Last Updated on November 27, 2025 by Bilal Hasdemir
Acute myocardial infarction, commonly known as a heart attack, is a critical condition where blood flow to the heart muscle is suddenly blocked, causing tissue damage.
At Liv Hospital, we emphasize the importance of prompt AMI diagnosis and treatment to improve patient outcomes. Recent guidelines highlight the need for timely intervention to minimize damage and enhance survival rates.
Our approach involves using the latest academic protocols and a multidisciplinary team to deliver world-class care. Effective myocardial infarction treatment requires a comprehensive strategy, and we are committed to providing the best possible care for our international patients.
Key Takeaways
- Prompt diagnosis is crucial for effective AMI treatment.
- Advanced care protocols improve patient outcomes.
- A multidisciplinary team is essential for comprehensive care.
- Timely intervention minimizes heart damage.
- Liv Hospital is committed to delivering world-class care.
AMI in Medical Terms: Definition and Overview
AMI represents a significant global health burden, necessitating comprehensive understanding and management. As a leading cause of morbidity and mortality worldwide, AMI has substantial economic and healthcare implications.
Definition and Clinical Significance
Acute myocardial infarction (AMI), commonly referred to as a heart attack, occurs when the blood flow to the heart is abruptly blocked, causing damage to the heart muscle. This condition is a medical emergency requiring immediate attention. The clinical significance of AMI lies in its potential to cause significant morbidity, mortality, and healthcare expenditure.
The definition of AMI encompasses various clinical presentations, including ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI). Understanding these distinctions is vital for guiding treatment decisions.
Epidemiology and Global Impact
Studies have shown that AMI is a leading cause of morbidity and mortality worldwide, with significant economic and healthcare burdens (Hall et al., 2024). The global impact of AMI is substantial, affecting millions of people annually. Factors such as aging populations, lifestyle changes, and increasing prevalence of risk factors contribute to the growing burden of AMI.
Epidemiological data highlight the need for effective preventive strategies and timely management of AMI to reduce its global impact.
Classification of Myocardial Infarction Types
Myocardial infarction can be classified into several types based on the underlying pathophysiology and clinical presentation. The main types include:
- Type 1: Spontaneous MI related to ischemia due to a primary coronary event
- Type 2: MI secondary to ischemia due to either increased oxygen demand or decreased supply
- Type 3: Sudden unexpected cardiac death, including cardiac arrest
- Type 4: MI associated with percutaneous coronary intervention (PCI)
- Type 5: MI associated with coronary artery bypass grafting (CABG)
Understanding these classifications is essential for tailoring management strategies to individual patient needs.
The Pathophysiology of Acute Myocardial Infarction

Understanding the pathophysiology of AMI is crucial for developing effective treatment strategies. The process involves a complex interplay of various factors leading to coronary artery occlusion and subsequent myocardial tissue damage.
Coronary Artery Occlusion Process
The coronary artery occlusion process is a critical event in the pathophysiology of AMI. It typically occurs due to the rupture of an atherosclerotic plaque, leading to the formation of a thrombus that occludes the coronary artery. This occlusion results in a sudden reduction or complete cessation of blood flow to the myocardium, causing ischemia and eventually necrosis of the cardiac tissue.
Thrombus formation is a key factor in this process, and it is influenced by various factors including platelet activation, coagulation cascade, and local hemodynamic factors. Research has shown that the composition of the atherosclerotic plaque, including its lipid content and inflammatory status, plays a significant role in determining its vulnerability to rupture as highlighted in recent studies.
Myocardial Tissue Damage Progression
The progression of myocardial tissue damage following coronary artery occlusion is a dynamic process. Initially, the lack of blood flow leads to ischemia, which can be reversible if blood flow is restored promptly. However, prolonged ischemia results in irreversible damage or infarction of the myocardial tissue.
The extent and severity of the damage depend on several factors, including the duration of occlusion, the presence of collateral circulation, and the metabolic demand of the myocardium. Understanding these factors is crucial for timely intervention to minimize damage.
Reperfusion Injury Mechanisms
While reperfusion is essential to salvage ischemic myocardium, it can also lead to additional damage, known as reperfusion injury. This injury is caused by the sudden restoration of blood flow, which can lead to oxidative stress, inflammation, and disruption of cellular function.
Reperfusion injury mechanisms involve complex cellular and molecular pathways, including the generation of reactive oxygen species, calcium overload, and mitochondrial dysfunction. Understanding these mechanisms is vital for developing strategies to mitigate reperfusion injury and improve outcomes in AMI patients.
Recognizing Key Symptoms of AMI
The ability to recognize AMI symptoms promptly is essential for effective treatment and patient outcomes. Acute Myocardial Infarction (AMI), commonly known as a heart attack, occurs when blood flow to the heart is severely blocked, causing damage to the heart muscle. Recognizing the symptoms of AMI is crucial for timely medical intervention.
Classic and Atypical Presentation Patterns
AMI symptoms can vary significantly among patients. Classic symptoms include chest pain or discomfort, often described as a pressure or tightness in the chest that may radiate to the arm, neck, or jaw. However, not all patients present with these typical symptoms. Atypical presentations can include symptoms such as shortness of breath, nausea, or fatigue, which can be misleading and delay diagnosis.
Studies have shown that a significant proportion of patients, especially women and older adults, may experience atypical symptoms. For instance, women are more likely to report shortness of breath and fatigue as primary symptoms, whereas men often present with chest pain. Understanding these differences is vital for healthcare providers to make accurate and timely diagnoses.
Gender and Age Differences in Symptom Presentation
Research has highlighted that AMI symptoms can differ significantly across various demographic groups. For example, older adults and patients with diabetes may have a higher incidence of atypical presentations. Recognizing these differences is crucial for providing appropriate care. We must be aware of these variations to ensure that all patients receive timely and effective treatment.
- Women are more likely to experience atypical symptoms such as back or jaw pain.
- Older adults may present with confusion or altered mental status.
- Patients with diabetes may have reduced pain perception, making diagnosis more challenging.
Red Flags Requiring Immediate Medical Attention
Certain symptoms and signs should prompt immediate medical evaluation. These red flags include severe chest pain, difficulty breathing, or loss of consciousness. Patients experiencing these symptoms should be taken to the emergency department without delay. We emphasize the importance of acting quickly in the face of these symptoms to prevent serious outcomes.
In conclusion, recognizing the key symptoms of AMI and understanding the variations in presentation among different patient groups are critical for timely diagnosis and effective treatment. By being aware of the classic and atypical symptoms, as well as the red flags that require immediate attention, we can improve patient outcomes and save lives.
Vital Signs and Physical Examination in AMI Patients
Assessing vital signs and performing a physical examination are crucial steps in evaluating patients with Acute Myocardial Infarction (AMI). These assessments provide critical information about the patient’s hemodynamic stability and guide immediate care and management decisions.
Characteristic Vital Sign Changes
In AMI patients, vital signs can exhibit characteristic changes that indicate the severity of the condition. Heart rate and blood pressure are particularly important, as tachycardia or bradycardia can occur, and hypertension or hypotension may be present. We must carefully monitor these changes to assess the patient’s hemodynamic status.
For instance, hypotension can be a sign of cardiogenic shock, a serious complication of AMI that requires immediate attention. Conversely, hypertension may indicate increased stress on the heart, necessitating appropriate management.
Physical Examination Findings
A thorough physical examination can reveal valuable information about AMI patients. We look for signs such as jugular venous distension, which can indicate right ventricular failure, and pulmonary edema, which suggests left ventricular failure.
Other important findings include cardiac murmurs, which may indicate valvular dysfunction, and pericardial rub, suggesting pericarditis. These physical examination findings help us understand the extent of cardiac involvement and guide further diagnostic and therapeutic strategies.
Hemodynamic Instability Assessment
Assessing hemodynamic instability is critical in AMI patients, as it directly impacts management decisions. We evaluate parameters such as cardiac output and systemic vascular resistance to determine the patient’s hemodynamic status.
Hemodynamic instability can manifest as hypotension, oliguria, or cool extremities, among other signs. Recognizing these signs early allows us to intervene promptly and effectively manage the patient’s condition.
Risk Factors Contributing to MI Development
Understanding the risk factors that contribute to the development of Acute Myocardial Infarction (AMI) is crucial for effective prevention and management. We recognize that AMI risk factors can be broadly categorized into modifiable and non-modifiable factors, each playing a significant role in disease development.
Modifiable Risk Factors
Modifiable risk factors are those that can be changed or controlled through lifestyle modifications or medical interventions. Key modifiable risk factors for AMI include:
- Hypertension
- Diabetes mellitus
- Smoking
- Hyperlipidemia
- Obesity
- Physical inactivity
These factors are significant because they can be targeted through preventive measures, thereby reducing the risk of developing AMI. For instance, managing hypertension through medication and lifestyle changes can substantially reduce cardiovascular risk.
Non-modifiable Risk Factors
Non-modifiable risk factors are those that cannot be changed by the individual. These include:
- Age
- Family history of coronary artery disease
- Gender
- Genetic predispositions
Understanding these non-modifiable risk factors is essential for identifying individuals at higher risk and implementing early preventive strategies.
Risk Stratification Approaches
Risk stratification involves assessing the likelihood of an individual developing AMI based on their risk factor profile. This approach enables healthcare providers to tailor preventive measures and monitor high-risk patients more closely.
| Risk Factor Category | Examples | Intervention Strategies |
|---|---|---|
| Modifiable | Hypertension, Diabetes, Smoking | Lifestyle modifications, Medications |
| Non-modifiable | Age, Family History, Gender | Close monitoring, Early preventive measures |
By understanding and addressing both modifiable and non-modifiable risk factors, we can develop effective strategies for preventing and managing AMI, ultimately improving patient outcomes.
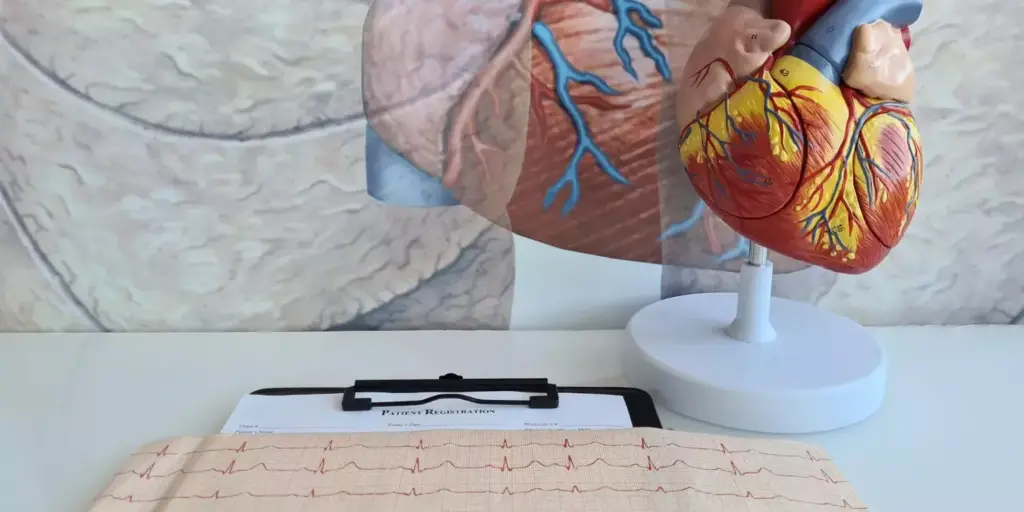
Diagnostic Approach to Suspected AMI
A timely diagnosis of AMI is critical for effective management and patient outcomes. We outline a structured diagnostic approach that begins with an initial clinical assessment, followed by considerations for differential diagnosis, and concludes with the implementation of diagnostic algorithms.
Initial Clinical Assessment
The initial clinical assessment is pivotal in identifying patients with suspected AMI. It involves a thorough medical history, physical examination, and electrocardiogram (ECG) to quickly identify potential acute coronary syndrome (ACS).
- Assessing symptoms and medical history
- Performing a focused physical examination
- Conducting an electrocardiogram (ECG)
Differential Diagnosis Considerations
Differential diagnosis for AMI includes conditions that may mimic its symptoms, such as myocarditis, pulmonary embolism, and acute aortic dissection. Accurate differentiation is crucial for appropriate management.
- Myocarditis and pericarditis
- Pulmonary embolism
- Acute aortic dissection
Diagnostic Algorithm Implementation
Guidelines recommend using a diagnostic algorithm that incorporates clinical assessment, ECG findings, and cardiac biomarkers to diagnose AMI.
The algorithm facilitates a rapid and accurate diagnosis, enabling timely intervention. Key components include:
- Risk stratification tools
- Serial biomarker measurements
- Imaging studies when necessary
By following this structured diagnostic approach, healthcare providers can effectively identify and manage AMI, improving patient outcomes.
Laboratory Tests for AMI Diagnosis
Accurate diagnosis of AMI is significantly facilitated by laboratory tests, especially the analysis of cardiac biomarkers. These tests are crucial for confirming the diagnosis and guiding treatment decisions.
Cardiac Biomarkers: Troponin and Beyond
Cardiac biomarkers, such as troponin, are proteins released into the bloodstream when the heart muscle is damaged. Troponin is highly specific and sensitive for myocardial infarction, making it a cornerstone in AMI diagnosis. Other biomarkers like creatine kinase (CK-MB) and myoglobin are also used, although they are less specific than troponin.
The use of cardiac biomarkers has revolutionized the diagnosis of AMI, enabling healthcare providers to quickly and accurately identify patients who require immediate intervention.
Interpretation of Serial Biomarker Results
Serial measurements of cardiac biomarkers are essential for diagnosing AMI and assessing the extent of cardiac damage. The pattern of biomarker release can provide valuable information about the timing and severity of the infarct.
| Biomarker | Peak Elevation | Normalization Time |
|---|---|---|
| Troponin | 12-24 hours | 7-14 days |
| CK-MB | 12-24 hours | 2-3 days |
| Myoglobin | 1-3 hours | 12-24 hours |
Novel Biomarkers in AMI Diagnosis
Research is ongoing to identify novel biomarkers that can enhance the diagnosis and management of AMI. Potential candidates include heart-type fatty acid-binding protein (H-FABP) and glycogen phosphorylase BB (GPBB). These biomarkers may offer earlier detection and additional prognostic information.
The integration of laboratory tests, particularly cardiac biomarkers, into clinical practice has significantly improved the diagnosis and management of AMI. Ongoing research into novel biomarkers holds promise for further enhancing patient outcomes.
Understanding STEMI vs. NSTEMI Diagnosis
Understanding the differences between STEMI and NSTEMI is essential for healthcare providers to deliver optimal care. The distinction between these two conditions is primarily based on electrocardiographic findings and has significant implications for treatment pathways (Rao et al., 2025).
Electrocardiographic Differentiation
The electrocardiogram (ECG) is a critical tool in differentiating between STEMI and NSTEMI. STEMI is characterized by ST-segment elevation in two or more contiguous leads, indicating complete occlusion of a coronary artery. In contrast, NSTEMI typically presents with ST-segment depression or T-wave inversion, suggesting partial or transient occlusion. Accurate interpretation of ECG findings is crucial for diagnosing and managing AMI effectively.
Clinical Implications of STEMI vs. NSTEMI
The clinical implications of STEMI versus NSTEMI are significant, as they guide immediate treatment decisions. Patients with STEMI require urgent reperfusion therapy, typically through primary percutaneous coronary intervention (PCI) or thrombolysis. In contrast, the management of NSTEMI often involves a more nuanced approach, including antiplatelet therapy, anticoagulation, and potentially invasive coronary angiography. Understanding these differences is vital for providing timely and appropriate care.
Early recognition and differentiation between STEMI and NSTEMI can significantly impact patient outcomes, as timely interventions can reduce morbidity and mortality associated with AMI.
Treatment Pathway Differences
The treatment pathways for STEMI and NSTEMI differ substantially. For STEMI, the focus is on immediate reperfusion to restore blood flow to the affected myocardium. This involves rapid assessment for primary PCI or thrombolytic therapy. In contrast, NSTEMI management involves risk stratification to identify patients who would benefit from an early invasive strategy versus those who can be managed conservatively. The choice of antithrombotic therapy and the timing of coronary angiography are also guided by the initial diagnosis.
- STEMI: Urgent reperfusion therapy (primary PCI or thrombolysis)
- NSTEMI: Risk stratification and potentially invasive coronary angiography
By understanding the differences between STEMI and NSTEMI, healthcare providers can tailor their approach to the specific needs of each patient, ultimately improving outcomes.
Advanced Diagnostic Technologies in AMI
Advanced diagnostic technologies are playing a crucial role in enhancing the diagnosis and management of AMI. The integration of innovative technologies is not only improving diagnostic accuracy but also enabling healthcare providers to make timely interventions.
Artificial Intelligence in ECG Interpretation
Artificial Intelligence (AI) is being increasingly utilized to enhance the interpretation of electrocardiograms (ECGs), a critical tool in diagnosing AMI. AI algorithms can analyze ECG data with high precision, identifying patterns that may elude human observers. This capability is particularly valuable in emergency settings where rapid diagnosis is paramount.
Key benefits of AI in ECG interpretation include:
- Enhanced accuracy in detecting AMI
- Reduced time to diagnosis
- Improved risk stratification
Recent studies have demonstrated the efficacy of AI-enhanced ECG interpretation. For instance, research by Rossello et al. (2025) highlighted the potential of AI to improve diagnostic accuracy and support clinical decision-making.
Deep Learning Algorithms for Risk Prediction
Deep learning algorithms are being explored for their potential to predict the risk of AMI. By analyzing vast datasets, including clinical variables and imaging data, these algorithms can identify complex patterns associated with increased risk.
The advantages of deep learning for AMI risk prediction include:
- The ability to analyze complex, multi-dimensional data
- Improved predictive accuracy compared to traditional risk models
- Potential for early identification of high-risk patients
Emerging Point-of-Care Diagnostic Tools
Point-of-care diagnostic tools are being developed to facilitate rapid AMI diagnosis in various clinical settings. These tools are designed to be portable, user-friendly, and capable of providing accurate results in real-time.
Some of the emerging technologies include:
- Portable ECG devices with AI-powered analysis
- Handheld troponin testing devices
- Microfluidic lab-on-a-chip technologies for biomarker detection
These advancements are poised to revolutionize AMI diagnosis, enabling healthcare providers to deliver timely and effective care.
Imaging Modalities in AMI Diagnosis
Advanced imaging modalities have revolutionized the way we diagnose and treat Acute Myocardial Infarction (AMI). Various imaging techniques, including echocardiography, coronary angiography, CT, and MRI, are used in the assessment of AMI, as noted by Byrne et al. (2023). These modalities provide critical information for diagnosis and treatment planning.
Echocardiography Applications
Echocardiography is a non-invasive imaging technique that plays a vital role in the diagnosis and management of AMI. It allows for the assessment of left ventricular function, detection of wall motion abnormalities, and evaluation of mechanical complications. Echocardiography is particularly useful in the acute setting due to its bedside availability and rapid results.
According to recent studies, echocardiography can also help in risk stratification by identifying patients with significant left ventricular dysfunction or other complications that may require immediate intervention.
Coronary Angiography Indications
Coronary angiography is an invasive imaging technique that provides detailed information about the coronary artery anatomy and the extent of coronary artery disease. It is indicated in patients with AMI who are candidates for revascularization, either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG).
The decision to proceed with coronary angiography is typically based on clinical presentation, electrocardiographic findings, and biomarker results. This procedure is crucial for identifying the culprit lesion and planning revascularization strategies.
Advanced Imaging Techniques (CT, MRI)
Advanced imaging techniques such as coronary computed tomography angiography (CCTA) and cardiac magnetic resonance (CMR) imaging are increasingly being used in the assessment of AMI. CCTA can provide detailed information about coronary artery anatomy without the need for invasive procedures.
CMR imaging, on the other hand, offers insights into myocardial tissue characterization, including the extent of infarction and the presence of microvascular obstruction. These advanced imaging modalities can aid in prognostication and guide long-term management.
As stated by experts, “Advanced imaging techniques are becoming integral to the diagnosis and management of AMI, offering a more comprehensive understanding of the disease process and facilitating personalized treatment plans.”
Comprehensive Treatment Strategies for AMI
AMI treatment is most effective when it includes a comprehensive strategy that encompasses pharmacological, interventional, and supportive measures. The complexity of AMI necessitates a multifaceted treatment approach that addresses the immediate need to restore blood flow to the affected myocardium, as well as long-term management to prevent further cardiovascular events.
Pharmacological Interventions
Pharmacological interventions play a crucial role in the management of AMI. These interventions are aimed at reducing myocardial oxygen demand, preventing further thrombosis, and managing symptoms.
- Antiplatelet Therapy: Dual antiplatelet therapy is a cornerstone in the treatment of AMI, involving the use of aspirin and a P2Y12 inhibitor to prevent platelet aggregation.
- Anticoagulation: Anticoagulants such as heparin are used to prevent further clot formation.
- Beta-blockers: These reduce myocardial oxygen demand by lowering heart rate and contractility.
- ACE Inhibitors/ARBs: They help in reducing mortality and preventing further cardiac remodeling.
As emphasized by recent guidelines, the early initiation of these pharmacological interventions is critical for improving outcomes in AMI patients (Silvain et al., 2024).
Reperfusion Strategies
Reperfusion strategies are pivotal in restoring blood flow to the ischemic myocardium. The choice between different reperfusion strategies depends on various factors, including the time from symptom onset and the availability of interventional cardiology services.
- Primary Percutaneous Coronary Intervention (PCI): This is considered the preferred reperfusion strategy when available in a timely manner.
- Fibrinolysis: When primary PCI is not readily available, fibrinolysis is an alternative reperfusion strategy.
The timely implementation of reperfusion strategies is crucial for salvaging the myocardium and improving survival.
Multidisciplinary Team Approach to AMI Care
The care of AMI patients benefits significantly from a multidisciplinary team approach, involving cardiologists, emergency medicine physicians, nurses, and other healthcare professionals. This team works together to ensure that patients receive comprehensive care, from initial assessment through to long-term management.
“A multidisciplinary approach to AMI care ensures that patients receive the most appropriate and timely interventions, improving outcomes and reducing mortality.”
Effective communication and coordination among team members are essential for delivering high-quality care. This includes clear documentation, regular team meetings, and a patient-centered approach to care.
Conclusion: Optimizing AMI Outcomes Through Evidence-Based Approaches
We have seen that optimizing AMI outcomes requires a multifaceted approach that incorporates the latest evidence-based practices in diagnosis and treatment. By leveraging advancements in medical imaging, such as CXCR4 PET/CT, and following recent guidelines (Rao et al., 2025; Byrne et al., 2023), we can significantly improve patient care and outcomes. For instance, a study involving 49 patients who suffered an acute myocardial infarction used a multimodal imaging protocol, demonstrating the potential of advanced imaging technologies to forecast recovery and inform treatment strategies following a heart attack, as reported in a study available on Bioengineer.org.
Evidence-based approaches to AMI enable healthcare providers to identify individuals at increased risk of adverse heart remodeling and heart failure, allowing for timely interventions. By adopting these approaches, we can enhance the quality of care and improve outcomes for AMI patients.
As we continue to advance in the field of cardiology, it is crucial that we remain committed to delivering care that is grounded in the latest research and technological advancements, ultimately optimizing AMI outcomes for our patients.
FAQ
What is Acute Myocardial Infarction (AMI)?
Acute Myocardial Infarction, commonly known as a heart attack, occurs when blood flow to the heart is severely blocked, causing damage to the heart muscle.
What are the classic symptoms of AMI?
Classic symptoms include chest pain or discomfort, often described as a pressure or tightness in the chest, shortness of breath, and pain or discomfort in one or both arms, the back, neck, jaw, or stomach.
How does AMI differ between men and women in terms of symptoms?
While both men and women may experience chest pain, women are more likely to have atypical symptoms such as abdominal pain, nausea, or fatigue, making diagnosis sometimes more challenging.
What are the risk factors for developing AMI?
Risk factors include modifiable factors like hypertension, high cholesterol, diabetes, and smoking, as well as non-modifiable factors such as age, family history, and genetic predisposition.
How is AMI diagnosed?
Diagnosis involves a combination of clinical assessment, electrocardiogram (ECG) changes, and laboratory tests, particularly cardiac biomarkers like troponin.
What is the difference between STEMI and NSTEMI?
STEMI (ST-Elevation Myocardial Infarction) is characterized by ST-segment elevation on an ECG, indicating a complete blockage of a coronary artery, while NSTEMI (Non-ST Elevation Myocardial Infarction) does not show ST-segment elevation, suggesting a partial blockage.
What are the treatment strategies for AMI?
Treatment involves pharmacological interventions such as anticoagulants and antiplatelet therapy, reperfusion strategies like primary percutaneous coronary intervention (PCI), and a multidisciplinary team approach to care.
How important is timely diagnosis and treatment in AMI?
Timely diagnosis and treatment are crucial as they directly impact outcomes, with early intervention significantly reducing mortality and improving the chances of a successful recovery.
What role do advanced diagnostic technologies play in AMI?
Advanced technologies, including artificial intelligence in ECG interpretation and deep learning algorithms for risk prediction, are enhancing diagnostic accuracy and personalizing treatment plans.
Can AMI be prevented?
While some risk factors cannot be changed, managing modifiable risk factors through lifestyle changes and medical therapy can significantly reduce the risk of developing AMI.
References:
• Mechanic, O. J., Gavin, M., Grossman, S., Ziegler, K. (2023). Acute Myocardial Infarction. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29083808/
• NHS. (n.d.). Diagnosing a heart attack. Retrieved from https://www.nhs.uk/conditions/heart-attack/diagnosis/
• AAFP. (2017). Acute Coronary Syndrome: Diagnostic Evaluation. Retrieved from https://www.aafp.org/pubs/afp/issues/2017/0201/p170.html
• American Heart Association. (n.d.). Diagnosing a Heart Attack. Retrieved from https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack
• PMC. (2023). Understanding Myocardial Infarction. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9463516/.