In today’s world, understanding medical intervention is essential for making informed healthcare decisions. Many patients and readers wonder about the interventional medical meaning and what it involves in real-world healthcare.
At Liv Hospital, we focus on patient-centered care and use the latest medical techniques. Interventional medical meaning refers to a broad range of actions taken to diagnose, treat, or manage health conditions. These can include administering medications, performing minimally invasive procedures, or conducting surgeries that improve patient outcomes.
Medical interventions play a vital role in maintaining health and preventing complications. Understanding the interventional medical meaning helps patients appreciate the purpose and benefits of these procedures. By knowing what interventions involve, patients can make smarter choices about their care and feel confident in their treatment plans.
Key Takeaways
- Understanding medical interventions is key for everyone in healthcare.
- Medical interventions include many actions, like tests and treatments.
- The World Health Organization says these actions are a wide range.
- These interventions aren’t just about treating but also preventing health issues.
- Making informed choices about care is important for patient care.
The Complete Scope of Healthcare Interventions
Understanding healthcare interventions is key to better patient care and health systems worldwide. These interventions are a big part of healthcare systems. They aim to improve patient outcomes, stop disease, and boost health.
The World Health Organization (WHO) is very important in guiding healthcare interventions. The WHO says health interventions are actions to better health outcomes, stop disease, and promote health. This shows how wide-ranging healthcare interventions are.
World Health Organization’s Framework
The WHO’s framework helps us understand the scope and effect of healthcare interventions. Healthcare interventions are divided into types like preventive, diagnostic, therapeutic, and rehabilitative. Each type is vital for patient care.
“Health interventions are key for universal health coverage and better health outcomes,” the WHO stresses in its global health efforts.
The WHO’s framework highlights the need for evidence-based practices in healthcare interventions. This ensures interventions are effective, efficient, and fair.
Impact on Patient Care and Health Systems
Healthcare interventions have a big impact on patient care and health systems. Good interventions lead to better health, happier patients, and more efficient systems. For example, preventive actions can cut disease rates, while treatments can manage chronic conditions better.
By grasping the wide scope of healthcare interventions, we see their big role in bettering patient care and health systems. The WHO’s framework is a great tool for healthcare workers, policymakers, and patients.
Key Definition 1: Diagnostic Interventions
In healthcare, diagnostic interventions are key to figuring out and diagnosing medical issues. They help doctors create good treatment plans. The World Health Organization says, “Diagnostic accuracy is essential for improving health outcomes.”
“Diagnostic accuracy is essential for improving health outcomes.”
World Health Organization
Purpose and Types of Diagnostic Procedures
Diagnostic procedures aim to accurately identify and diagnose medical conditions. They range from simple lab tests to complex imaging techniques. Laboratory tests, like blood and urine analyses, give vital info about a patient’s health.
We use many diagnostic procedures to get a full picture of a patient’s health. These include:
- Laboratory tests (blood, urine, etc.)
- Imaging tests (X-rays, ultrasounds, etc.)
- Endoscopic procedures
From Laboratory Tests to Advanced Imaging
Advanced imaging, like MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans, gives detailed views of the body’s inside. These tools help doctors diagnose complex conditions better.
As medical tech gets better, so do diagnostic interventions. This leads to more accurate and less invasive ways to diagnose. It improves patient care and treatment results.
Key Definition 2: Preventive Interventions

Preventive interventions are key in healthcare. They aim to stop disease and boost well-being. These efforts help lower illness risk and enhance life quality.
Primary Prevention Strategies
Primary prevention stops disease before it starts. We use vaccines, health talks, and lifestyle changes. These steps are vital for public health.
Some main primary prevention strategies are:
- Immunization against infectious diseases
- Promoting healthy lifestyles through diet and exercise
- Conducting health education campaigns
Secondary and Tertiary Prevention Approaches
Secondary prevention finds disease early, often before symptoms show. Tertiary prevention manages and lessens disease complications. We use screenings and early actions for these goals.
| Prevention Type | Objective | Examples |
| Primary Prevention | Prevent disease before it occurs | Vaccination, health education |
| Secondary Prevention | Detect disease early | Screening programs, early intervention |
| Tertiary Prevention | Manage and reduce complications | Disease management, rehabilitation |
By using these preventive steps, we can greatly improve health outcomes and cut healthcare costs.
Key Definition 3: Therapeutic Interventions
In healthcare, therapeutic interventions are key to better patient outcomes and quality of life. They are vital for treating and managing many medical conditions. This improves the healthcare experience for everyone.
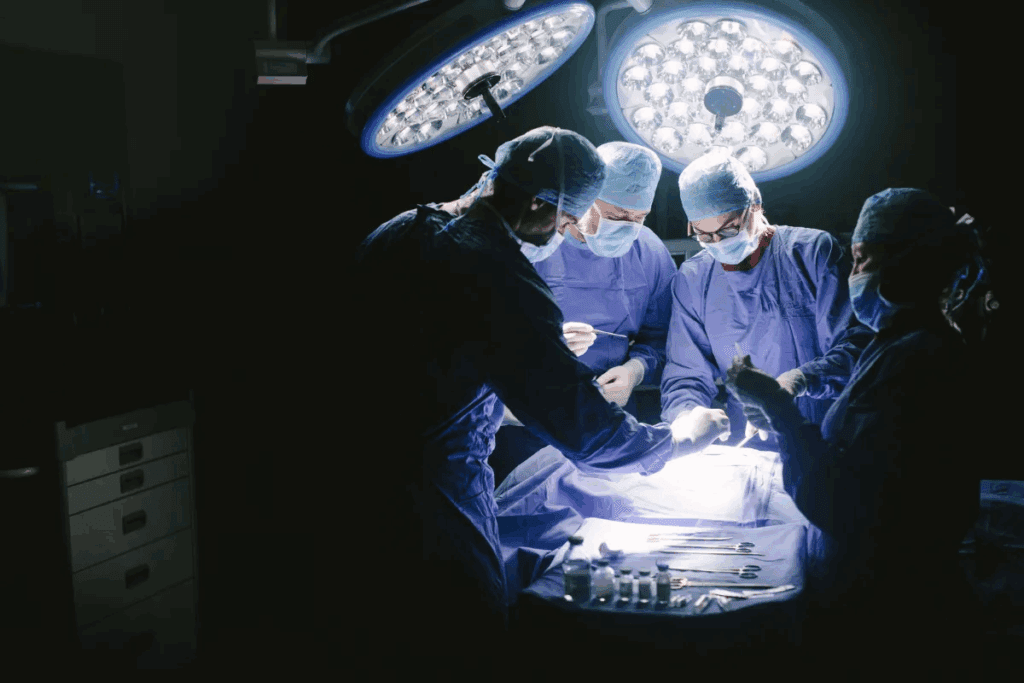
Acute Care Treatment Methodologies
Acute care treatment is essential for immediate health needs. It includes various treatments and interventions for acute conditions. Timely and appropriate acute care is key to preventing complications and improving patient outcomes.
Some important aspects of acute care include:
- Emergency response and stabilization
- Surgical interventions
- Intensive care unit (ICU) management
Chronic Disease Management Approaches
Chronic disease management is vital for long-term patient care. It focuses on managing chronic conditions over time. This improves quality of life and reduces healthcare costs. Effective chronic disease management involves a team approach, patient education, and ongoing monitoring.
| Disease | Management Approach | Key Interventions |
| Diabetes | Lifestyle modification and medication | Monitoring blood glucose, dietary counseling |
| Hypertension | Medication and lifestyle changes | Blood pressure monitoring, stress reduction techniques |
| Asthma | Inhaler therapy and trigger avoidance | Peak flow monitoring, asthma action plans |
By understanding and using these therapeutic interventions, we can greatly improve patient outcomes. This also enhances the quality of care provided.
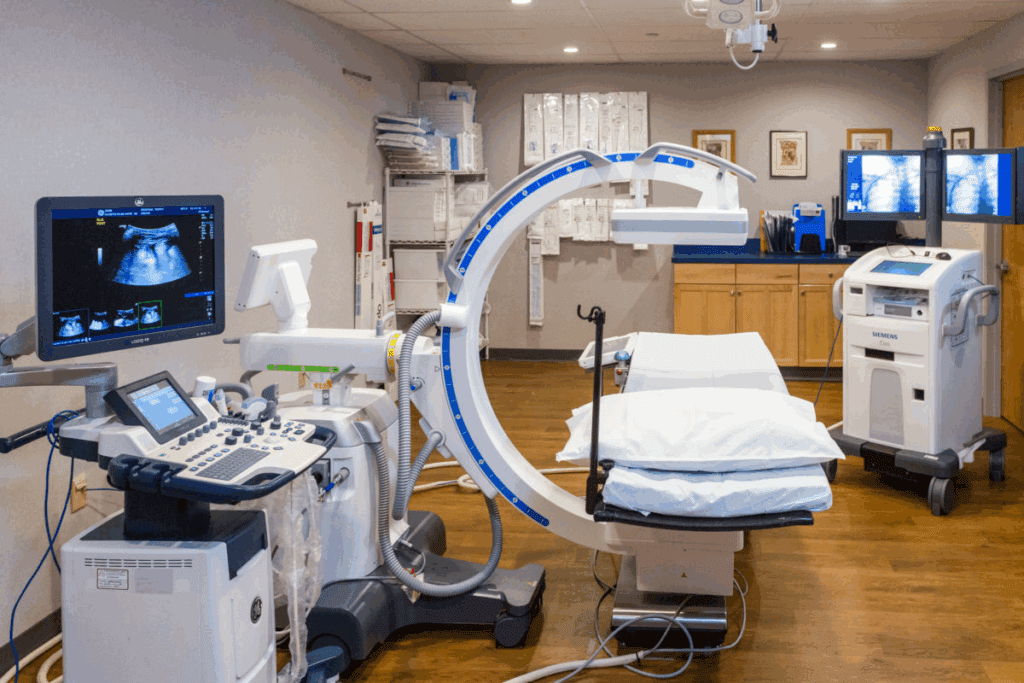
Key Definition 4: Interventional Medical Meaning and Procedures
Interventional medical procedures have changed healthcare a lot. They offer new ways to diagnose and treat many health issues. These methods help doctors do complex tasks with less risk and better results for patients.
Interventional medical procedures use new tech and methods to treat without big surgery. They are minimally invasive, which means they cause less damage and help patients heal faster.
Minimally Invasive Techniques
Minimally invasive techniques are key in these procedures. They use small cuts, special tools, and imaging to do detailed work. This way, we can lower the chance of problems and help patients get better quicker.
- Reduced risk of infection
- Faster recovery times
- Less post-operative pain
- Improved cosmetic outcomes
Cardiac Catheterization and Endoscopic Procedures
Cardiac catheterization and endoscopic procedures are big changes in patient care. Cardiac catheterization uses a catheter to check and fix heart problems. Endoscopic procedures use a tube with a camera and tools to look at and treat body issues, like stomach problems.
These methods have made diagnosing and treating health issues more accurate and effective. They help us give better care to those with complex health problems.
Key Definition 5: Medication Intervention Meaning
Medication interventions are key in treating many health issues. They involve giving medicines to help patients. This ensures they get the best care for their health needs.
Pharmaceutical Treatment Protocols
Pharmaceutical treatment protocols help improve treatment results. They follow proven methods and are made for specific health problems. Effective treatment protocols take into account the patient’s health, how medicines interact, and possible side effects.
Let’s look at a sample protocol for managing high blood pressure:
| Protocol Component | Description | Clinical Consideration |
| Medication Selection | Choosing the right blood pressure medicine for the patient. | Think about other health issues and how medicines might interact. |
| Dosing Regimen | Figuring out the best dose and how often to take it. | Watch how the patient responds and adjust as needed. |
| Monitoring Requirements | Checking blood pressure and side effects regularly. | Change the treatment plan based on how the patient is doing and new information. |
Patient Safety and Medication Adherence
Patient safety is very important in medicine. Medication errors can be very harmful. We work to keep patients safe by using clear labels and teaching them how to use their medicines right.
Getting patients to stick to their medication is also key. We make it easier for them by simplifying how often to take it, using reminders, and teaching them why it’s important. Improving medication adherence helps treatment work better and saves money by avoiding complications from not taking medicine as directed.
Key Definition 6: Rehabilitative Interventions
Rehabilitative interventions are key to helping patients with disabilities. They aim to restore function and improve life quality. Patients regain strength, mobility, and independence, making it easier to live daily lives.
We use a wide range of therapies to meet each patient’s needs. This approach ensures effective treatment for physical, cognitive, and emotional challenges.
Physical and Occupational Therapy Approaches
Physical and occupational therapy are vital in rehab. Physical therapy works on physical function, mobility, and strength. Occupational therapy helps with daily living skills and independence.
Our physical therapy programs aim to improve range of motion and reduce pain. We use manual therapy, exercise, and modalities like heat or cold therapy.
Occupational therapy focuses on daily tasks and activities. Therapists help develop strategies for daily routines and improve fine motor skills.
| Therapy Type | Focus | Techniques |
| Physical Therapy | Restoring physical function and mobility | Manual therapy, exercise programs, modalities |
| Occupational Therapy | Developing skills for daily living | Task-specific training, adaptive equipment, environmental modifications |
Cognitive and Psychological Rehabilitation
Cognitive and psychological rehabilitation are critical parts of care. They address cognitive impairments, emotional challenges, and behavioral issues. This promotes overall well-being and recovery.
Cognitive rehabilitation programs target specific cognitive deficits. Therapists use strategies to help patients compensate and improve cognitive function.
Psychological rehabilitation tackles emotional and psychological challenges. Therapists offer counseling, cognitive-behavioral therapy, and other interventions to support emotional well-being.
We combine physical, occupational, cognitive, and psychological rehabilitation for complete care. This holistic approach helps patients recover fully, regain independence, and enhance their quality of life.
Key Definition 7: Public Health Interventions
Public health interventions are wide-ranging strategies aimed at improving health and preventing disease. They are key in tackling health issues at various levels, from local to national.
Population-Level Intervention Strategies
These strategies focus on health promotion and disease prevention for all. We use different programs to achieve this, including:
- Health Education: Teaching people about healthy habits and disease prevention.
- Vaccination Programs: Running vaccination campaigns to stop infectious diseases from spreading.
- Disease Surveillance: Watching for disease outbreaks to act quickly.
Our goal is to be proactive, aiming to lower disease rates and boost overall health.
Health Policy as Preventive Intervention
Health policy is vital in shaping public health. By creating and enforcing policies that support health, we can greatly improve population health. For example:
- Legislation to curb tobacco use and lower smoking-related illnesses.
- Regulations to ensure food and water safety.
- Policies to encourage physical activity and healthy eating.
Good health policy is a strong tool for prevention. It helps create environments that support healthy choices and reduce health gaps.
In summary, public health interventions, including strategies for populations and health policy, are vital for better health outcomes. By understanding and applying these, we can strive for a healthier future for everyone.
Evidence-Based Protocols in Modern Medical Practice
Modern medicine uses evidence-based protocols to make decisions. These protocols make sure treatments are safe and work well. This leads to better health outcomes for patients. It’s key to keep using evidence-based practice in our daily work.
Developing Interventions with Research-Driven Design
Creating treatments based on research is vital. Healthcare pros use new research to make treatments fit each patient’s needs. This makes treatments more effective and safer. We always update our knowledge with new studies.
Creating treatments involves several steps:
- Identifying the clinical problem or need
- Conducting a thorough review of existing literature
- Designing the intervention based on the evidence gathered
- Testing and refining the intervention
Enhancing Quality through Measurement and Improvement
Measuring and improving quality is key. It helps make sure protocols work well in real life. By checking results and making changes, we can do better. This keeps care at a high level.
We use different metrics to check quality:
| Metric | Description | Target |
| Patient Satisfaction | Measures patient feedback and satisfaction with care | 90% or higher |
| Treatment Outcomes | Assesses the effectiveness of interventions | 85% or higher success rate |
| Adverse Events | Tracks the incidence of adverse events | Less than 5% |
By using research and quality checks, we make sure our protocols work. This approach is key to top-notch patient care today.
The Rise of Personalized Medicine in Interventions
Personalized medicine is changing healthcare by making treatments fit each patient’s needs. This method has become more popular because it can lead to better health outcomes and lower costs.
We’re seeing a big move towards genetic and biomarker-based approaches in medical care. These new tools help doctors create treatments that work better and cause fewer side effects.
Genetic and Biomarker-Based Approaches
Genetic and biomarker-based methods are being used more in medicine. They help doctors find the right treatments by looking at a patient’s genes. This way, they can create personalized treatment strategies.
In cancer treatment, for example, genetic tests can find the exact cause of the cancer. This lets doctors use targeted therapies that are more effective and safer than old treatments.
Patient-Centered Intervention Planning
Patient-centered planning is key in personalized medicine. It means making medical plans that fit each patient’s needs and wants. This makes sure care is both effective and easy for the patient.
Doctors consider things like a patient’s history, lifestyle, and what they prefer. This helps create patient-centered care plans that make patients more involved and happy. It also helps them stick to their treatment plans.
As we keep moving forward in personalized medicine, focusing on patient-centered care is vital. We must make sure medical plans are made with each patient in mind.
Integrated Care Pathways: Case Study of Liv Hospital
Integrated care pathways are key in modern healthcare, with Liv Hospital leading the way. These paths coordinate care across different settings, using proven methods to better patient results. Liv Hospital has made its care better and faster by streamlining these processes.
Academic Protocol Integration
Liv Hospital bases its care paths on academic protocol integration. It works with schools to create and use the newest care methods. This ensures patients get the best and latest treatments.
The hospital’s teams include experts from many fields. They work together to make detailed care plans. This teamwork helps Liv Hospital meet complex patient needs, leading to better results and happier patients.
International Standards and Competitive Outcomes
Liv Hospital follows international standards closely. This helps it achieve top results that are known worldwide. Its dedication to excellence has made it a top name in healthcare.
The hospital’s focus on quality care has led to better patient results and more efficient work. By using integrated care paths, Liv Hospital has cut down on hospital stays and complications. This has made the patient experience better.
As healthcare keeps changing, Liv Hospital’s approach is a great example for others. By following similar paths, hospitals everywhere can improve their services. This will lead to better care and results for patients.
Conclusion: The Evolving Landscape of Medical Interventions
Medical interventions are key in healthcare, shaping how patients do. The field is always changing, thanks to new tech, research, and patient needs. We’ve looked at what medical interventions are, their types, and their importance.
The future of medical care will bring new trends like personalized medicine. Places like Liv Hospital are already seeing these changes help patients. Keeping up with new medical advancements helps us give better care to our patients.
Healthcare is always evolving, and we’re committed to top-notch care. The changing world of medical interventions brings both chances and challenges. We’re ready to face these to make patient care better.
FAQ
What is a medical intervention?
A medical intervention is any action by healthcare professionals to help or treat a medical issue. This can range from tests and preventive steps to treatments and rehabilitation.
What are the different types of medical interventions?
There are many types of medical interventions. These include diagnostic tests, preventive steps, treatments, and more. They also include procedures, medication, and public health efforts.
What is the purpose of diagnostic interventions?
Diagnostic interventions help find and diagnose medical issues. They include tests and studies to get accurate information.
What are preventive interventions, and why are they important?
Preventive interventions aim to stop diseases and keep people healthy. They include vaccinations, health education, and screenings.
What are therapeutic interventions, and how are they used?
Therapeutic interventions treat and manage health issues. They include acute care and chronic disease management.
What are interventional medical procedures, and what are their benefits?
Interventional medical procedures are small, non-invasive ways to diagnose and treat. They include procedures like cardiac catheterization.
What is the role of medication interventions in healthcare?
Medication interventions use drugs to treat health issues. They require careful planning and focus on patient safety and adherence.
What are rehabilitative interventions, and how do they support patients?
Rehabilitative interventions help patients with disabilities. They include physical therapy and cognitive rehabilitation to improve quality of life.
What are public health interventions, and why are they important?
Public health interventions aim to improve health at a population level. They include health policies and initiatives.
What is the significance of evidence-based protocols in medical practice?
Evidence-based protocols make sure interventions are safe and effective. They are based on research and quality improvement.
What is personalized medicine, and how is it used in interventions?
Personalized medicine uses genetic information to tailor treatments. It improves patient care by focusing on individual needs.
What are integrated care pathways, and how do they improve patient care?
Integrated care pathways coordinate care across settings. They ensure care is complete, coordinated, and effective for better patient outcomes.








