It’s important to know the differences between atrial tachycardia and supraventricular tachycardia (SVT) for the right treatment. At Liv Hospital, we offer detailed care for patients from around the world. We help you understand and manage heart rhythm problems.
Both conditions cause the heart to beat too fast, but they start in different places. Atrial tachycardia starts in the atria. SVT, on the other hand, is a wider term that includes atrial tachycardia and others. Knowing the exact cause is key to finding the right treatment.
Discover 7 key differences between atrial tachycardia vs SVT, their ECG patterns, causes, and treatment options.
Key Takeaways
- Atrial tachycardia and SVT are both rapid heart rhythms but have different origins.
- Accurate diagnosis is critical for effective treatment.
- Liv Hospital offers comprehensive care for international patients.
- Understanding the differences between atrial tachycardia and SVT is vital.
- Our team provides clarity and expertise in managing cardiac arrhythmias.
Understanding Cardiac Arrhythmias
It’s important for both patients and doctors to understand cardiac arrhythmias. These are irregular heartbeats that can be too fast, too slow, or irregular. They can be caused by many things, like changes in the heart, electrical problems, or even stress or certain medicines.
Normal Heart Rhythm vs. Arrhythmias
A normal heart rhythm is steady and coordinated. But arrhythmias disrupt this, causing irregular heartbeats. The main difference is in the heart’s electrical activity. A normal heart beats between 60 to 100 times per minute. Arrhythmias can make the heart beat too fast or too slow.
Impact of Arrhythmias on Quality of Life
Arrhythmias can really affect a person’s life. Symptoms like palpitations, shortness of breath, and fatigue can make daily tasks hard. The impact can vary based on the type and severity of the arrhythmia. For example, paroxysmal atrial tachycardia (PAT) can cause sudden, unpredictable fast heart rates, making it hard to do normal things.
| Arrhythmia Type | Common Symptoms | Impact on Quality of Life |
| Atrial Tachycardia | Palpitations, shortness of breath | Reduced ability to perform daily tasks |
| Supraventricular Tachycardia (SVT) | Rapid heart rate, dizziness | Increased anxiety, limited physical activity |
Importance of Accurate Diagnosis
Getting the right diagnosis is key to treating cardiac arrhythmias. Tests like electrocardiograms (ECGs) and Holter monitors help doctors understand the arrhythmia. A correct diagnosis leads to better treatment plans, improving outcomes and lowering risks.
By knowing the difference between normal heart rhythms and arrhythmias, their effects on life, and the need for accurate diagnosis, we can better manage and treat them. This approach ensures patients get the right care for their condition.
What is Atrial Tachycardia?
Atrial tachycardia is a fast heart rhythm that starts in the upper chambers of the heart. It can cause symptoms like a racing heartbeat, shortness of breath, and feeling dizzy.
Definition and Mechanism
Atrial tachycardia happens when the heart’s upper chambers beat too fast. This is different from the normal heart rhythm. Understanding how it works is key to treating it.
There are several reasons why atrial tachycardia happens. It can be caused by abnormal electrical pathways in the heart. These can be due to heart disease, imbalances in electrolytes, or other heart issues.
Types of Atrial Tachycardia
Atrial tachycardia can be divided into different types based on its characteristics. The main types are:
- Persistent atrial tachycardia: Episodes that last more than 48 hours.
- Paroxysmal atrial tachycardia: Episodes that start and stop suddenly.
- Incessant atrial tachycardia: Almost constant episodes with brief breaks.
Each type needs a different approach to treatment.
Paroxysmal Atrial Tachycardia Explained
Paroxysmal atrial tachycardia is when the heart rhythm suddenly speeds up and then goes back to normal. It can be triggered by stress, caffeine, or some medicines. Knowing what triggers it is important for managing it.
When it happens, people might feel their heart racing, chest pain, or feel lightheaded. The length of these episodes can vary. Knowing how paroxysmal atrial tachycardia works is important for finding the right treatment.
What is Supraventricular Tachycardia?
Supraventricular tachycardia (SVT) is when the heart beats too fast. This happens because of problems in the heart’s electrical system above the ventricles. It includes different types like atrial tachycardia and AV nodal reentrant tachycardia.
Definition and Classification
SVT is a fast heart rate that starts in the upper heart chambers or the AV node. Doctors sort SVT into types based on where it starts and how it happens. Knowing the exact type of SVT is key to finding the right treatment.
“Getting SVT right is vital for good care,” say heart doctors. They must tell AVNRT from AVRT, as each has its own cause.
Types of SVT
SVT comes in several forms, each with its own traits. The main ones are:
- Atrial Tachycardia: Starts in the atria.
- AV Nodal Reentrant Tachycardia (AVNRT): Has a loop in the AV node.
- AV Reentrant Tachycardia (AVRT): Uses an extra electrical path between the atria and ventricles.
Each SVT type has its own causes and signs. Knowing the difference is not just for fun; it’s critical for treatment.
Doctors can tailor treatments by understanding SVT types. This helps patients get better faster.
Atrial Tachycardia vs SVT: 7 Key Differences
Understanding the differences between atrial tachycardia and supraventricular tachycardia (SVT) is key. Doctors need to know these differences to diagnose and treat patients correctly.
1. Origin and Mechanism
Atrial tachycardia starts in the atria and can have a fast heart rate that lasts or comes and goes. It’s often caused by an abnormal electrical focus in the atrial tissue. SVT, on the other hand, includes a range of tachycardias that start above the ventricles, like atrial tachycardia, AV nodal reentrant tachycardia (AVNRT), and AV reentrant tachycardia (AVRT).
Key differences in origin and mechanism:
| Characteristics | Atrial Tachycardia | SVT |
| Origin | Atria | Above the ventricles (various locations) |
| Mechanism | Abnormal electrical focus | Re-entry circuits or abnormal automaticity |
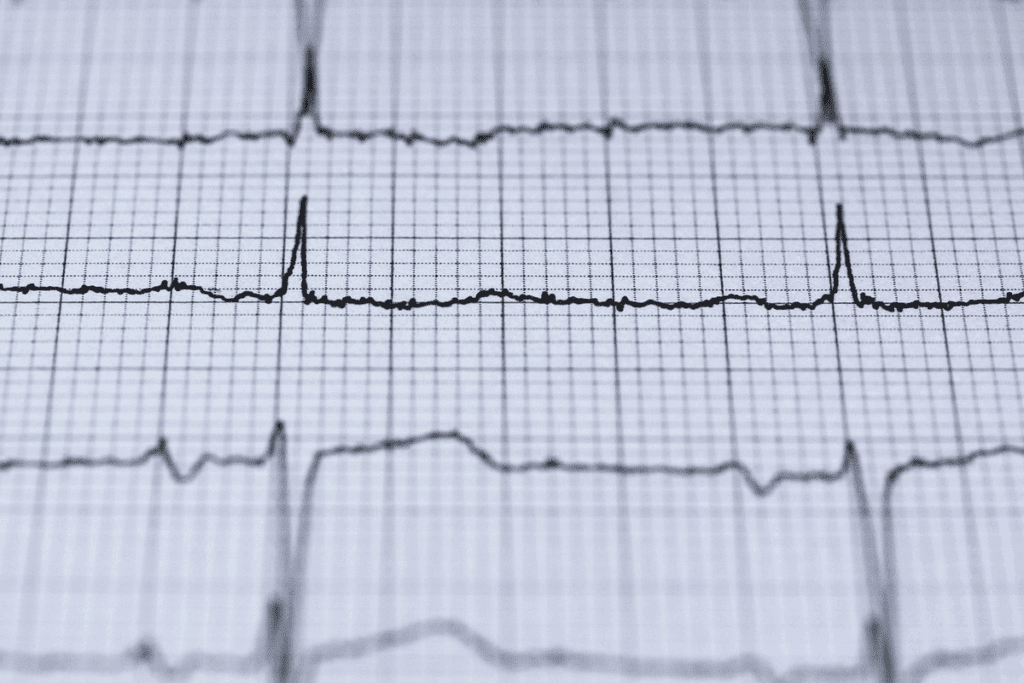
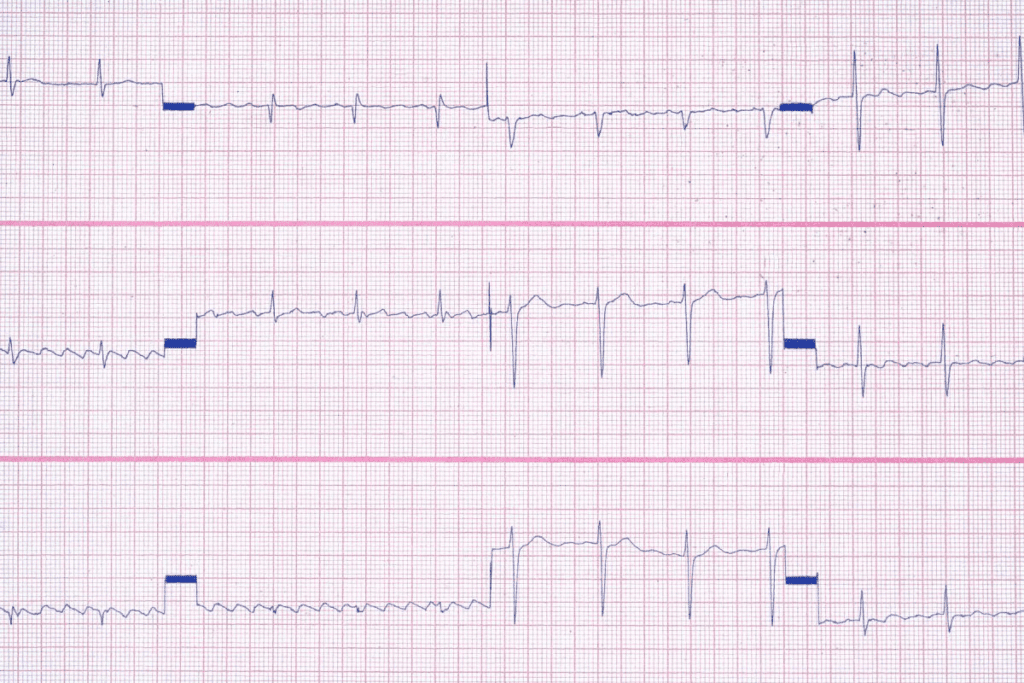
2. Electrocardiogram (ECG) Patterns
The ECG patterns for atrial tachycardia and SVT are quite different. Atrial tachycardia shows a P wave before each QRS complex, with the P wave shape changing based on the focus location. SVT, depending on its type, can show different ECG patterns.
“The ECG remains a key tool for diagnosing and differentiating between atrial tachycardia and SVT.”
3. Clinical Presentation
Both conditions can cause palpitations, dizziness, and shortness of breath. But, symptoms can vary a lot from person to person.
“Symptoms can range from mild to severe and may include chest pain, fatigue, and near-syncope. A thorough clinical evaluation is necessary to determine the underlying cause of the symptoms.”
— Medical Expert, Cardiologist
4. Triggers and Risk Factors
Stress, caffeine, and heart disease are triggers and risk factors for both conditions. Managing these factors is important to reduce episode frequency and severity.
By knowing the 7 key differences between atrial tachycardia and SVT, healthcare providers can create specific treatment plans for each patient.
Common Symptoms and Warning Signs
Knowing the signs of atrial tachycardia and SVT is key for quick medical help. Both can really affect a person’s life quality. Spotting their warning signs is vital for good care.
Shared Symptoms Between AT and SVT
Atrial tachycardia (AT) and supraventricular tachycardia (SVT) share many symptoms. This makes it hard to tell them apart. Common signs include:
- Palpitations or a feeling of a fast heartbeat
- Chest discomfort or pain
- Shortness of breath
- Dizziness or feeling lightheaded
- Fatigue or feeling generally unwell
These symptoms happen because both conditions cause abnormal heart rhythms. This can make the heart pump less efficiently.
Unique Symptoms of Atrial Tachycardia
While many symptoms are the same, atrial tachycardia has some special signs. For example, AT might cause:
- Prolonged episodes of tachycardia, lasting hours or days
- Variable ventricular response, leading to irregular palpitations
Knowing these differences is important for correct diagnosis and treatment.
When to Seek Medical Attention
It’s important to see a doctor if symptoms don’t go away or get worse. You should get medical help right away if you have:
- Severe chest pain or trouble breathing
- Severe dizziness or fainting
- A rapid or irregular heartbeat that lasts more than a few minutes
Quick medical help can greatly improve outcomes for those with atrial tachycardia or SVT. If you’re feeling any of these symptoms, call your healthcare provider right away.
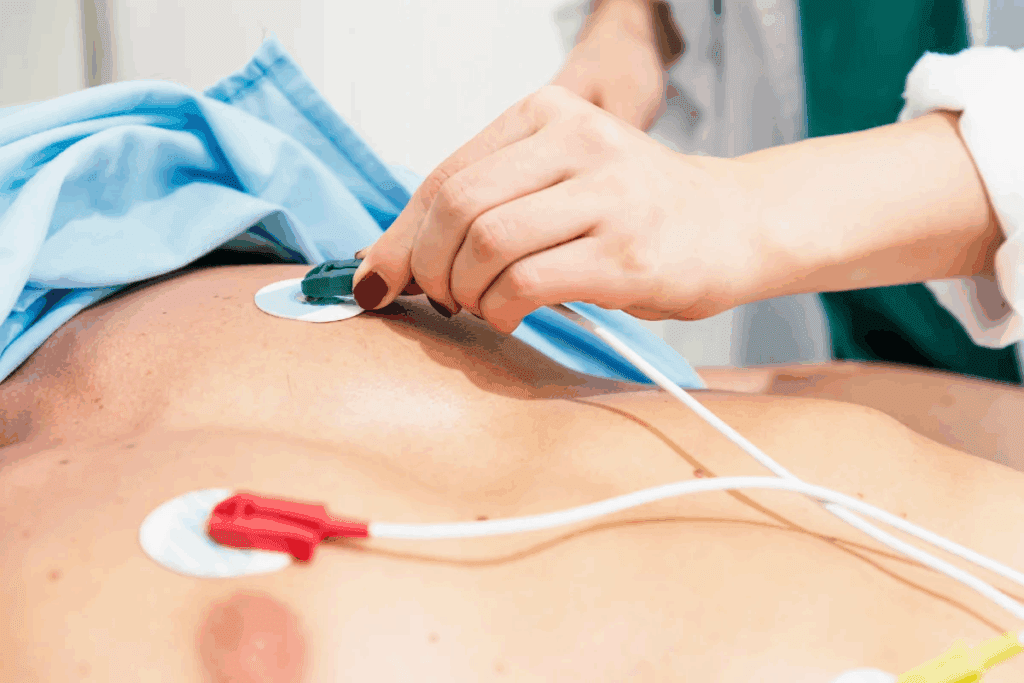
Diagnostic Approaches for Accurate Identification
To manage atrial tachycardia and SVT well, we need to diagnose them accurately. We use a mix of first checks, ECG results, and more detailed tests to decide on treatments.
Initial Assessment and History Taking
The first step is a detailed check and talking to the patient. We learn about their symptoms, health history, and lifestyle. This helps us find out what might cause atrial tachycardia and SVT.
Key elements of the initial assessment include:
- Detailed medical history
- Symptom characterization
- Lifestyle and environmental factors
Electrocardiogram (ECG) Findings
The electrocardiogram (ECG) is key in diagnosing atrial tachycardia and SVT. We look at ECG results to spot special patterns and understand how arrhythmias work.
ECG findings help us tell apart atrial tachycardia and SVT by showing:
- P-wave shape and direction
- Heart rate and rhythm
- Any AV block
Advanced Diagnostic Methods
Sometimes, we need more detailed tests to confirm a diagnosis or plan treatment. These might include electrophysiology studies (EPS) or other special tests.
Advanced diagnostic methods offer:
- More info on arrhythmia causes
- Spotting possible targets for ablation
- Help for device therapy
By using first checks, ECG results, and more detailed tests, we can make sure we diagnose atrial tachycardia and SVT right. Then, we can create good treatment plans for our patients.
Treatment Options for Atrial Tachycardia
There are many ways to treat atrial tachycardia. Each treatment is chosen based on the patient’s needs. This includes the cause of the condition, symptoms, and overall health.
Acute Management Strategies
Quick actions are key when treating atrial tachycardia. These can include:
- Vagal maneuvers to slow the heart rate
- Cardioversion, which uses electrical shocks to fix the rhythm
- Anti-arrhythmic medications to control the heart rate or fix the rhythm
These steps are taken in emergencies or when symptoms are severe.
Pharmacological Treatments
Medicines play a big role in treating atrial tachycardia. They can help control the heart rate, fix the rhythm, or stop future episodes. Common medicines include:
| Medication Type | Examples | Purpose |
| Beta Blockers | Metoprolol, Propranolol | Control heart rate |
| Anti-arrhythmic Drugs | Flecainide, Amiodarone | Fix the rhythm |
| Calcium Channel Blockers | Verapamil, Diltiazem | Control heart rate |
The American Heart Association says, “anti-arrhythmic medicines help keep the rhythm normal and stop atrial tachycardia from coming back.”
“The right medicine depends on the patient’s condition, how often episodes happen, and how well they can handle the medicine.”
Catheter Ablation for Atrial Tachycardia
Catheter ablation is a less invasive method that works well for many. It uses catheters to destroy the bad electrical pathway in the heart. This stops the arrhythmia.
Many patients choose catheter ablation because it’s very effective. It can greatly reduce or get rid of symptoms.
Success Rates and Outcomes
How well catheter ablation works depends on several things. These include where the arrhythmia is, the patient’s health, and the doctor’s skill. Studies show:
- Success rates are 70% to 90% for the right patients
- Complications are rare, affecting less than 5% of patients
- Some might need the procedure again
Catheter ablation is a good option for many with atrial tachycardia. It can greatly improve their quality of life.
Treatment Options for SVT
SVT treatment is tailored to each person. It considers their unique situation and health history. Understanding the different ways to manage SVT is key.
Acute Management Strategies
Acute SVT management aims to stop the episode and get the heart back to normal. This can be done with simple methods like the Valsalva maneuver or more complex medical treatments.
Vagal Maneuvers
Vagal maneuvers are simple, non-invasive ways to stop SVT episodes. They work by stimulating the vagus nerve. Techniques like the Valsalva maneuver and carotid massage are often recommended first.
Pharmacological Treatments
If vagal maneuvers don’t work, medication might be needed. Adenosine is often used because it’s effective and has a short half-life. Beta-blockers or calcium channel blockers can help prevent SVT from coming back.
Catheter Ablation for Different SVT Types
Catheter ablation is a highly effective treatment for many SVT types. It aims to cure SVT by destroying the abnormal electrical pathway in the heart. Success depends on the SVT type and the pathway’s location.
Here’s a summary of the treatment options for different types of SVT:
| SVT Type | Treatment Options | Success Rate |
| AVNRT | Catheter Ablation, Pharmacological Treatment | High |
| AVRT | Catheter Ablation, Pharmacological Treatment | High |
| Atrial Tachycardia | Catheter Ablation, Pharmacological Treatment | Moderate to High |
We stress the need for personalized SVT treatment plans. These plans should consider the SVT type, the patient’s health, and their preferences.
Paroxysmal Atrial Tachycardia: Special Considerations
Paroxysmal atrial tachycardia is a tricky condition to handle. It happens suddenly and can stop just as fast. This makes it hard for patients to know what’s causing it.
Defining Characteristics
Paroxysmal atrial tachycardia is known for its sudden start and stop. It can be spotted on an electrocardiogram (ECG) by a fast heart rate. This rate is usually between 100 to 250 beats per minute.
Key Features:
- Sudden onset and termination
- Rapid atrial rate
- Often associated with symptoms like palpitations and dizziness
Management Challenges
Handling PAT is tough because it comes and goes. Patients might not have episodes often. So, it’s key to watch them closely to figure out what’s happening.
Common Management Challenges:
- Difficulty in capturing episodes during diagnostic tests
- Variability in symptom severity and frequency
- Need for personalized treatment plans
Long-term Monitoring Approaches
Keeping an eye on PAT over time is vital. Tools like Holter monitors, event recorders, or implantable loop recorders help. They catch episodes and find out what causes them.
Monitoring Strategies:
- Holter monitoring for continuous recording
- Event recorders for capturing infrequent episodes
- Implantable loop recorders for long-term tracking
Quality of Life Impact
Paroxysmal atrial tachycardia can really affect a person’s life. The unpredictable nature of episodes can cause worry and limit what they can do.
Improving Quality of Life:
- Lifestyle modifications to reduce triggers
- Stress management techniques
- Adherence to treatment plans
Understanding PAT’s special needs helps doctors manage it better. This leads to better care and a better life for patients.
Living with Cardiac Arrhythmias: Lifestyle Modifications
Managing cardiac arrhythmias requires medical treatment and lifestyle changes. These changes can greatly improve your life quality. By making the right lifestyle adjustments, you can better handle your symptoms and feel better overall.
Stress Management Techniques
Stress can make cardiac arrhythmias worse. It’s key to manage stress well. Meditation, deep breathing, and yoga are great for reducing stress. Try to make these activities a part of your daily life to help manage stress and reduce arrhythmia episodes.
Keeping a healthy work-life balance is also important. Doing things that bring you joy and relaxation can help manage stress. Find what works best for you and make it a regular part of your life.
Dietary Considerations
Your diet is very important when managing cardiac arrhythmias. Eating a heart-healthy diet with lots of fruits, vegetables, whole grains, and lean proteins is beneficial. Avoid too much caffeine, alcohol, and high-sodium foods as they can trigger or worsen arrhythmias.
Drinking plenty of water is also key. Some people might need to avoid foods high in sugar or saturated fats. Keeping a food diary can help you find out what foods might trigger arrhythmias for you.
Exercise Recommendations
Regular exercise is good for heart health and can reduce symptoms of cardiac arrhythmias. Choose low-intensity exercises like walking, swimming, or cycling. These are less likely to trigger arrhythmias than high-intensity or contact sports.
Always talk to your healthcare provider before starting any new exercise program. They can help you choose the best activities for your condition and health. Listen to your body and adjust your exercise routine as needed.
Monitoring and Self-Care Strategies
Self-care and monitoring are essential for managing cardiac arrhythmias. Be aware of how your body reacts to different activities, medications, and lifestyle changes. Keeping a symptom journal can help you track patterns and find triggers, which is useful to share with your healthcare provider.
Regular check-ups with your healthcare provider are also important. They help monitor your condition and adjust your treatment plan as needed. By being proactive in your care and making informed lifestyle choices, you can improve your quality of life and better manage your cardiac arrhythmias.
Conclusion
It’s important to know the difference between atrial tachycardia and supraventricular tachycardia (SVT) for the right treatment. This article has covered their unique signs, symptoms, and treatment choices.
Both conditions need a detailed approach for diagnosis and treatment. We talked about the role of ECGs, advanced tests, and treatments like medicines and catheter ablation.
Our hospital is dedicated to top-notch healthcare for all patients, including those from abroad. Our team works hard to give each patient the care they need, aiming for the best results.
We aim to help people with atrial tachycardia and SVT live better lives. By giving them the right treatment and information, we help them manage their health and reach their health goals.
FAQ
What is the difference between atrial tachycardia and supraventricular tachycardia?
Atrial tachycardia starts in the atria. Supraventricular tachycardia (SVT) is a wider term. It includes atrial tachycardia and other tachycardias above the ventricles.
What is paroxysmal atrial tachycardia?
Paroxysmal atrial tachycardia (PAT) is a sudden and short-lived fast heart rate. It often has a regular rhythm.
How is atrial tachycardia diagnosed?
Doctors use an electrocardiogram (ECG) to find atrial tachycardia. The ECG shows a fast, regular heart rate. It might also show varying degrees of AV block.
What are the treatment options for atrial tachycardia?
Treatments for atrial tachycardia vary. They include quick fixes, medicines, and catheter ablation. The choice depends on the cause and the patient.
How does SVT differ from atrial tachycardia?
SVT is a broader term. It includes atrial tachycardia, AV nodal reentrant tachycardia (AVNRT), and AV reentrant tachycardia (AVRT). Atrial tachycardia is a specific type of SVT from the atria.
What are the symptoms of paroxysmal atrial tachycardia?
PAT symptoms include palpitations, rapid heartbeat, dizziness, and shortness of breath. Chest discomfort is also common. These symptoms come on suddenly and stop just as fast.
Can lifestyle modifications help manage cardiac arrhythmias?
Yes, making lifestyle changes can help. Stress management, diet, exercise, and self-care can improve life quality and manage symptoms.
What is the role of catheter ablation in treating atrial tachycardia and SVT?
Catheter ablation is a procedure to treat atrial tachycardia and some SVTs. It removes the bad electrical pathways or foci.
How can I manage stress related to cardiac arrhythmias?
Stress management techniques like meditation, deep breathing, and yoga can help. They reduce stress and anxiety related to heart rhythm problems.
Are there any dietary recommendations for individuals with cardiac arrhythmias?
Eating a balanced diet with fruits, vegetables, whole grains, and lean proteins is good. Avoiding caffeine and heavy meals can also help manage symptoms.
References
- Liwanag, M., & Willoughby, C. (2023, June 26). Atrial tachycardia. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK542235/
- Kotadia, I. D., et al. (2020). Supraventricular tachycardia: An overview of diagnosis and management. Progress in Cardiovascular Diseases, https://www.sciencedirect.com/science/article/pii/S1470211824036510