Atrial fibrillation (AFib) is a complex heart condition affecting millions worldwide. While pacemakers are not a cure for AFib, they can help manage its symptoms. This is true for patients with heart rate issues.
At Liv Hospital, we combine international expertise with patient-centered care. We ensure you get a treatment plan based on the latest evidence. For patients with AFib and slow heart rates or other heart conduction disorders, a pacemaker might be helpful.
We understand that managing AFib requires a complete approach. Lifestyle changes are often suggested to manage AFib before a pacemaker is considered. But for the right patients, pacemakers can bring stability and better quality of life.
Learn does a pacemaker help AFib, how it supports rhythm control, and which patients benefit most from the device.
Key Takeaways
- Pacemakers are not a cure for AFib but can help manage its symptoms.
- Patients with AFib involving slow heart rate or heart conduction disorders may benefit from a pacemaker.
- Lifestyle changes are often recommended before considering a pacemaker.
- A tailored treatment plan is essential for effective AFib management.
- Pacemakers can offer stability and improved quality of life for the right patients.
Understanding Atrial Fibrillation and Its Challenges
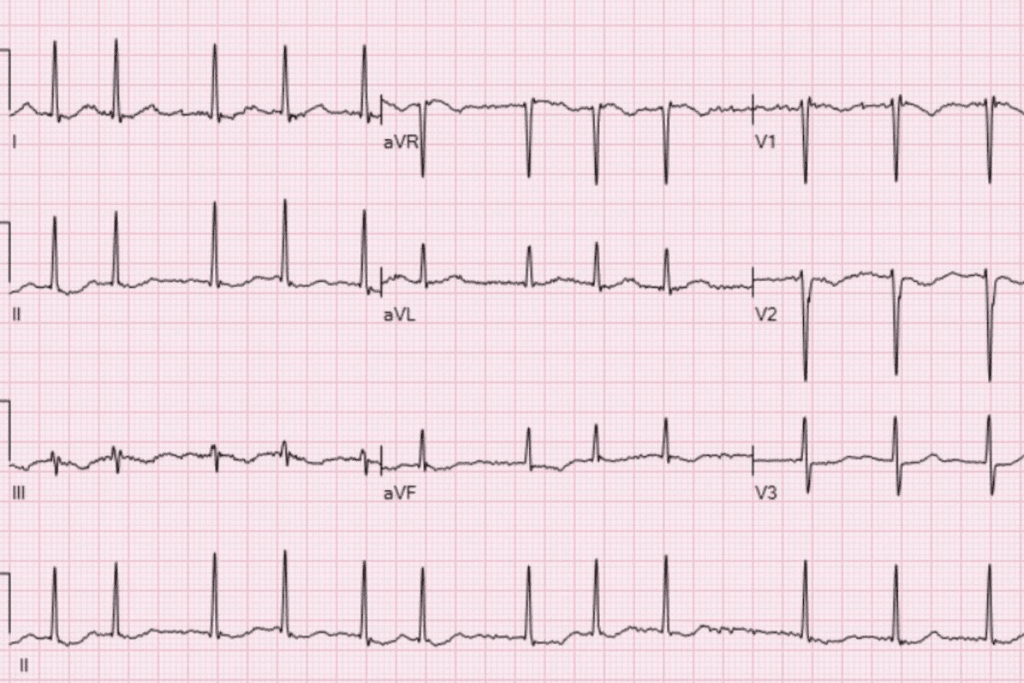
It’s important for both patients and doctors to understand atrial fibrillation (AFib). This heart condition makes managing and treating it tough. AFib is when the heart’s upper chambers beat in a chaotic, irregular way.
What Happens in the Heart During AFib
AFib disrupts the heart’s electrical signals. This leads to irregular heartbeats. The heart might beat too fast, too slow, or irregularly. Symptoms include palpitations, shortness of breath, and fatigue.
The chaotic atria beating can also cause blood clots. This increases the risk of stroke.
Common Symptoms and Complications
AFib symptoms vary from person to person. Common ones include:
- Palpitations or irregular heartbeat
- Shortness of breath
- Fatigue or weakness
- Dizziness or lightheadedness
- Chest pain or discomfort
AFib can also lead to heart failure, stroke, and other heart problems if not managed well.
Standard Treatment Approaches
Treatment for AFib includes lifestyle changes, medications, and medical procedures. The goals are to control heart rate, restore rhythm, and prevent blood clots and stroke.
| Treatment Approach | Description |
| Medications | To control heart rate or rhythm, and to prevent blood clots |
| Cardioversion | A procedure to restore normal heart rhythm using electrical shocks |
| Catheter Ablation | A minimally invasive procedure to destroy abnormal electrical pathways |
| Pacemaker Therapy | Using a pacemaker to help regulate heart rhythm |
Knowing about AFib is key to understanding how pacemakers can help. Pacemakers can control heart rate and improve function. They are a vital part of treatment for some AFib patients.
What Is a Pacemaker and How Does It Work?
heart rhythms. They are small, battery-powered, and prevent the heart from beating too slowly. Knowing how they work is key to understanding their role in managing atrial fibrillation (AFib).
Components and Function of Modern Pacemakers
A pacemaker has two main parts: a pulse generator and leads. The pulse generator is a small metal box with the battery and circuitry. The leads are insulated wires that connect to the heart.
Together, they send electrical signals to the heart. This ensures it beats at the right rhythm.
Key Components:
- Pulse Generator: Contains the battery and electronic circuitry.
- Leads: Insulated wires that connect to the heart.
- Electrodes: Tips of the leads that deliver electrical signals.
Different Types of Pacemakers
There are many types of pacemakers, each for different heart conditions. The main types include:
| Type | Description |
| Single-Chamber Pacemakers | Use one lead to pace one chamber of the heart. |
| Dual-Chamber Pacemakers | Use two leads to pace both the atrium and ventricle, providing a more natural heartbeat. |
| Biventricular Pacemakers | Used in cardiac resynchronization therapy (CRT), these pacemakers help coordinate the beating of the left and right ventricles. |
How Pacemakers Regulate Heart Rhythm
Pacemakers work by sending electrical impulses to the heart. When they detect a slow heart rate, they send a signal. This makes the heart beat at a consistent rate.
This helps patients with heart rhythm disorders feel better and live better lives.
Understanding pacemakers helps us see their importance in managing atrial fibrillation and other heart issues.
Does a Pacemaker Help AFib? The Truth About Its Role
Many think pacemakers can fix AFib, but it’s not that simple. Atrial Fibrillation (AFib) is a serious heart issue affecting millions. The role of pacemakers in treating it is often misunderstood.
Clarifying Common Misconceptions
Some believe pacemakers can cure AFib or control its symptoms. But, pacemakers are not a cure for AFib. They help manage some aspects of the condition, mainly when AFib is linked with other heart rhythm problems.
One big mistake is thinking pacemakers can directly fix AFib. In truth, they ensure the heart beats at a good rate. This is important when AFib causes a slow heartbeat or long pauses between beats.
Supportive vs. Curative Functions
Pacemakers are not meant to cure AFib; they support it. Their main job is to keep the heart rate right, preventing it from beating too slow. Sometimes, they’re used with other treatments like ablation to better manage AFib.
For example, in patients with AFib and slow heart rate, a pacemaker can keep the heart rate right. This improves symptoms and life quality. But, the pacemaker doesn’t treat the AFib itself; it just helps the heart’s rhythm.
Measuring Success in AFib Management with Pacemakers
Success with pacemakers for AFib is seen in better symptoms, life quality, and heart function. For those with AFib and slow heart rate, a working pacemaker means fewer symptoms. This includes less dizziness, fatigue, and shortness of breath.
| Outcome Measure | Description | Expected Improvement with Pacemaker |
| Symptom Reduction | Decrease in symptoms such as dizziness, fatigue, and shortness of breath | Significant reduction |
| Quality of Life | Improvement in overall well-being and ability to perform daily activities | Noticeable improvement |
| Heart Rate Stability | Maintenance of an appropriate heart rate during AFib episodes | Improved stability |
Clinical Evidence and Research Findings
Many studies have looked into pacemakers for AFib. The results are mixed, but most agree they help certain patients. This includes those with slow heart rate or pauses in rhythm.
Research keeps getting better, looking into new ways to use pacemakers with other treatments. As we learn more about AFib and pacemakers, we’ll see better ways to manage this complex condition.
When Is a Pacemaker Recommended for AFib Patients?
AFib patients might need a pacemaker in certain situations. We suggest pacemakers for those with heart rhythm issues that pacing can fix.
AFib with Bradycardia (Slow Heart Rate)
Bradycardia, or a slow heart rate, is a common reason for pacemakers in AFib patients. This slow rate can cause fatigue, dizziness, and shortness of breath. A pacemaker helps keep the heart rate steady, improving heart function.
Significant Pauses in Heart Rhythm
AFib patients might experience sinus pauses or sinus arrest. These pauses can lead to dizziness, fainting, or heart failure. A pacemaker prevents these pauses, keeping the heart rhythm stable.
Medication-Induced Bradycardia
Some AFib medications, like beta-blockers or calcium channel blockers, can cause bradycardia. If this bradycardia is severe and causes symptoms, a pacemaker is needed. It ensures a proper heart rate while managing AFib with medication.
After Specific Ablation Procedures
After certain ablation procedures, like AV node ablation, a pacemaker might be recommended. This procedure stops rapid heart rates in AFib. A pacemaker is then used to maintain a stable heart rhythm.
Understanding these scenarios helps us decide when a pacemaker is right for AFib patients. Our aim is to provide care that meets each patient’s unique needs.
The “Pace and Ablate” Strategy Explained
The “pace and ablate” strategy is a key treatment for Atrial Fibrillation (AFib). It uses a pacemaker and AV node ablation to manage AFib symptoms well.
What Is AV Node Ablation?
AV node ablation uses heat to destroy the AV node. This area is between the heart’s upper and lower chambers. It sends electrical signals that can cause irregular heart rhythms in AFib patients.
By ablating the AV node, doctors block faulty signals. This helps prevent AFib symptoms.
How Pacemakers Complement This Procedure
After AV node ablation, a pacemaker is implanted. It regulates the heartbeat. This ensures the heart beats at the right rhythm, making up for the AV node’s loss.
This combination is why the “pace and ablate” strategy works well.
Key benefits of using a pacemaker with AV node ablation include:
- Regulation of heart rhythm
- Improvement in symptoms related to AFib
- Enhanced quality of life for patients
Ideal Candidates for This Approach
The “pace and ablate” strategy is for AFib patients who haven’t responded to other treatments. It’s for those with symptomatic AFib who face discomfort or complications.
Expected Outcomes and Success Rates
Studies show the “pace and ablate” strategy improves symptoms and quality of life for AFib patients. Success rates vary, but many see a decrease in AFib symptoms and better heart function.
It’s important for patients to talk to their healthcare provider. They should discuss their situation and what to expect from the “pace and ablate” strategy.
Special Pacemaker Technologies for AFib Patients
For those with AFib, new pacemaker technologies bring hope. These advancements help manage AFib better. They improve life quality and treatment results.
Rate-Responsive Pacemakers
Rate-responsive pacemakers adjust their rate with your activity. They make sure your heart rate matches your body’s needs, whether you’re resting or moving.
Key Benefits:
- Improved exercise tolerance
- Better adaptation to physical demands
- Enhanced overall heart function
Cardiac Resynchronization Therapy (CRT)
CRT makes the heart’s chambers beat in sync. This boosts heart efficiency and lessens heart failure symptoms, common in AFib.
How CRT Works:
- CRT devices send electrical impulses to both ventricles.
- This helps the ventricles beat in a more synchronized manner.
- Improved synchronization enhances the heart’s pumping efficiency.
Leadless Pacemakers
Leadless pacemakers are a big leap forward. They’re a less invasive option than traditional pacemakers, without the need for leads.
Advantages:
- Reduced risk of lead-related complications
- Minimally invasive implantation procedure
- Potential for fewer post-procedure complications
MRI-Compatible Pacemakers
MRI-compatible pacemakers let patients safely get MRI scans. This is key for diagnosing many conditions. It’s vital for those needing regular imaging.
Benefits of MRI Compatibility:
- Safe access to MRI scans for diagnostic purposes
- Reduced risk associated with MRI scans in patients with pacemakers
- Enhanced patient safety and diagnostic flexibility
In conclusion, these special pacemaker technologies offer AFib patients advanced treatment options. They’re tailored to their needs, improving condition management and life quality.
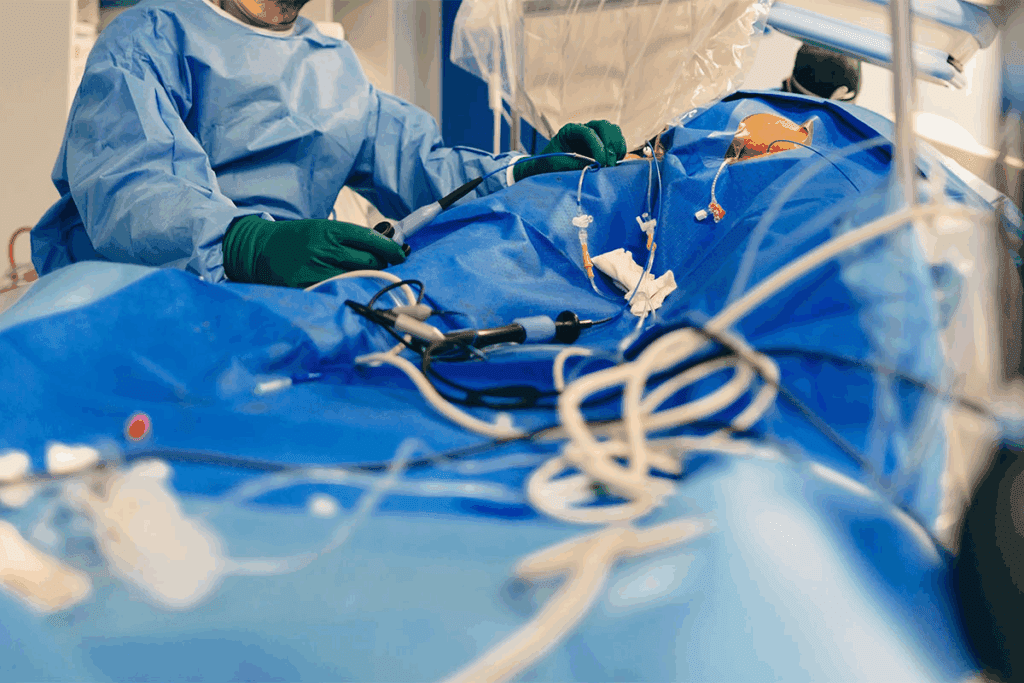
The Pacemaker Implantation Procedure for AFib Patients
AFib patients often have many questions about the pacemaker implantation process. We know this can be scary, and it’s key to know what to expect.
Pre-Procedure Preparation
Before the procedure, we make sure you’re ready. We do tests to check your heart and health. Our team also looks at your medical history and current medications to lower risks.
What Happens During Implantation
During the procedure, we numb the area with local anesthesia. A small cut is made, and the pacemaker leads are guided through a vein into your heart. The pacemaker is then connected and set up for your needs. This usually takes a few hours.
Recovery and Initial Adjustments
After the procedure, we watch you closely for any issues. You might feel some pain or bruising, but it should go away in a few days. We also adjust the pacemaker settings as needed to make sure it works right for you.
Typical Hospital Stay and Follow-up
Most patients stay in the hospital overnight for observation. Our team checks the pacemaker’s function and makes sure you’re doing well. After you go home, we schedule follow-up visits to check the pacemaker and make any needed changes. We also give you tips on caring for the implant site and what to expect during recovery.
Living with Both AFib and a Pacemaker
Having a pacemaker can change how you manage AFib. It brings both good points and challenges. Knowing how to care for both conditions is key.
Monitoring and Follow-Up Care
It’s important to see your doctor often if you have AFib and a pacemaker. We check how the device is working and make any needed changes. We also look for any problems.
- Regular check-ups with your cardiologist
- Device interrogation to assess pacemaker function
- Adjustments to pacing settings to optimize heart rhythm
These visits help us keep an eye on your heart health. We also manage any symptoms of AFib. This way, we make sure both the pacemaker and AFib are well-managed.
Activity Restrictions and Lifestyle Considerations
Pacemakers are tough, but some activities need caution. We tell patients to:
- Avoid strong magnetic fields, such as those from MRI machines (unless the pacemaker is MRI-compatible)
- Be cautious with certain household appliances and tools
- Inform their doctor about any new medical procedures or treatments
Most activities, like exercise and travel, are okay. But, it’s good to talk to your doctor about any plans.
Managing AFib Episodes with a Pacemaker
Even with a pacemaker, AFib episodes can happen. We teach patients to recognize these episodes and what to do. This includes:
- Monitoring pulse and rhythm
- Using prescribed medications to control heart rate or convert AFib to a normal sinus rhythm
- Seeking medical attention if episodes are prolonged or severe
By being proactive, patients can manage their AFib better. This reduces the risk of complications.
Device Longevity and Replacement
Pacemakers last several years, but they need to be replaced eventually. How long a pacemaker lasts depends on many things. We keep an eye on the device to plan for replacement when needed.
| Device Type | Average Lifespan | Factors Affecting Longevity |
| Single-Chamber Pacemaker | 8-12 years | Pacing frequency, battery capacity |
| Dual-Chamber Pacemaker | 6-10 years | Pacing frequency, battery capacity, complexity of device |
| CRT Pacemaker | 5-8 years | Pacing frequency, battery capacity, resynchronization therapy requirements |
Knowing these details helps patients plan for the long-term care of their condition and device.
Alternatives to Pacemakers for AFib Management
Managing AFib isn’t just about pacemakers. There are many other treatments that can help. These options depend on the patient’s needs and how severe their AFib is.
Medication-Based Approaches
Medicines are key in treating AFib. Anti-arrhythmic drugs help control heart rhythm. Rate-control medications manage heart rate. We often start with these to ease symptoms and improve life quality.
Choosing the right medicine is important. It depends on the patient’s health, other conditions, and their AFib type. For example, some heart conditions might need specific medicines.
Catheter Ablation Techniques
Catheter ablation is a popular treatment for AFib. It uses catheters to destroy bad electrical pathways in the heart.
This method is great for those who don’t do well with medicines or want a more lasting solution. How well it works depends on the patient’s health and AFib type.
Surgical Options
Surgery might be needed for some AFib cases. The Maze procedure is one example. It creates scar tissue to guide heart impulses.
We usually save surgery for patients having other heart surgeries or with severe symptoms. Each patient’s suitability is carefully checked.
Emerging Therapies and Clinical Trials
New treatments and trials are always coming up in AFib management. These include new medicines, advanced catheter ablation, and more.
Joining clinical trials can give patients early access to new treatments. We suggest talking to your doctor about these options to see if you qualify.
Conclusion: The Future of AFib Management with Pacemakers
Our understanding of atrial fibrillation (AFib) and pacemaker technology is growing. This makes managing AFib more effective. Pacemakers are key in treating AFib, working well with other therapies.
New pacemaker designs, like rate-responsive and leadless pacemakers, are improving lives. These advancements, along with other treatments, are leading to better patient outcomes. We can look forward to even more progress in managing AFib.
Pacemakers are being used with other treatments like catheter ablation and medications. This approach provides personalized care for each patient. As research keeps advancing, pacemakers will remain essential in treating AFib.
FAQ
Does a pacemaker cure atrial fibrillation?
No, a pacemaker doesn’t cure atrial fibrillation (AFib). But it can help manage its symptoms. This is true for patients with heart rate issues.
Can a pacemaker help with AFib?
Yes, pacemakers can help manage AFib. They are good for patients with slow heart rates or pauses in rhythm. They also help with medication-induced bradycardia.
What is the “pace and ablate” strategy for AFib management?
The “pace and ablate” strategy involves two steps. First, ablating the AV node to block irregular signals. Then, implanting a pacemaker to regulate the heartbeat. It’s for patients with symptomatic AFib who can’t have catheter ablation.
Are pacemakers used for atrial fibrillation?
Yes, pacemakers are used for AFib. They help manage heart rate issues. They can be used with other therapies to improve AFib management.
How does a pacemaker help with AFib symptoms?
Pacemakers regulate the heartbeat. This reduces symptoms like palpitations, shortness of breath, and fatigue. They’re most helpful for patients with slow heart rates or pauses in rhythm.
What type of pacemaker is suitable for AFib patients?
Specialized pacemakers are best for AFib patients. These include rate-responsive pacemakers, leadless pacemakers, and MRI-compatible pacemakers. They offer better management and fewer complications.
Can I stil experience AFib episodes with a pacemaker?
Yes, a pacemaker doesn’t eliminate AFib episodes. But it can manage the heart rate and reduce symptoms. Patients with a pacemaker need to keep monitoring and managing their AFib.
Are there alternative treatments to pacemakers for AFib management?
Yes, there are other treatments. These include medications, catheter ablation, and surgery. New therapies and clinical trials also offer promising options for managing AFib.
How do I manage AFib episodes with a pacemaker?
Managing AFib episodes with a pacemaker involves regular monitoring and follow-up care. It’s important to understand activity restrictions and lifestyle considerations. Knowing about device longevity and replacement needs is also key.
Can a pacemaker stop AFib?
No, a pacemaker can’t stop AFib. But it can manage its symptoms and heart rate issues. This improves the quality of life for patients.
What happens when you go into AFib with a pacemaker?
When a patient with a pacemaker goes into AFib, the pacemaker regulates the heart rate. This reduces symptoms and improves cardiac function. But it doesn’t eliminate the AFib episode.









