Last Updated on November 26, 2025 by Bilal Hasdemir

Having a stent placed to treat coronary artery disease is a significant step, and many patients wonder how long after a stent can you fly safely. At Liv Hospital, we prioritize your safety and comfort throughout recovery, following the latest care standards.
Coronary angioplasty and stenting have improved treatment outcomes, but careful adherence to recovery guidelines is essential. Knowing how long after a stent can you fly helps patients plan travel while avoiding unnecessary stress or complications.
Our team guides you on when it’s safe to resume air or road travel, ensuring you follow a timeline that supports a smooth, safe recovery. With the right advice, you can confidently return to daily life and travel after a stent procedure.
Key Takeaways
- Understand the recovery process after stent placement.
- Learn when it’s safe to resume air travel.
- Discover guidelines for driving after a stent procedure.
- Find out how to maintain positive treatment outcomes.
- Explore the importance of following international care standards.
Understanding Coronary Stent Procedures
Learning about coronary stent procedures can ease worries and help patients make better choices. These procedures are key to treating coronary artery disease. This disease narrows or blocks arteries due to plaque buildup.
What Is Coronary Angioplasty and Stenting?
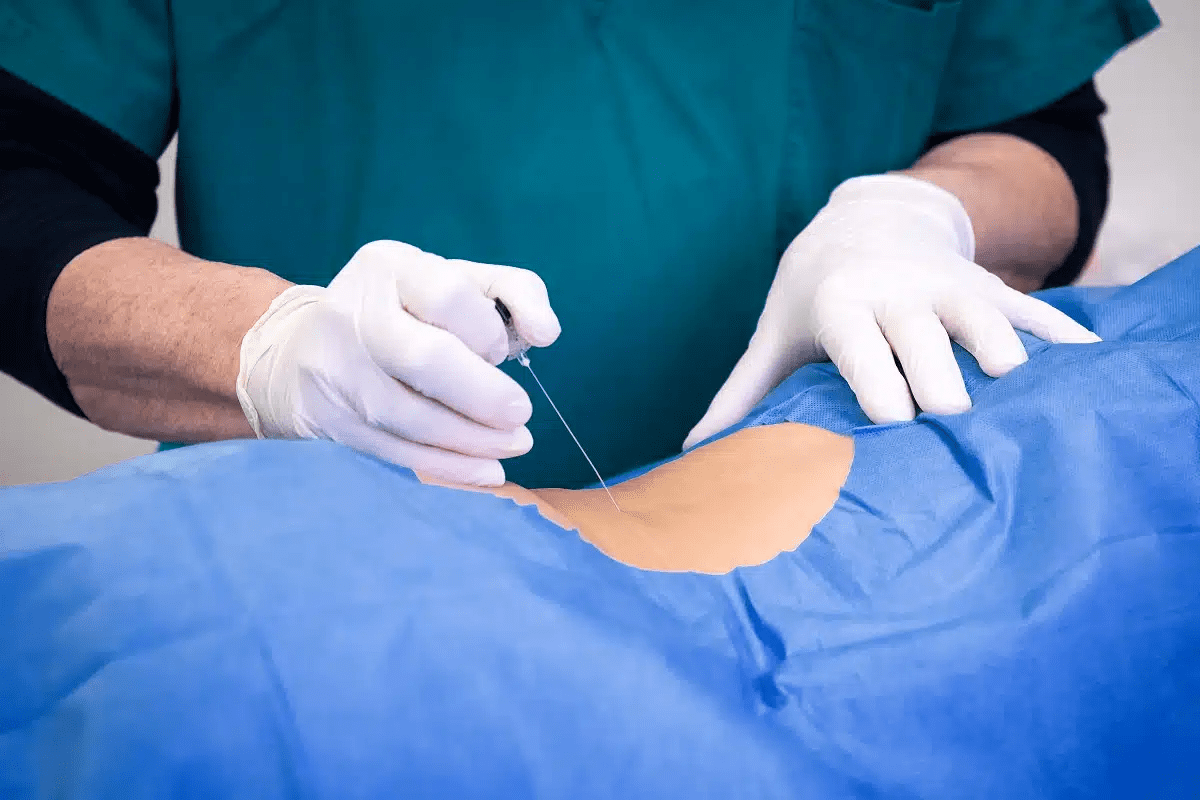
Coronary angioplasty and stenting help restore blood flow to the heart. Angioplasty uses a balloon to widen narrowed or blocked arteries. Stenting places a mesh-like device (stent) to keep the artery open. These steps are often done together to keep the artery open and working well.
The process starts with a small incision in the wrist or groin. A thin, flexible tube (catheter) is guided to the blocked area. Then, a balloon is inflated to widen the artery. After that, a stent is placed to keep the artery open, improving blood flow to the heart muscle.
PCI vs. Angioplasty: Understanding the Terminology
Many get confused by PCI (Percutaneous Coronary Intervention), angioplasty, and stenting. While they’re often used together, they mean different things. PCI is a wide term for treatments like angioplasty and stenting for coronary artery disease. Angioplasty is the use of a balloon to widen the artery. Stenting is the placement of a stent.
Often, PCI means both angioplasty and stenting are used. The term “PCI” is used because it covers the whole strategy of using minimally invasive methods to restore blood flow in the coronary arteries.
Types of Stents and Their Purposes
There are many types of stents, each with its own purpose. Bare-metal stents are the traditional type, made from metal mesh. Drug-eluting stents are coated with medication to prevent the artery from re-narrowing. Bioresorbable stents dissolve over time, potentially reducing long-term complications.
The type of stent chosen depends on the patient’s health, the blockage’s location and severity, and past stenting experiences. Knowing about the different stents and their uses helps patients understand their options and make informed decisions.
The Recovery Process After Stent Placement

The recovery after stent placement is very important. You need to pay close attention and follow the doctor’s advice. Knowing what to expect can make your recovery better.
Immediate Post-Procedure Care
Right after the stent is placed, you’ll stay in a recovery area for a few hours. The medical team will watch your vital signs and the area where the procedure was done. It’s key to listen to the healthcare team about rest, medicine, and follow-up visits for a smooth recovery.
Most people go home the same day or the next day. It’s a good idea to have someone with you when you get home because you might feel sleepy from the sedation.
Common Side Effects and Symptoms
After the stent is placed, some people might feel certain side effects. These can include:
- Bruising or discomfort at the catheter insertion site
- Fatigue or feeling tired
- Mild chest discomfort
- Allergic reactions to the contrast dye used during the procedure
These symptoms are usually mild and short-lived. But it’s important to tell your doctor if they get worse or last too long. Watching how your body reacts and talking to your doctor can help avoid problems.
| Symptom | Typical Duration | Action to Take |
| Bruising at the insertion site | A few days to a week | Apply ice, monitor for infection |
| Fatigue | Several days to a few weeks | Rest, gradually increase activity |
| Mild chest discomfort | A few days | Contact your doctor if persistent |
Fatigue After Stent Placement: What to Expect
Fatigue is common after stent placement. How much and for how long you feel tired can vary. It depends on the procedure’s complexity, your health, and whether the stent was placed after a heart attack.
“Patients often report feeling tired or fatigued after stent placement. This is usually temporary and improves as you recover.”
— Medical Expert in Cardiology
To deal with fatigue, try to:
- Rest when needed
- Slowly start moving more as your doctor suggests
- Eat a balanced diet full of nutrients
Knowing what to expect during recovery can help you get through it better. It’s vital to keep in touch with your healthcare team and follow their advice for the best results.
General Activity Guidelines Following Stent Procedures
After a stent procedure, patients often wonder when they can go back to normal. We know this time can be tough. Clear guidelines help make recovery smoother.
Resuming Daily Activities
Most patients can start doing daily things a few days after the procedure. But it’s key to follow your doctor’s advice on how active you can be. Start with light activities like walking or doing light chores. Stay away from heavy lifting, bending, or hard work for a bit, or as your doctor says.
Watch how your body reacts to more activity. If you feel chest pain, shortness of breath, or dizziness, stop right away and talk to your doctor.
Exercise Recommendations
Exercise is key to getting better. Begin with easy exercises like short walks. Then, slowly add more time and effort as your doctor suggests. Avoid hard exercise or heavy work for a while.
Regular exercise boosts heart health and overall feeling. But don’t push too hard. If you’re worried about exercising after a stent, talk to your cardiologist.
When to Call Your Doctor
After a stent, knowing when to call for help is important. Call your doctor for chest pain, shortness of breath, or severe bleeding. Also, watch for signs of infection at the catheter site,like redness, swelling, or fever. Get medical help if you see these.
Your doctor will tell you what to watch for and when to get help. Always be cautious and ask your doctor if you’re unsure about symptoms.
Driving After a Stent: Timeline and Safety Considerations
Many people ask when it’s okay to drive again after getting a stent. The answer depends on your health, the procedure details, and the stent type.
How Soon Can You Drive After a Stent?
Doctors usually tell patients not to drive for 24 to 48 hours after getting a stent. This helps with recovery and lowers the chance of problems.
It’s key to listen to your doctor’s advice. They can give you specific guidance based on your situation and procedure details.
Factors That May Delay Return to Driving
Several things can affect when you can drive again after a stent. These include:
- Complications during or after the procedure
- Side effects from medications, such as drowsiness
- Underlying health conditions that affect driving ability
Talking to your doctor about these factors is important. They can tell you when it’s safe to drive.
Special Considerations for Commercial Drivers
Commercial drivers face stricter rules for returning to work and driving. The rules can vary by area, but often, they need to take more time off than others.
| Driver Type | Recommended Time Off Driving |
| Non-Commercial Drivers | 24-48 hours |
| Commercial Drivers | Typically longer than 48 hours; check local regulations |
Commercial drivers should talk to their doctor and check the rules before driving again.
Passenger Travel by Car After Stent Placement
Many patients wonder when they can safely travel by car as a passenger after getting a stent. As a passenger, you can usually go on short car trips soon after your stent procedure. But it’s important to follow certain guidelines to stay safe and comfortable while traveling.
Short Car Trips as a Passenger
For short car trips, you can usually start traveling a few days after your procedure. It’s key to:
- Follow your doctor’s specific instructions regarding travel.
- Wear comfortable clothing and consider wearing compression stockings if recommended by your doctor.
- Take regular breaks to stretch your legs if the trip is longer than 30 minutes.
Recommendations for Longer Road Trips
For longer road trips, we suggest waiting at least a week after your stent procedure. When you do travel, keep these tips in mind:
- Plan your trip to include regular breaks (every 1-2 hours) to stretch and move around.
- Stay hydrated and avoid heavy meals during travel.
- Keep your medications and medical records easily accessible.
Preventing DVT During Car Travel
One risk of prolonged car travel is Deep Vein Thrombosis (DVT). To prevent DVT:
- Stay hydrated by drinking plenty of water.
- Take regular breaks to walk around and stretch your legs.
- Consider wearing compression stockings if you’re at higher risk of DVT.
By following these guidelines, you can reduce the risks of car travel after stent placement. This ensures a safe and comfortable journey for you.
How Long After a Stent Can You Fly?
Many patients wonder when it’s safe to fly after getting a stent. Flying after a stent needs careful thought to keep you safe and comfortable.
General Guidelines for Air Travel After Routine Stent Placement
For routine stent placements, wait 24 to 48 hours before flying. This helps your body heal and lowers the risk of problems.
Pre-flight preparations are key. Carry all your meds and wear loose, comfy clothes to avoid blood clots.
Flying After Emergency Stent Procedures
Emergency stent procedures mean waiting longer to fly, usually 7-10 days or more. This depends on your health and the procedure details.
Your doctor’s advice is vital. Emergency stents often mean serious heart issues that need close watch.
Getting Medical Clearance Before Flying
Always get clearance from your cardiologist before flying, no matter the stent type. They can check your health and give tailored advice.
| Procedure Type | Recommended Waiting Period | Medical Clearance |
| Routine Stent Placement | 24-48 hours | Recommended |
| Emergency Stent Placement | 7-10 days or more | Highly Recommended |
Knowing these guidelines and talking to your doctor helps you decide when to fly after a stent.
Air Travel Risks and Precautions for Stent Patients
It’s important for patients with stents to know about flying risks. Air travel is mostly safe, but there are dangers like deep vein thrombosis (DVT) and how cabin pressure affects the heart.
Understanding DVT Risk During Flights
DVT is a blood clot in the deep veins, often in the legs. Long flights increase DVT risk because of sitting for too long. Patients with stents need to be extra careful because they’re already at risk.
A study in the Journal of Thrombosis and Haemostasis showed long flights raise DVT risk. It stressed the need for prevention.
“The risk of venous thromboembolism is increased in passengers on long-distance flights, especially those over 4 hours.”
We suggest patients get up and move around the cabin often. Doing simple exercises can help blood flow.
| Prevention Strategies | Description |
| Regular Movement | Walk up and down the aisle every 1-2 hours |
| Exercises | Do leg stretches and ankle rotations while sitting |
| Compression Stockings | Wear stockings to help blood flow |
Cabin Pressure and Cardiovascular Considerations
Changes in cabin pressure can affect the heart. Lower air pressure means less oxygen in the blood, which can strain the heart.
Patients with stents should talk to their cardiologist before flying. This is important if they worry about their heart health.
Safety Measures During Air Travel
There are safety steps patients can take during flights:
- Drink lots of water to stay hydrated
- Avoid crossing legs or ankles to keep blood flowing
- Wear loose, comfy clothes
Knowing these risks and taking precautions can help patients with stents have a safer flight.
Special Considerations: Stent Following Heart Attack
Getting a stent after a heart attack means you need special care. It’s important to follow a safe and effective recovery plan.
Recovery Timeline After Heart Attack and Stent
The recovery after a heart attack and stent is different from a regular stent. It has several phases:
- Immediate Recovery (0-3 days): Rest and do less activity right after.
- Short-term Recovery (3-14 days): Start doing more, but slowly. Most can do light things.
- Long-term Recovery (2-6 weeks): Keep getting more active. Cardiac rehab is a good idea if your doctor says so.
Always listen to your doctor about what activities you can do and when to take your meds.
How Soon Can You Drive After Heart Attack and Stent?
Driving after a heart attack and stent needs careful thought. How soon you can drive depends on your health and local rules.
Doctors often say to wait:
- At least 1 week (7 days): But it can change.
- Until your doctor’s approval: Your cardiologist must say it’s okay to drive, even if you’ve had big heart damage.
Drivers who make money from driving might have to wait longer and follow special rules.
How Soon Can You Fly After Heart Attack and Stents?
Thinking about flying after a heart attack and stent is important. The usual advice is to wait:
- At least 2-4 weeks: This helps your body heal and lowers flight risks.
- Until medically cleared: Always check with your doctor before flying, as they can say if it’s safe.
- Carrying your meds and medical records
- Avoiding sitting too long on flights
- Drinking water and not eating too much before and during travel
Knowing these tips and listening to your doctor helps you get back to normal after a heart attack and stent.
Discussing Travel Plans With Your Cardiologist
Before you plan any trips after getting a stent, talk to your cardiologist. They can tell you about the dangers of travel and how to avoid them. They know your health well and can give you advice that fits you.
Important Questions to Ask Before Traveling
When you talk to your cardiologist about traveling, ask these questions:
- Are there any specific risks associated with my travel plans?
- How should I manage my medications while traveling?
- What are the signs and symptoms I should watch out for during travel?
- Are there any precautions I can take to minimize risks during travel?
These questions help you understand how to stay safe on your trip. A doctor says, “It’s always better to be cautious when it comes to your health, specially after a big procedure like stent placement.”
Individualized Risk Assessment
Your cardiologist will check if your travel plans are safe. They look at many things, like:
- The type of stent used and its implications
- Your overall health and any comorbid conditions
- The nature of your travel plans (e.g., mode of transport, duration, destination)
They use these factors to give you advice that fits you. A cardiologist says, “The key to safe travel after stent placement is understanding the individual’s health status and planning according.”
When to Postpone Travel Plans
There are times when you should wait to travel after a stent. For example:
- If you have complications or symptoms like chest pain, shortness of breath, or dizziness
- If your cardiologist says it’s not safe for you to travel
- If you’re close to your stent placement procedure
In these cases, your health and safety come first. A medical guideline says, “Patient safety should always be the top priority when considering travel after a medical procedure.”
Talking to your cardiologist and following their advice can help you stay safe on your trip.
Practical Tips for Traveling After Stent Placement
Traveling after a stent placement needs careful planning. You must consider several key factors for your safety and comfort. This ensures a smooth trip.
Packing Medications and Medical Supplies
It’s vital to pack your medications and medical supplies carefully. Carry all prescribed medications and any needed documents or ID.
- Keep medications in their original packaging to avoid any confusion.
- Pack a small supply of medications in your carry-on luggage in case your checked luggage is delayed.
- Bring a list of your medications, including dosages and the name of the prescribing physician.
Finding Medical Care at Your Destination
Research medical facilities and healthcare providers at your destination before you go. Find hospitals or clinics near your stay that can help if needed.
| Destination | Nearest Hospital/Clinic | Contact Information |
| New York | NewYork-Presbyterian Hospital | (212) 746-3740 |
| Los Angeles | Cedars-Sinai Medical Center | (310) 423-3277 |
| Chicago | Northwestern Memorial Hospital | (312) 926-5188 |
Travel Insurance Considerations for Cardiac Patients
Travel insurance is key for cardiac patients after a stent placement. Look for policies that cover medical emergencies, including heart-related issues.
Key considerations when selecting travel insurance:
- Coverage for pre-existing conditions
- Emergency medical evacuation coverage
- Coverage for trip cancellations or interruptions due to medical reasons
Conclusion: Ensuring Safe Travel After Stent Procedures
Traveling after a stent procedure needs careful planning. We’ve given you guidelines for driving and flying, talked about risks, and shared tips for safe travel. By knowing the recovery process and taking precautions, patients can have a safe and fun trip.
Before traveling after a stent, talk to your cardiologist. They can give you advice based on your stent type, health, and why you got the stent. Usually, you can drive a few days to a week after the procedure. Flying might be safe a week or more later.
To travel safely after a stent, know the risks like DVT on flights. Follow the guidelines and advice we’ve given. We’re here to help you recover and live a healthy, active life.
FAQ
How soon can I drive after a stent procedure?
You can usually drive a few days after getting a stent. But, it depends on your health and the procedure. Always ask your cardiologist for advice.
How long after a stent can I fly?
For most stent procedures, flying is okay a few days to a week later. Emergency stents or heart attacks might need longer waiting. Always check with your cardiologist before flying.
What is the difference between PCI and angioplasty?
PCI is a term for many procedures, like angioplasty and stenting, to open blocked arteries. Angioplasty uses a balloon to widen the artery. Then, a stent is used to keep it open.
Can I fly with a stent in my heart?
Yes, flying with a stent is possible. But, follow your cardiologist’s advice and wait the recommended time. Also, take precautions to avoid DVT during flight.
How soon can I drive after a heart attack and stent placement?
Driving after a heart attack and stent varies. You might wait a few days to a week. Your cardiologist will give you specific advice based on your health.
What are the risks associated with air travel after stent placement?
Air travel risks include DVT from sitting too long and cabin pressure effects. Stay hydrated, move often, and wear compression stockings to reduce risks.
How long after stent placement can I resume normal activities?
You can usually go back to normal activities a few days to a week after a stent. But, follow your cardiologist’s instructions and increase activity slowly for a smooth recovery.
Are there special considerations for commercial drivers after stent placement?
Yes, commercial drivers might need to wait longer due to their job’s demands. They must also follow specific regulations. Always talk to your cardiologist and check the rules.
What should I discuss with my cardiologist before traveling after stent placement?
Talk to your cardiologist about your travel plans, including how you’ll travel and for how long. They can give you personalized advice, assess risks, and suggest precautions or medical clearance.
References
- Rassaf, T., Steiner, S., & Kelm, M. (2013). Postoperative care and follow-up after coronary stenting. Dtsch Arztebl International, 110 (5), 72-82. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3576602/
- Shroff, A., Gilchrist, I., Caputo, R., Bertrand, M., & Pancholy, S. (2016). Same-day discharge after percutaneous coronary intervention. JAMA Cardiology, 1 (3), e160141. https://jamanetwork.com/journals/jamacardiology/fullarticle/2506675
- Li, J., et al. (2024). Analysis of influential factors of stent-related adverse outcomes: A 10-year single-centre study. Scientific Reports, 14, 79362. https://www.nature.com/articles/s41598-024-79362-7