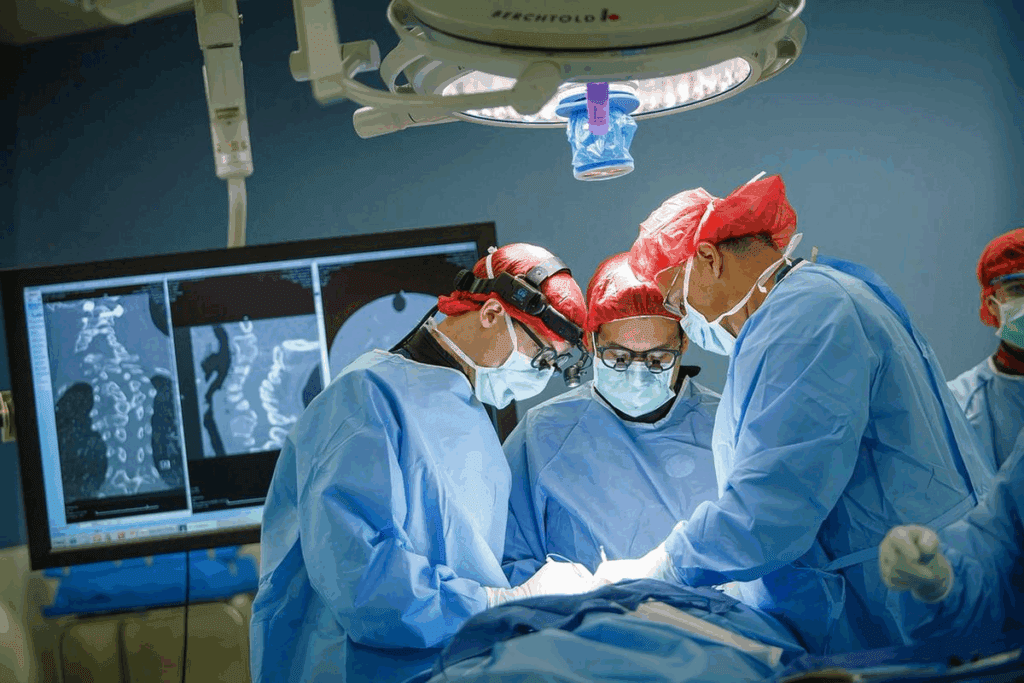
We understand the importance of interventional radiology procedures in today’s medicine. They are key for complex surgeries like Roux-en-Y Gastric Bypass (RYGB). Getting the right imaging insights is vital for a successful surgery.
RYGB is a detailed surgery needing careful attention before and after. Research shows that precise surgery radiology assessment is critical. It helps avoid problems and speeds up recovery with interventional radiology.
At Liv Hospital, we use the latest IR procedures for top-notch care. Our focus on international standards and patient needs helps patients get life-changing benefits from RYGB.
Key Takeaways
- Interventional radiology procedures improve patient outcomes for RYGB.
- Accurate imaging insights are key for successful RYGB surgery.
- Radiological assessment is essential before and after RYGB.
- Liv Hospital is dedicated to delivering exceptional patient care through IR procedures.
- Cutting-edge IR procedures reduce complications and improve recovery.
The Critical Role of Surgery Radiology in Bariatric Procedures

In bariatric surgery, radiology is key. It ensures patients get the best care before, during, and after surgeries like Roux-en-Y Gastric Bypass (RYGB). Advanced imaging has made these surgeries safer and more effective.
Evolution of Imaging Techniques in Weight Loss Surgery
Imaging has changed a lot in bariatric surgery. At first, plain radiographs and fluoroscopy were used. Now, CT imaging and MRI are essential for planning and checking up after surgery.
These new tools help doctors make accurate diagnoses and spot problems early. For example, CT scans can find internal hernias or bowel obstructions after RYGB.
Radiological Assessment Before and After RYGB
Checking with radiology is important before and after RYGB. It helps doctors plan and check on patients. This ensures the best results for patients.
Research shows that good radiology checks lower the risk of problems and improve results. IR procedures, like draining collections and checking for bleeding, are very helpful.
“The role of radiology in bariatric surgery is multifaceted, from pre-operative planning to post-operative care, and its importance cannot be overstated.”
| Imaging Modality | Pre-Operative Use | Post-Operative Use |
| CT Imaging | Assessing anatomy, identifying possible risks | Finding complications like internal hernias or bowel obstructions |
| Fluoroscopy | Looking at esophageal and gastric anatomy | Checking for leaks or strictures at the anastomosis site |
| MRI | Checking the liver and other specific needs | Looking for certain complications after surgery |
The table shows how different imaging tools are used before and after RYGB. These tools help doctors give better care and results.
IR procedures are also key in managing problems after RYGB. They help reduce serious issues, showing the importance of teamwork in patient care.
Understanding Roux-en-Y Gastric Bypass Anatomy Through Imaging
Imaging is key in understanding RYGB patients’ anatomy after surgery. We use different imaging methods to see the changes after RYGB. It’s important to correctly read these images to spot normal changes and any problems.
Normal Post-Surgical Radiological Appearance
After RYGB, the stomach is smaller and connected to a new part of the intestine. The gastrojejunal anastomosis is a key spot for radiologists to check. We use X-rays to see if the connection works right and if things move through it as they should.
The look of things on images can change based on the surgery. For example, how much stomach is left and the length of the new intestine can vary. Knowing these differences helps us understand what we see on images better.
Key Anatomical Landmarks for Radiologists
Radiologists need to know the important parts of RYGB patients’ anatomy. These include the gastrojejunal anastomosis, the connection between two parts of the intestine, and the stomach that’s left out. Finding these spots is important for spotting problems like leaks or blockages.
| Anatomical Landmark | Imaging Characteristic | Clinical Significance |
| Gastrojejunal Anastomosis | Narrowing at the anastomotic site | Potential stricture or leak |
| Jejunojejunal Anastomosis | Presence of a blind-ending stump | Potential site for internal hernia |
| Excluded Stomach | Non-opacification on upper GI series | Potential for complications like ulceration |
By knowing what to look for on images, radiologists can give accurate diagnoses. This helps doctors take better care of their patients. Imaging is a big part of managing RYGB patients, helping doctors make the best treatment plans.
Insight #1: Fluoroscopic Upper GI Series for Leak Detection
In RYGB, a fluoroscopic upper GI series is key for finding leaks. Leaks are a big problem after Roux-en-Y gastric bypass surgery. It’s important to find them quickly and correctly.
Technique and Protocol Optimization
To get the most from a fluoroscopic upper GI series, we focus on technique and protocol. We pick the right contrast agent and adjust the patient’s position. This ensures the images are clear and useful.
We use a water-soluble contrast agent to lower the risk of problems if a leak is found. We adjust the patient’s position to make sure the contrast flows well. This helps us see the anatomy clearly.
Interpretation of Normal vs. Abnormal Findings
Understanding normal and abnormal findings from a fluoroscopic upper GI series is key. Normal findings show the contrast flowing as expected through the stomach and small intestine.
Abnormal findings might show a leak or other issues like blockages. Getting these findings right is important for deciding what to do next.
| Normal Findings | Abnormal Findings |
| Expected flow of contrast through the gastric pouch and into the small intestine | Contrast extravasation indicating a leak |
| No signs of obstruction or stricture | Signs of obstruction or stricture |
Timing Considerations for Maximum Diagnostic Value
The timing of a fluoroscopic upper GI series is very important. Doing it too soon or too late can affect its accuracy.
We usually do this study a few days after surgery to catch early problems. The exact timing depends on the patient’s health and the surgeon’s advice.
Insight #2: CT Imaging for Post-RYGB Complications
CT imaging is key in spotting problems after Roux-en-Y Gastric Bypass (RYGB) surgery. It gives detailed images that help doctors find and fix issues quickly. This makes sure patients get the right care fast.
Identifying Internal Hernias and Bowel Obstructions
Internal hernias and bowel obstructions are big problems after RYGB. CT imaging is great at finding these because it shows the body’s inner workings clearly. For example, it can spot internal hernias by seeing bowel loops behind the superior mesenteric artery.
Research shows CT scans are very good at finding these issues. Using multi-planar reconstruction makes them even better. It gives a full view of the belly’s structures.
| Complication | CT Imaging Features | Clinical Significance |
| Internal Hernia | Bowel loops behind SMA, mesenteric swirl | Potential for bowel ischemia, requires prompt surgical intervention |
| Bowel Obstruction | Dilated bowel loops, transition point | May require surgical intervention to relieve obstruction |
| Anastomotic Stricture | Narrowing at anastomotic site, proximal dilation | Can cause dysphagia, may require endoscopic dilation |
Detection of Anastomotic Strictures
Anastomotic strictures can happen after RYGB. CT imaging spots these by showing the narrowing at the anastomotic site. This info helps plan treatments, like endoscopic dilation.
Vascular Complications Assessment
Vascular problems, like bleeding and thrombosis, can happen after RYGB. CT imaging, with contrast, checks the blood vessels. It finds any problems early, which is very important.
In short, CT imaging is very important for RYGB patients. It helps find and fix problems, making sure patients get the best care.
Insight #3: Interventional Radiology Procedures for RYGB Complications
Interventional radiology has changed how we handle Roux-en-Y gastric bypass (RYGB) issues. These small, non-invasive methods have greatly helped patients. They offer effective fixes for problems after surgery.
Image-Guided Drainage of Post-Operative Collections
Image-guided drainage is key for dealing with fluid buildup after RYGB. It uses images to guide the placement of drainage tubes. This way, surgery is often not needed.
Research shows this method works well. It cuts down on the need for more surgery. This approach also makes patients recover faster and spend less time in the hospital.
Angiography and Embolization for Post-RYGB Bleeding
Angiography and embolization are important for stopping bleeding after RYGB. Angiography helps find where the bleeding is. Then, embolization stops it by using special agents.
These methods are very effective. They help control bleeding well and often avoid the need for surgery.
Percutaneous Gastrostomy in the Excluded Stomach
Percutaneous gastrostomy is used for the excluded stomach after RYGB. It involves putting in a feeding tube under images. This helps with stomach issues.
This method is great when other ways can’t reach the stomach. It’s a safe and effective way to handle stomach problems after RYGB.
Using these interventional radiology methods, we can better handle RYGB issues. This leads to better results for patients and less complications.
Insight #4: MRI Applications in RYGB Assessment
MRI is now a key tool for checking on patients after Roux-en-Y Gastric Bypass (RYGB) surgery. It helps us see how the body has changed and spot any problems.
Advantages Over CT for Specific Complications
MRI beats CT scans in finding certain problems after RYGB. It’s great at spotting internal hernias without using harmful radiation.
Research shows MRI is very good at finding internal hernias. These can cause serious issues like bowel obstruction or ischemia if not caught early.
MR Enterography Techniques for RYGB Patients
MR enterography is a special MRI method. It uses a contrast agent to see the small bowel. It’s super helpful for RYGB patients with issues like bowel obstruction or internal hernias.
This technique gives us clear pictures of the Roux limb and other changes after surgery. It helps us make the right treatment plans.
Hepatobiliary Imaging Post-RYGB
MRI is also great for checking liver and bile duct problems after RYGB. Fast weight loss can lead to gallstones in these patients.
MRI can spot gallbladder disease and other liver and bile duct issues. This helps us figure out the best way to treat them.
| Imaging Modality | Advantages | Limitations |
| MRI | No ionizing radiation, high sensitivity for internal hernias | Higher cost, longer examination time |
| CT | Quick examination time, widely available | Ionizing radiation, less sensitive for certain complications |
Insight #5: Ultrasound Utilization in RYGB Follow-up
Ultrasound is a key tool in managing RYGB patients after surgery. It helps us watch for complications and see how well the surgery worked.
Gallstone Detection and Management Post-RYGB
Ultrasound is great for finding gallstones in RYGB patients. Gallstones are more common after this surgery. We check for gallstones early to treat them quickly.
Gallstone detection is important because untreated gallstones can cause serious problems. Ultrasound lets us find gallstones without surgery, helping us treat them fast.
Abdominal Wall Complications Assessment
Ultrasound is also good for checking the abdominal wall after RYGB. We look for hernias, hematomas, or other issues. This helps us know who needs more treatment.
Using ultrasound, we can non-invasively check the abdominal wall. This helps us find problems early and improve patient care.
Limitations and Optimization Strategies
Ultrasound has its limits. Things like the skill of the person using it and the patient’s body shape can affect how clear the images are. To get the best results, we use high-frequency probes and adjust settings for each patient.
Knowing the limits and using these strategies helps us get the most out of ultrasound in RYGB follow-up care.
Insight #6: 3D Reconstruction and Virtual Surgical Planning
3D reconstruction and virtual surgical planning have changed Roux-en-Y gastric bypass surgery. They give surgeons detailed, interactive models of patient anatomy. This helps with preoperative planning and improves surgical results.
Preoperative Mapping of Vascular Anatomy
3D reconstruction is key in RYGB surgery for mapping vascular anatomy. Accurate visualization of blood vessels is vital to avoid surgery complications. Studies show 3D reconstruction helps identify key vascular structures better. This reduces the risk of bleeding and other vascular issues.
- Enhanced visualization of arterial and venous anatomy
- Improved identification of possible bleeding sites
- Better planning for vascular clamping and ligation
A study in the Journal of Surgical Research found, “Preoperative 3D reconstruction enhances understanding of complex anatomy. This leads to more precise surgical planning.”
Volume Rendering Techniques for Complex Cases
Volume rendering techniques are essential for complex RYGB cases. They create detailed 3D models from CT or MRI scans. This helps surgeons understand the patient’s anatomy and plan their approach.
Volume rendering allows for detailed models that can be viewed from different angles. This is very useful for complex cases with multiple adhesions or anatomical variations.
Integration with Surgical Navigation Systems
The combination of 3D reconstruction and virtual surgical planning with surgical navigation systems is a big step forward in RYGB surgery. It allows for more precise and accurate surgery by combining preoperative planning with real-time navigation.
“The fusion of 3D reconstruction with surgical navigation systems has the power to further reduce complications and improve patient outcomes in RYGB surgery.” – Expert Opinion
This integration lets surgeons correlate their preoperative plans with the actual surgical site. They can make adjustments in real-time. This leads to a more precise and controlled surgery.
Insight #7: Artificial Intelligence in RYGB Imaging Analysis
The use of artificial intelligence (AI) in RYGB imaging analysis is changing bariatric radiology. It’s making diagnosis more accurate and efficient.
Machine Learning for Complication Prediction
Machine learning algorithms are now used to predict complications in RYGB patients. They look at big datasets to find patterns that doctors might miss.
Research shows these algorithms can spot issues like internal hernias and bowel obstructions with great accuracy. This helps doctors act early, which can lower the risk of serious problems.
Automated Measurement of Post-Surgical Anatomy
AI tools are also used to measure post-surgical anatomy in RYGB patients. They check the size of the gastric pouch, the stoma diameter, and the Roux limb length.
These automated measurements are more consistent than manual ones. They give doctors reliable data for making decisions.
Current Limitations and Future Potentials
AI has a lot of promise for RYGB imaging, but there are some hurdles. These include needing good training data, avoiding bias, and getting regulatory approval.
Despite these challenges, AI’s future in RYGB imaging looks bright. As technology gets better, we’ll see more advanced algorithms. They’ll use more data, like imaging, clinical, and genomic information.
| AI Application | Current Status | Future Potentials |
| Machine Learning for Complication Prediction | High accuracy in predicting internal hernias and bowel obstructions | Integration with clinical data for more complete risk assessment |
| Automated Measurement of Post-Surgical Anatomy | Reliable measurements of gastric pouch size and stoma diameter | Expansion to measure more anatomical parameters |
| AI-powered Imaging Analysis | Enhanced detection of post-surgical complications | Real-time analysis during surgical procedures |
Conclusion: Integrating Radiological Insights for Optimal RYGB Patient Care
We’ve seen how surgery radiology is key in Roux-en-Y gastric bypass (RYGB) procedures. It’s vital for better patient care. By using insights from imaging, we can make RYGB care and results better.
Research shows that a full approach to RYGB care leads to better results. IR procedures like image-guided drainage help manage post-op issues. These steps help us give RYGB patients the best care, cutting down on problems and boosting their life quality.
As we move forward in surgery radiology, we must keep radiological insights at the heart of RYGB care. This way, we ensure patients get top-notch care, with better results and fewer complications.
FAQ
What is the role of interventional radiology in Roux-en-Y Gastric Bypass (RYGB) procedures?
Interventional radiology (IR) is key in RYGB. It uses minimally invasive methods to manage complications. This helps reduce risks and improves patient results.
What are the most common IR procedures used in RYGB?
IR in RYGB includes draining collections and treating bleeding. It also involves creating a new stomach opening. These steps help manage post-surgery issues.
How does fluoroscopic upper GI series help in leak detection after RYGB?
This imaging method uses contrast to see the GI tract. It spots leaks by showing where there shouldn’t be connections.
What is the importance of CT imaging in post-RYGB complications?
CT scans are vital for finding complications like hernias and strictures. They help doctors act quickly to improve patient care.
How does MRI contribute to RYGB assessment?
MRI, like MR enterography, helps find issues like bowel obstructions. It’s safe and useful, often better than CT scans for some problems.
What is the role of ultrasound in RYGB follow-up care?
Ultrasound checks for gallstones and abdominal issues. It’s a non-invasive way to monitor patients after surgery.
How does 3D reconstruction and virtual surgical planning aid in RYGB?
These tools help plan surgeries by mapping anatomy. They improve precision and reduce risks during surgery.
What are the applications of artificial intelligence in RYGB imaging analysis?
AI uses algorithms to predict issues and measure anatomy. It’s a new tool that could make diagnoses more accurate, but it’s not yet perfect.
What is the significance of understanding RYGB anatomy for radiologists?
Knowing RYGB anatomy is critical for radiologists. It helps them spot problems and guide treatment, leading to better patient care.
How do IR procedures reduce complications in RYGB patients?
IR procedures offer non-invasive solutions for complications. They help manage issues like collections and bleeding, reducing risks and speeding recovery.
References
Majumdar, A., et al. (2024). Current trends in herbal medicines targeting renal cell carcinoma. Phytomedicine, 131, 152837. https://www.sciencedirect.com/science/article/abs/pii/S2950199724001174



































