
Knowing about biliary drainage color is key for those recovering from liver or biliary surgery. The color of the drainage shows if bile drainage systems are working right.
Normal bile is yellow-green. Any change from this could mean trouble. Liv Hospital knows a lot about handling bile duct problems and infections. They stress the need for good care of bile drainage bags and biliary catheters.
It’s important to manage hepatic drainage well for recovery. Watching the drainage color is a big part of this. It helps doctors spot problems early.
Key Takeaways
- Monitoring biliary drainage color is vital for patient recovery after liver or biliary surgery.
- Normal bile color is typically yellow-green.
- Deviations in drainage color can indicate possible complications.
- Proper care for bile drainage bags and biliary catheters is essential.
- Liv Hospital’s expertise ensures high-quality care for patients needing advanced biliary interventions.
The Fundamentals of Biliary Drainage Systems
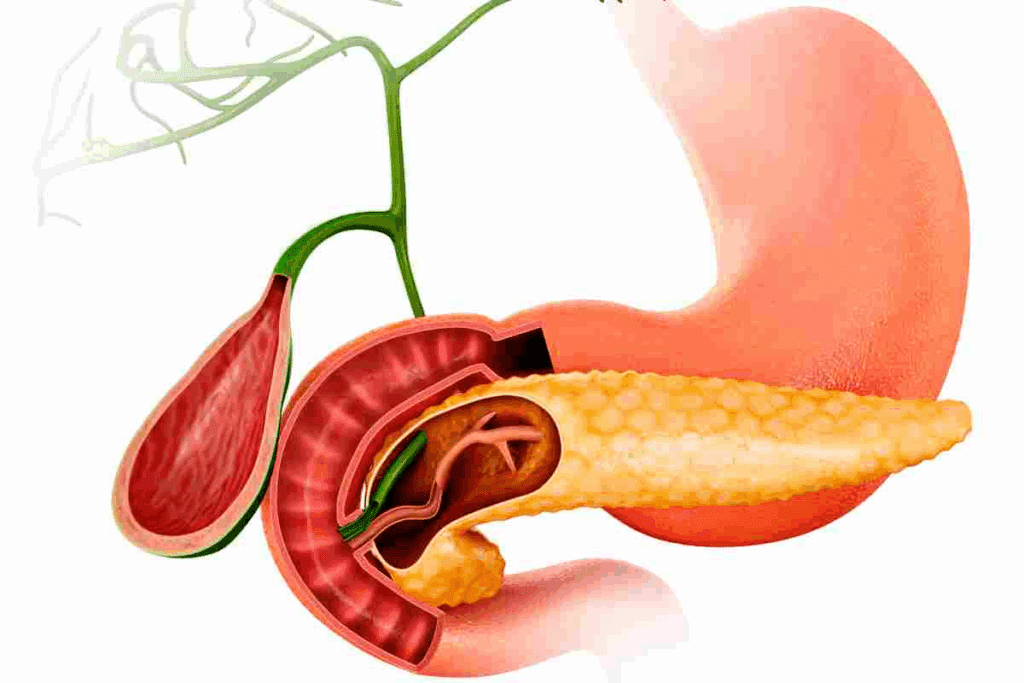
Understanding biliary drainage is key for managing liver and bile duct issues. Biliary drainage systems help remove blockages in the bile ducts. These blockages can be due to tumors, stones, or strictures.
To manage these blockages, doctors use catheters and drainage bags. This method is vital for patients with bile duct obstructions. It ensures bile flows properly into the intestine.
What is Biliary Drainage and Why It’s Performed
Biliary drainage is a medical procedure to clear bile duct obstructions. It’s often needed for conditions like pancreatic cancer, cholangiocarcinoma, or bile duct stones.
The main goal is to keep bile flowing into the intestine. This prevents issues like jaundice, cholangitis, and liver damage.
Components of Biliary Drainage Systems
Biliary drainage systems have important parts like bile catheters and drainage bags. The catheters are placed in the bile ducts to drain bile.
These catheters can be internal-external or external, based on the patient’s needs. The drainage bags collect the bile from the liver.
Percutaneous vs. Endoscopic Drainage Approaches
There are two main ways to do biliary drainage: percutaneous transhepatic cholangiography (PTC) and endoscopic retrograde cholangiopancreatography (ERCP). PTC goes through the skin, while ERCP uses an endoscope through the mouth.
The choice between these methods depends on the blockage’s location and the patient’s health.
Understanding Biliary Drainage Color: A Critical Clinical Indicator

Knowing the importance of biliary drainage color is key for good patient care. The color tells us a lot about the patient’s health and how well the biliary system is working.
Normal Yellow-Green Bile: What It Indicates
Normal bile is yellow-green, showing bile flows well from the liver to the bile ducts. This color comes from bile pigments like bilirubin. A yellow-green color means there are no big blockages and the liver is making and releasing bile right.
The Relationship Between Bile Color and Liver Function
The liver makes about a liter of bile every day, which goes to the gallbladder. The color of the bile shows how well the liver is working. For example, pale or clay-colored bile might mean there’s a problem with bile making or moving.
| Bile Color | Indication |
| Yellow-Green | Normal bile flow, effective liver function |
| Dark Brown | Possible bile duct obstruction |
| Pale/Clay | Potential issue with bile production or secretion |
How to Document and Monitor Color Changes
It’s very important to keep track of biliary drainage color for patient care. Doctors should check the color often and write down any changes. This helps spot problems early, like infections or blockages, so they can be treated quickly.
To keep an eye on drainage color, doctors should:
- Check the drainage bag regularly
- Record the color and any changes
- Note the volume and consistency of the drainage
- Report any significant changes to the healthcare team
Types of Biliary Drainage Bags and Their Functions
Biliary drainage bags are made for different needs. They collect bile from the liver or bile ducts. This is key for managing blockages in the biliary system.
External Bile Drainage Bags: Design and Usage
External bile drainage bags are for patients needing bile drained outside their body. They are made of strong, clean materials. They also have anti-reflux valves to stop bile from flowing back.
These bags have markers to track how much bile is drained. They are attached to a catheter or tube in the bile duct. Patients learn how to take care of these bags to avoid problems.
Bile Duct Drainage Bags for Post-Surgical Care
Bile duct drainage bags are for after bile duct surgery. They help watch bile flow and catch any issues early.
These bags are used until the bile duct heals or the patient gets better. They are made to be comfy and stay in place well.
Liver Drainage Bags: Special Considerations
Liver drainage bags are for special cases needing direct liver drainage. They handle the liver’s unique drainage needs, like different bile types and infection risks.
Handling liver drainage bags requires careful, clean technique. It’s also important to watch bile for signs of infection or blockage.
In summary, there are many biliary drainage bags for different needs. This helps improve patient care and results. Knowing about these bags is key for healthcare professionals to make the best choices.
Biliary Catheters: Varieties and Placement Techniques
Biliary catheters help drain bile from the liver or bile ducts. They are key in managing bile duct obstructions. They ensure bile flows into a drainage bag or into the intestine.
Bile Duct Catheters: Structure and Function
Bile duct catheters are made to fit inside bile ducts for proper drainage. They come in various materials, sizes, and designs. This depends on the patient’s needs and the procedure.
These catheters have a lumen for bile drainage. They might also have side holes for better drainage.
Internal-External Biliary Drainage Catheters
Internal-external biliary drainage catheters offer both internal and external bile drainage. They have side holes along their length. This allows bile to drain into the intestine or a drainage bag.
This dual function is great for managing complex biliary obstructions.
Biliary Drain Catheter Placement Procedures
Placing biliary drain catheters requires imaging guidance and interventional techniques. The method used can depend on whether it’s percutaneous or endoscopic. Common methods include percutaneous transhepatic cholangiography (PTC) and endoscopic retrograde cholangiopancreatography (ERCP).
The table below shows the main differences between various biliary catheter placement techniques:
| Placement Technique | Description | Advantages | Disadvantages |
| Percutaneous | Involves accessing the bile ducts through the skin | Effective for external drainage, can be used in emergency situations | Risk of infection, possible bile leakage |
| Endoscopic | Uses an endoscope to access the bile ducts | Less invasive, allows for internal drainage | Needs specialized equipment and expertise |
| Internal-External | Combines both internal and external drainage methods | Flexible in managing bile drainage | May need more complex catheter management |
It’s important for healthcare professionals to know about different biliary catheters and how they are placed. This knowledge helps in providing the best care for patients with biliary disorders.
Post-Cholecystectomy Drainage: Color Changes and Volume
Understanding drainage after gallbladder removal is key to spotting problems early. After surgery, patients often have drainage systems to manage bile flow.
Expected Drainage Color After Gallbladder Removal
The color of drainage after gallbladder removal can vary. It’s usually yellow or green because of bile. The exact shade depends on the patient’s health and any infections.
- Normal Bile Color: Yellow or green, showing normal bile production.
- Abnormal Colors: Dark brown or black might mean bile duct blockage. White or clay-colored bile could mean a lack of bile salts.
Normal Volume Ranges and Reduction Patterns
The amount of drainage after cholecystectomy is a key recovery sign. Drainage is usually highest right after surgery and then goes down as healing happens.
- Initial Volume: High volume is expected right after surgery.
- Reduction Pattern: Drainage volume should gradually go down over the next few days.
- Monitoring: It’s important to watch drainage closely to catch any unusual changes.
When Post-Surgical Drainage Indicates Complications
Changes in drainage color or volume can mean post-surgical problems. For example, more volume or darker color might show an obstruction or infection.
Key indicators of complications include:
- Increased Volume: May show an obstruction or infection.
- Change in Color: Darker colors or blood might mean complications.
- Persistent Drainage: If drainage doesn’t go down over time, it could be a sign of a problem.
Healthcare providers must watch post-cholecystectomy drainage closely. This ensures quick action if complications happen.
Abnormal Biliary Drainage Colors: Warning Signs and Meanings
Changes in biliary drainage color can signal serious health issues. These include obstruction, infection, or malignancy. It’s important to monitor the color of biliary drainage for early detection and intervention.
Dark Brown Drainage: Bile Duct Obstruction Indicators
Dark brown biliary drainage often indicates bile duct obstruction. This color change is due to bilirubin and its derivatives in the bile. Bile duct obstruction can be caused by gallstones, tumors, or inflammatory strictures.
Seeing dark brown drainage means you need to investigate further. This includes imaging studies like ultrasound or CT scans. They help find the cause and guide treatment.
White Bile in Malignant Biliary Obstruction
White bile, or “white bile syndrome,” is rare but significant. It’s often linked to malignant biliary obstruction. This happens when a tumor blocks the bile duct, causing mucinous material and desquamated epithelial cells to build up.
White bile is a sign of advanced disease. Treatment focuses on addressing the underlying malignancy through oncological interventions.
Bloody or Cloudy Drainage: Infection and Inflammation
Bloody or cloudy biliary drainage suggests infection or inflammation in the biliary system. Hemobilia, or bleeding into the biliary tree, can be caused by trauma, iatrogenic reasons, or vascular abnormalities.
Cloudy drainage may indicate pus or debris, pointing to infection. Quick evaluation and management are key. This includes antibiotics and possible drainage revision to prevent complications.
Essential Care and Maintenance of Biliary Drainage Systems
Proper care and maintenance of biliary drainage systems are vital. They directly affect patient outcomes and quality of life. Daily catheter care, bile drain bag management, and infection prevention are key. These steps help reduce complications from biliary drainage.
Daily Biliary Catheter Care Protocols
Daily care of biliary catheters is key to prevent infection and keep them working. Clean the catheter site with antiseptic solution and dress it with sterile gauze. Always check the catheter for damage or blockage.
Key steps in daily biliary catheter care include:
- Cleaning the catheter site with antiseptic solution
- Dressing the site with sterile gauze
- Inspecting the catheter for damage or blockage
- Flushing the catheter as directed by healthcare professionals
Bile Drain Bag Management Techniques
Managing bile drain bags properly is critical to avoid leakage and infection. Empty the bag regularly, clean it with soap and water, and make sure it’s securely attached. Teach patients how to do these tasks to keep things clean and prevent problems.
Preventing Infection and Dislodgement
To prevent infection and catheter dislodgement, use a multi-faceted approach. Use sterile techniques during catheter care, watch for infection signs like fever or redness, and secure the catheter well. Educate patients on recognizing complications and when to get medical help.
By sticking to these guidelines and being proactive, healthcare providers can greatly improve patient outcomes. This reduces the risk of complications from biliary drainage.
Troubleshooting Common Biliary Drainage Complications
Complications can happen with biliary drainage. This is a key procedure for those with bile duct blockages. But, like any treatment, it has risks that need quick action.
Addressing Catheter Blockages
Catheter blockages are a big problem in biliary drainage. They can cause less drainage, pain, and serious infections. Doctors use different methods to fix these blockages, like flushing with saline or using agents to break up clots.
The following table summarizes the steps to manage catheter blockages:
| Step | Description |
| 1. Assess the Catheter | Check for kinking or external compression. |
| 2. Flush the Catheter | Use sterile saline to clear blockages. |
| 3. Use Thrombolytic Agents | If flushing fails, consider thrombolytic agents. |
Managing Leakage Around Insertion Sites
Leakage around the insertion site is another issue. It can be caused by bad catheter placement, movement, or high biliary pressure. To fix it, doctors check the cause and take steps like adjusting the catheter or adding more drainage bags.
- Assessing the insertion site for signs of infection or irritation.
- Adjusting the catheter to ensure proper placement.
- Using additional support or drainage bags as needed.
When to Seek Immediate Medical Attention
It’s important for patients and caregivers to know when to get help fast. Look out for severe pain, big leaks, fever, or infection signs around the site. Quick action can stop serious problems and keep the drainage working well.
Patients should learn about complication signs and why getting help quickly is key.
Conclusion: Optimizing Patient Outcomes Through Proper Biliary Drainage Monitoring
Managing biliary drainage systems well is key to avoiding problems and getting the best results for patients. This is true for those going through hepatic drainage procedures.
Keeping an eye on biliary drainage helps doctors spot issues early. This lowers the chance of infections, catheter problems, and other complications. It’s all about keeping the drainage system working right.
Healthcare workers need to know how biliary drainage systems work. This includes understanding the importance of drainage color, the different types of bags, and how to place catheters. Knowing this helps them take better care of patients and improve their lives.
To get the best results, doctors should watch the drainage color, volume, and consistency closely. They should also act fast if they see anything off. This careful monitoring is what makes a big difference in patient care.
FAQ
What is the normal color of biliary drainage?
Normal biliary drainage is yellow-green. This shows the liver is working right and making bile.
What does dark brown biliary drainage indicate?
Dark brown biliary drainage might mean there’s a blockage in the bile duct. This could be due to gallstones or tumors.
How often should I check my biliary drainage bag?
You should check your biliary drainage bag often. Try to do it every few hours. Look at the color, volume, and how it’s flowing.
What are the different types of biliary catheters available?
There are many types of biliary catheters. These include bile duct catheters and internal-external biliary drainage catheters. There are also percutaneous transhepatic biliary drainage catheters.
How do I care for my biliary catheter?
To care for your biliary catheter, clean the insertion site daily. Check for blockages and make sure the catheter is secure to prevent it from coming out.
What are the signs of infection in biliary drainage?
Signs of infection include cloudy or bloody drainage, fever, chills, or pain in the belly. If you see these signs, get medical help right away.
Can I shower with a biliary drainage bag?
It’s best to avoid showering with a biliary drainage bag. Water can get into the catheter or bag and cause infection.
How long will I need to have a biliary drainage catheter?
How long you’ll need a biliary drainage catheter depends on your condition, treatment goals, and personal needs.
What are the possible complications of biliary drainage?
Complications can include blockages, leakage, infection, and the catheter coming out. These can be managed with good care and quick medical help.
How is biliary drainage color related to liver function?
Biliary drainage color is a key indicator of liver health. Changes in color can show liver problems, blockages, or other issues.
References
Bamias, A., et al. (2017). Current clinical practice guidelines for the treatment of renal cell carcinoma: A systematic review. Cancer Treatment Reviews, 53, 107-116. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5469586/










