate medical therapy, including antiplatelet agents, anticoagulants, and coronary revascularization. The goal is to restore blood flow to the affected myocardium and prevent further damage.
“Early revascularization, either through percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), is critical for improving outcomes in patients with Type 1 MI.”
Effective management strategies can significantly improve outcomes for patients with Type 1 MI. Timely intervention is key to reducing morbidity and mortality.
Type 2 Myocardial Infarction: Oxygen Supply-Demand Imbalance
Type 2 myocardial infarction (MI) is a condition characterized by an imbalance between myocardial oxygen supply and demand. This type of MI is secondary to an imbalance in oxygen supply and demand, rather than a sudden blockage of a coronary artery.
Underlying Mechanisms and Common Causes
Type 2 MI often occurs in patients with underlying conditions such as anemia, tachycardia, or hypertension. These conditions can lead to an increase in myocardial oxygen demand or a decrease in oxygen supply, resulting in myocardial injury.
As stated by experts, “The diagnosis of Type 2 MI requires a careful assessment of the clinical context, including the presence of conditions that may lead to an imbalance in oxygen supply and demand.”
“The presence of underlying conditions such as anemia or tachycardia can significantly increase the risk of Type 2 MI.”
Distinguishing Type 2 from Type 1 MI
Distinguishing Type 2 MI from Type 1 MI is crucial for appropriate management. Type 1 MI is caused by a spontaneous coronary event such as plaque rupture or erosion, leading to thrombus formation and occlusion of a coronary artery. In contrast, Type 2 MI is not directly caused by a coronary thrombus but rather by an imbalance in oxygen supply and demand.
- Type 1 MI: Caused by a spontaneous coronary event.
- Type 2 MI: Caused by an imbalance in oxygen supply and demand.
Treatment Approaches and Challenges
The treatment of Type 2 MI focuses on addressing the underlying cause of the imbalance. This may involve correcting anemia, controlling hypertension, or managing tachycardia. The management strategy for Type 2 MI differs from that of Type 1 MI, where the focus is on restoring coronary blood flow.
As we manage patients with Type 2 MI, it’s essential to recognize that the treatment approach must be tailored to the individual patient’s condition. “A personalized treatment plan can significantly improve outcomes in patients with Type 2 MI.”
Type 3 Myocardial Infarction: Cardiac Death with Biomarker Evidence
The diagnosis of Type 3 myocardial infarction is reserved for cases of sudden cardiac death where myocardial infarction is suspected or confirmed. This type of myocardial infarction is particularly challenging to diagnose because it involves cases where patients die suddenly before biomarkers or other diagnostic criteria can be fully assessed.
Criteria for Diagnosis in Sudden Cardiac Death
Diagnosing Type 3 myocardial infarction requires a combination of clinical history, symptoms prior to death, and post-mortem findings. Key diagnostic criteria include evidence of fresh thrombus in a coronary artery or signs of recent myocardial infarction at autopsy. In some cases, electrocardiographic changes or elevated biomarkers in the hours preceding death can support the diagnosis.
It’s crucial to differentiate between sudden cardiac death due to myocardial infarction and other causes. A thorough investigation is necessary to rule out other potential causes of death.
Post-Mortem Evaluation and Classification Challenges
Post-mortem evaluation plays a critical role in diagnosing Type 3 myocardial infarction. Pathologists must carefully examine the heart for signs of acute myocardial infarction, such as necrosis or fresh thrombi in the coronary arteries. However, this process can be challenging due to the potential for limited or absent antemortem diagnostic data.
Classification challenges arise when trying to distinguish between Type 3 myocardial infarction and other causes of sudden cardiac death. Accurate classification is essential for both clinical and epidemiological purposes. It requires a comprehensive review of all available clinical and pathological information.
Type 4 Myocardial Infarction: PCI-Related Subtypes
Type 4 myocardial infarction encompasses several subtypes related to percutaneous coronary intervention (PCI), including procedure-related MI, stent thrombosis, and restenosis. We will explore these subtypes in detail, understanding their diagnosis and management strategies.
Procedure-Related MI (Type 4a)
Type 4a myocardial infarction refers to MI directly related to the PCI procedure. Procedure-related MI is diagnosed when there is evidence of myocardial necrosis in the context of PCI. This can be due to various factors such as side branch occlusion, coronary dissection, or embolism during the procedure.
The diagnosis of Type 4a MI involves assessing cardiac biomarkers, particularly troponin levels, which should be elevated above the 99th percentile upper reference limit. Clinical symptoms and ECG changes also play a crucial role in diagnosing procedure-related MI.
Stent Thrombosis (Type 4b)
Stent thrombosis, or Type 4b MI, is a serious complication that can occur after stent placement during PCI. It is characterized by the formation of a blood clot within the stent, which can lead to acute coronary occlusion.
The diagnosis of stent thrombosis is often made in the context of acute coronary syndrome, with symptoms such as chest pain and ECG changes indicative of ischemia. Timely intervention is critical to manage stent thrombosis effectively.
Restenosis (Type 4c)
Type 4c myocardial infarction refers to MI associated with restenosis after PCI. Restenosis is the re-narrowing of the coronary artery after angioplasty or stenting.
The diagnosis of restenosis-related MI involves assessing symptoms, angiographic evidence, and cardiac biomarkers. Managing restenosis involves considering repeat revascularization or other therapeutic strategies.
Type 5 Myocardial Infarction: CABG-Associated
Coronary artery bypass grafting (CABG) is associated with a specific type of myocardial infarction known as Type 5 MI. This condition is a significant concern for patients undergoing CABG surgery, as it can impact outcomes and prognosis.
Mechanisms of Perioperative Myocardial Injury
Perioperative myocardial injury in the context of CABG can occur due to various mechanisms. These include direct trauma to the heart, ischemia-reperfusion injury, and distal embolization during the surgical procedure. Understanding these mechanisms is crucial for developing effective prevention strategies.
The surgical process itself can lead to myocardial stress, partly due to cardiopulmonary bypass and the manipulation of the heart. Careful surgical techniques and optimized cardioprotective strategies are essential in minimizing this risk.
Prevention and Management Strategies
Preventing Type 5 MI involves a multifaceted approach, including preoperative risk assessment, optimized surgical techniques, and postoperative care. Identifying patients at high risk and implementing tailored strategies can help reduce the incidence of perioperative myocardial injury.
- Preoperative optimization of cardiac function
- Use of cardioprotective agents during surgery
- Minimizing cross-clamp time and optimizing myocardial protection
Management of Type 5 MI, when it occurs, involves prompt recognition and appropriate intervention. This may include intensive monitoring, supportive care, and targeted therapies to address the underlying cause of the myocardial injury.
Differential Diagnosis and Clinical Decision-Making
Accurate diagnosis of myocardial infarction (MI) is crucial for effective treatment, and understanding the different types of MI is essential for clinical decision-making. The complexity of MI diagnosis lies in distinguishing between various types, each with distinct implications for patient management and prognosis.
Distinguishing Between MI Types in Clinical Practice
In clinical practice, distinguishing between different MI types requires a comprehensive approach that incorporates clinical presentation, electrocardiographic (ECG) changes, and biomarker levels. Type 1 MI is characterized by spontaneous coronary artery thrombosis, whereas Type 2 MI is caused by an imbalance between oxygen supply and demand. Understanding these differences is vital for tailoring treatment strategies.
- Clinical assessment and history taking are crucial in identifying the underlying cause of MI.
- ECG changes and biomarker levels provide critical information for diagnosing and classifying MI.
- Imaging techniques, such as echocardiography, may be used to assess cardiac function and identify potential complications.
As -Dr. one of the authors of the Universal Definition of Myocardial Infarction, notes, “The diagnosis of MI requires a combination of clinical, ECG, and biochemical criteria.”
“The diagnosis of myocardial infarction is based on the detection of a rise and/or fall of cardiac troponin values with at least one value above the 99th percentile upper reference limit, together with evidence of myocardial ischemia.”
Impact on Treatment Decisions and Prognosis
The accurate diagnosis of MI type has a significant impact on treatment decisions and patient prognosis. For instance, Type 1 MI often requires immediate coronary angiography and revascularization, whereas Type 2 MI management focuses on addressing the underlying cause of the oxygen supply-demand imbalance.
Treatment decisions are also influenced by the presence of comorbidities and the patient’s overall clinical condition. A comprehensive treatment plan may include:
- Pharmacological interventions, such as antiplatelet therapy and anticoagulation.
- Lifestyle modifications, including dietary changes and smoking cessation.
- Revascularization procedures, such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
In conclusion, differential diagnosis and clinical decision-making are critical components of effective MI management. By accurately distinguishing between MI types and understanding their implications for treatment and prognosis, healthcare providers can deliver high-quality, patient-centered care.
Conclusion
Understanding the different types of myocardial infarction is crucial for providing effective care to patients. The 4th Universal Definition of Myocardial Infarction has clarified the classification of MI into distinct types, enabling healthcare providers to diagnose and manage patients more accurately.
At Liv Hospital, we prioritize the latest academic protocols and international standards, ensuring that our patients receive world-class healthcare. By adhering to the 4th Universal Definition, we can better distinguish between various MI types, such as Type 1 and Type 2 myocardial infarction, and develop targeted treatment strategies.
The precise definition of myocardial infarction is essential for clinicians to make informed decisions and provide optimal care. We are committed to staying up-to-date with the latest guidelines, ensuring that our patients benefit from the most advanced medical knowledge and treatments.
By understanding the nuances of myocardial infarction types and adhering to the 4th Universal Definition, we can improve patient outcomes and deliver high-quality care that meets the needs of our international patients.
FAQ
What is myocardial infarction (MI), and how is it defined according to the 4th Universal Definition?
Myocardial infarction (MI) is a condition characterized by acute myocardial injury with evidence of myocardial ischemia. The 4th Universal Definition provides a clear and updated classification system for MI, distinguishing it from other forms of myocardial injury.
What are the different types of myocardial infarction according to the 4th Universal Definition?
The 4th Universal Definition categorizes myocardial infarction into five types: Type 1 (spontaneous coronary event), Type 2 (oxygen supply-demand imbalance), Type 3 (cardiac death with biomarker evidence), Type 4 (PCI-related subtypes), and Type 5 (CABG-associated).
How is Type 1 MI different from Type 2 MI?
Type 1 MI is characterized by a spontaneous coronary event, often associated with atherothrombosis, whereas Type 2 MI is caused by an imbalance between oxygen supply and demand, often due to conditions such as severe hypertension or tachycardia.
What is the role of high-sensitivity cardiac troponin assays in diagnosing MI?
High-sensitivity cardiac troponin assays play a crucial role in diagnosing MI by detecting even minor elevations in cardiac troponin levels, allowing for earlier and more accurate diagnosis.
How does the 4th Universal Definition improve the diagnosis and management of MI?
The 4th Universal Definition provides a refined classification system, enabling healthcare providers to distinguish between different types of MI and offer more precise and targeted care to patients, ultimately improving outcomes.
What are the challenges in diagnosing Type 3 MI?
Diagnosing Type 3 MI is challenging due to the requirement for biomarker evidence in the context of sudden cardiac death, and the need for careful consideration of clinical and pathological evidence.
How is Type 4 MI related to PCI, and what are its subtypes?
Type 4 MI is related to percutaneous coronary intervention (PCI) and is further categorized into subtypes: Type 4a (procedure-related MI), Type 4b (stent thrombosis), and Type 4c (restenosis).
What is the significance of distinguishing between different types of MI in clinical practice?
Distinguishing between different types of MI is crucial for guiding treatment decisions and predicting prognosis, as each type has distinct underlying mechanisms and management strategies.
How does Liv Hospital approach the diagnosis and management of MI?
Liv Hospital follows the latest guidelines, including the 4th Universal Definition, to provide accurate diagnosis and effective management of MI, ensuring patients receive the best possible care.