Last Updated on November 25, 2025 by Ugurkan Demir
It’s important to know the difference between coronary artery disease and atherosclerosis of the native coronary artery. At Liv Hospital, we focus on top-notch cardiac care for our patients.Learn what athscl heart disease of native coronary artery means and how it differs from other forms of atherosclerosis.
Atherosclerosis is a widespread issue that can harm many arteries, including the ones in the heart. Coronary artery disease (CAD) happens when atherosclerosis blocks the heart’s arteries, reducing blood flow.
Using the right medical terms is key to diagnosing and treating these conditions. We’ll look into the causes, signs, and treatments for both. This will help you make informed health choices.
Key Takeaways
- Coronary artery disease is a sign of atherosclerosis in the heart’s arteries.
- Atherosclerosis is a widespread issue that affects many arteries.
- Knowing the difference between these conditions is vital for accurate diagnosis.
- Effective treatment relies on precise medical terms.
- Liv Hospital is committed to providing top healthcare with full support.
Cardiovascular Disease Terminology Explained
Understanding cardiovascular disease terms is key for diagnosis and treatment. It’s important for both doctors and patients to make informed decisions.
Key Definitions in Heart Disease
Atherosclerosis is when plaque builds up in arteries, leading to heart diseases. Coronary Artery Disease (CAD) happens when this buildup affects the heart’s arteries, reducing blood flow. Angina pectoris is chest pain from reduced blood to the heart muscle.
Knowing the difference between these terms is critical. For example, atherosclerosis of the coronary artery without angina pectoris means plaque in the heart’s arteries without chest pain. Yet, it can cause serious problems if not treated.
Why Precise Medical Terminology Matters
Using exact medical terms is vital for correct diagnosis and treatment plans. It ensures patients get the right care. For instance, knowing the difference between coronary atherosclerosis and CAD helps tailor treatments.
Accurate terms also improve communication among doctors and between doctors and patients. It prevents confusion and keeps everyone on the same page.
In cases of athSCL heart disease of native coronary artery w/o ang pctrs, clear terms help spot at-risk patients early. This allows for timely action.
Atherosclerosis: The Foundation of Arterial Disease
Atherosclerosis is a condition where plaque builds up in the walls of arteries. It’s a key part of arterial disease. We’ll look into how it develops and its effects on the body.
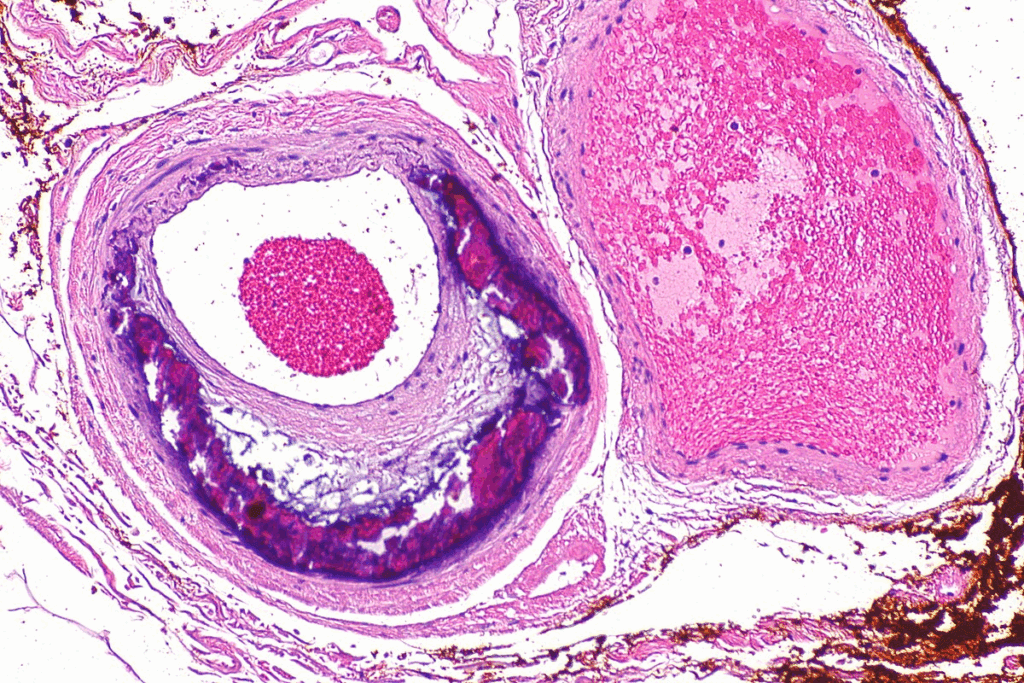
The Pathophysiology of Plaque Formation
Plaque formation in atherosclerosis involves cholesterol, inflammatory cells, and other substances. This buildup causes inflammation. It can make the plaque unstable and lead to severe heart problems.
The process of atherosclerosis is complex. It involves lipid metabolism, inflammatory responses, and problems with the endothelium. We’ll dive into these factors to understand how they contribute to plaque formation.
Systemic Nature of Atherosclerotic Disease
Atherosclerosis isn’t just in one area; it’s a systemic disease. It can affect many parts of the body. For example, atherosclerosis in the coronary arteries might show a bigger problem.
This systemic nature of atherosclerosis is important for diagnosis and treatment. It shows why we need to manage the whole cardiovascular risk of a patient, not just one area.
| Aspect | Description | Clinical Implication |
| Plaque Formation | Accumulation of cholesterol and inflammatory cells | Increased risk of cardiovascular events |
| Systemic Nature | Affects multiple vascular beds | Need for a complete management plan |
| Inflammatory Response | Key role in plaque development and instability | Target for therapeutic interventions |
Understanding atherosclerosis helps us see the complexity of atherosclerotic heart disease. It shows how it’s linked to coronary artery disease (CAD).
Coronary Artery Disease: When Atherosclerosis Affects the Heart
Atherosclerosis in the coronary arteries leads to coronary artery disease. This condition harms heart health. It’s a big reason for sickness and death around the world. We’ll look at what CAD is, why it matters, and how it affects health and life quality.
Definition and Clinical Significance of CAD
CAD happens when the coronary arteries narrow or block. This cuts down blood flow to the heart. It can cause angina, heart attacks, and serious problems.
The big deal about CAD is its harm to health, life, and money. The American Heart Association says CAD is the top killer in the U.S., causing over 1 in 7 deaths.
“Coronary heart disease is the leading cause of death in the United States, responsible for over 1 in 7 deaths.”
American Heart Association
Epidemiology of CAD in the United States
CAD is a big worry in the U.S., hitting millions. The CDC says about 1 in 7 deaths is from CAD. It gets worse with age and hits some groups harder.
Economic and Quality-of-Life Impact
CAD costs a lot, over $200 billion a year in the U.S. It affects work and life quality too. Symptoms like angina and shortness of breath limit what people can do. Finding ways to manage and prevent CAD is key.
- CAD costs a lot to healthcare.
- It makes life hard for those with CAD.
- Prevention and care can lessen CAD’s effects.
We need to tackle CAD seriously. Knowing what it is and how it affects us helps us fight it. This way, we can improve life for those with CAD.
Athscl Heart Disease of Native Coronary Artery: Clinical Perspective
Atherosclerotic heart disease of the native coronary artery is a complex challenge. Healthcare providers must consider many factors. This includes diagnosis, anatomy, and the disease’s progression to provide the best care.
Medical Coding and Documentation Explained
Accurate medical coding and documentation are key for managing atherosclerotic heart disease. The ICD-10 system has specific codes for this condition. Knowing these codes is vital for billing and tracking.
Good documentation also means detailed clinical notes. These notes should outline the patient’s condition, treatment, and follow-up care. This ensures care continuity and helps with communication among healthcare providers.
Anatomical Considerations of Native Coronary Arteries
The native coronary arteries are vital for the heart’s blood supply. Atherosclerotic disease here can cause serious problems. It’s important to understand the coronary arteries’ anatomy for diagnosis and treatment.
The left main coronary artery, left anterior descending artery, and right coronary artery are often affected. Knowing their anatomy and where stenosis can occur is critical for cardiologists and surgeons.
Progressive Nature of Coronary Atherosclerosis
Coronary atherosclerosis is a disease that gets worse over time. It can lead to serious health issues if not treated. The disease causes plaque buildup, leading to stenosis, ischemia, and possibly heart attacks.
It’s important to understand this disease’s progression to develop effective treatments. This includes lifestyle changes, medication, and procedures to manage symptoms and stop disease progression.
The Critical Relationship: How CAD and Atherosclerosis Intersect
It’s key to know how coronary artery disease (CAD) and atherosclerosis are linked for better heart care. We’ll look at how these two conditions are connected. We’ll also focus on what causes CAD and the importance of knowing the difference.
Atherosclerosis as the Primary Cause of CAD
Atherosclerosis is the main reason for CAD. It happens when plaque builds up in artery walls, making them hard and narrow. This can cut off blood to the heart, leading to pain, heart attacks, or other heart problems.
The process of atherosclerosis includes inflammation and the buildup of lipids and macrophages in the arteries. As it gets worse, it can cause CAD by narrowing or blocking the coronary arteries.
Beyond Atherosclerosis: Other Causes of CAD
While atherosclerosis is the main cause of CAD, other things can also play a part. These include:
- Coronary artery spasm
- Spontaneous coronary artery dissection
- Embolic events
- Congenital coronary artery anomalies
These other causes show how complex CAD can be. They highlight the need for a detailed check-up.
Clinical Implications of the Distinction
Telling CAD caused by atherosclerosis apart from other causes is very important. It helps doctors decide the best treatment, from medicine to surgery.
For example, CAD from atherosclerosis might be treated with statins, antiplatelet drugs, and changes in lifestyle. But CAD from other causes might need different treatments, like blood thinners for embolic events or surgery for birth defects.
| Condition | Primary Cause | Typical Treatment Approach |
| CAD with Atherosclerosis | Atherosclerotic plaque buildup | Medical management (statins, antiplatelet therapy), lifestyle modifications |
| CAD without Atherosclerosis | Coronary artery spasm, embolic events, etc. | Condition-specific treatment (e.g., anticoagulation for embolic events) |
Knowing the link between CAD and atherosclerosis helps doctors create better treatment plans. This improves patient outcomes and quality of life.
When Plaque Doesn’t Cause Pain: Atherosclerosis Without Angina
Atherosclerotic disease can quietly progress, without the usual symptom of angina. This makes it hard for doctors, as no pain doesn’t mean no disease. We’ll look into atherosclerosis without angina, its importance, and how hard it is to find.
Understanding “Athscl Heart Disease of Native Coronary Artery W/O Ang Pctrs”
“Athscl heart disease of native coronary artery w/o ang pctrs” means heart disease from plaque buildup in the coronary arteries without chest pain. It’s key to catch this early for treatment.
Not having chest pain doesn’t mean there’s no heart disease. Many people with blocked arteries don’t feel pain, a condition called silent ischemia.
The Phenomenon of Silent Ischemia
Silent ischemia happens when the heart muscle gets less blood without chest pain. This can be due to nerve problems or a higher pain threshold in some.
It’s very important to understand silent ischemia. People with it are at high risk of heart problems like heart attacks and sudden death.
Clinical Significance and Detection Challenges
Finding atherosclerosis without angina is tough. Traditional tests rely on symptoms, which are missing in silent ischemia. We need advanced tests like stress tests and coronary angiography to spot these patients.
The table below shows the main differences between atherosclerosis with and without angina:
| Characteristics | Atherosclerosis with Angina | Atherosclerosis without Angina |
| Symptoms | Chest pain or discomfort | No chest pain or discomfort |
| Detection Method | Often diagnosed based on symptoms | Requires advanced diagnostic techniques |
| Risk of Cardiac Events | High | High, potentially higher due to lack of symptoms |
We need to screen and assess risk for those at high risk of heart disease, even without symptoms. This can help improve outcomes for those with silent ischemia and lessen heart disease’s impact.
Diagnostic Approaches: Identifying and Differentiating the Conditions
To diagnose coronary artery disease (CAD) and atherosclerosis, we use many tools. These tests help us find and tell apart these conditions. This guides us in choosing the right treatments.
Non-Invasive Imaging Techniques
Non-invasive imaging is key in diagnosing CAD and atherosclerosis. Coronary computed tomography angiography (CCTA) and carotid ultrasound let us see the coronary arteries. They do this without needing to go inside the body.
CCTA is a top tool for looking at CAD. It shows us the coronary arteries in detail. This helps us see where the arteries are blocked and how bad it is. This info is key for deciding how to treat CAD.
Functional Assessment Methods
Functional tests help us see how CAD and atherosclerosis affect the heart. Stress testing checks how well the heart works under stress. It finds out if there’s any damage.
Fractional flow reserve (FFR) is another important test. It’s used during angiography to see if a blockage is serious. This helps us decide if we need to open up the artery.
Laboratory Markers and Risk Stratification
Laboratory markers are vital for figuring out the risk and diagnosing. Troponin and lipid profiles tell us about heart damage and risk of atherosclerosis.
| Diagnostic Test | Primary Use | Key Benefits |
| CCTA | Assess coronary artery disease | Non-invasive, detailed imaging |
| Stress Testing | Evaluate cardiac function under stress | Identifies ischemia, guides treatment |
| FFR | Assess functional significance of stenoses | Informs revascularization decisions |
| Lipid Profiles | Assess atherosclerotic risk | Guides risk stratification and treatment |
By using these tests together, we can accurately diagnose CAD and atherosclerosis. This helps us improve patient care by tailoring treatments.
Treatment Strategies: Targeting the Disease Process
Treating CAD and atherosclerosis requires a mix of medical, interventional, and lifestyle strategies. Each patient’s case is different, so we tailor our approach to fit their needs.
Medical Management Approaches
Medical management is key in treating CAD and atherosclerosis. This includes:
- Antiplatelet therapy to prevent clot formation
- Statins and other lipid-lowering medications to manage cholesterol levels
- Beta-blockers to reduce heart rate and blood pressure
- ACE inhibitors or ARBs to manage blood pressure and reduce heart strain
These medications help manage symptoms, slow disease progression, and lower the risk of heart events.
Revascularization Options
For those with severe CAD, revascularization procedures might be needed. These include:
- Percutaneous Coronary Intervention (PCI), also known as angioplasty, with or without stenting
- Coronary Artery Bypass Grafting (CABG), a surgery that bypasses blocked arteries
The choice between PCI and CABG depends on the CAD’s extent and complexity.
Lifestyle Modifications and Prevention
Lifestyle changes are essential in managing CAD and atherosclerosis. We suggest:
- Dietary changes to cut down on saturated fats, cholesterol, and sodium
- Regular physical activity that fits the patient’s health and ability
- Smoking cessation for smokers
- Weight management to keep a healthy weight
These changes help manage the disease and prevent it from getting worse. They also lower the risk of other heart diseases.
By using a complete treatment plan, we can greatly improve outcomes for patients with CAD and atherosclerosis. This plan includes medical management, revascularization when needed, and lifestyle changes.
Conclusion
It’s key to know the difference between coronary artery disease (CAD) and atherosclerosis. These terms are often mixed up, but they mean different things. Atherosclerosis is a process that can cause CAD, but not all atherosclerosis leads to CAD.
Getting the right diagnosis is very important. It helps doctors choose the best treatment, like medicine, surgery, or lifestyle changes. At Liv Hospital, we focus on accurate diagnoses and personalized treatment plans for our patients from around the world.
Healthcare providers need to understand the difference between CAD and atherosclerosis. This knowledge helps them manage atherosclerotic heart disease better. Good management of CAD involves treating the root causes and risk factors.
FAQ:
What is the difference between coronary artery disease and atherosclerosis of the native coronary artery?
Coronary artery disease (CAD) is when the coronary arteries narrow or block due to atherosclerosis. Atherosclerosis of the native coronary artery is when the native coronary arteries build up with plaque.
Is coronary artery disease the same as atherosclerosis?
No, they are related but not the same. Atherosclerosis is a condition that can affect many arteries, including the coronary arteries, leading to CAD.
What is atherosclerotic heart disease of native coronary artery without angina pectoris?
This is when the native coronary arteries are affected by atherosclerosis but the patient doesn’t have angina symptoms. This is often due to silent ischemia.
How is coronary artery disease diagnosed?
It’s diagnosed with non-invasive imaging like CT angiography, stress testing, and lab tests for risk.
What are the treatment options for managing CAD and atherosclerosis?
Treatments include medical management, angioplasty, CABG, and lifestyle changes. Each plan is tailored to the patient’s needs.
Can atherosclerosis be managed without surgery?
Yes, it can be managed with medications and lifestyle changes. Sometimes, surgery like angioplasty or CABG is needed.
What is the role of laboratory markers in diagnosing CAD and atherosclerosis?
Lab markers help identify high-risk patients and track disease progression. They are key in diagnosing CAD and atherosclerosis.
How does atherosclerosis affect the heart?
It can narrow or block coronary arteries, reducing blood flow. This can cause angina, heart attacks, or other heart problems.
What is silent ischemia, and how is it detected?
Silent ischemia is when the heart muscle doesn’t get enough oxygen, often without symptoms. It’s hard to detect and may need advanced tests like stress testing or imaging.
Why is precise medical terminology important in diagnosing and managing CAD and atherosclerosis?
Accurate terms help avoid confusion and ensure proper diagnosis and care. They help healthcare providers and patients make informed treatment choices.
References:
Libby, P., Buring, J. E., Badimon, L., Hansson, G. K., Deanfield, J., Bittencourt, M. S., Tokgözoğlu, L., & Lewis, E. F. (2019). Atherosclerosis. Nature Reviews Disease Primers, 5(1), 56. https://pubmed.ncbi.nlm.nih.gov/31420554/