Last Updated on November 25, 2025 by Ugurkan Demir
Learn what atherosclerotic coronary artery disease is and how it differs from atherosclerosis.
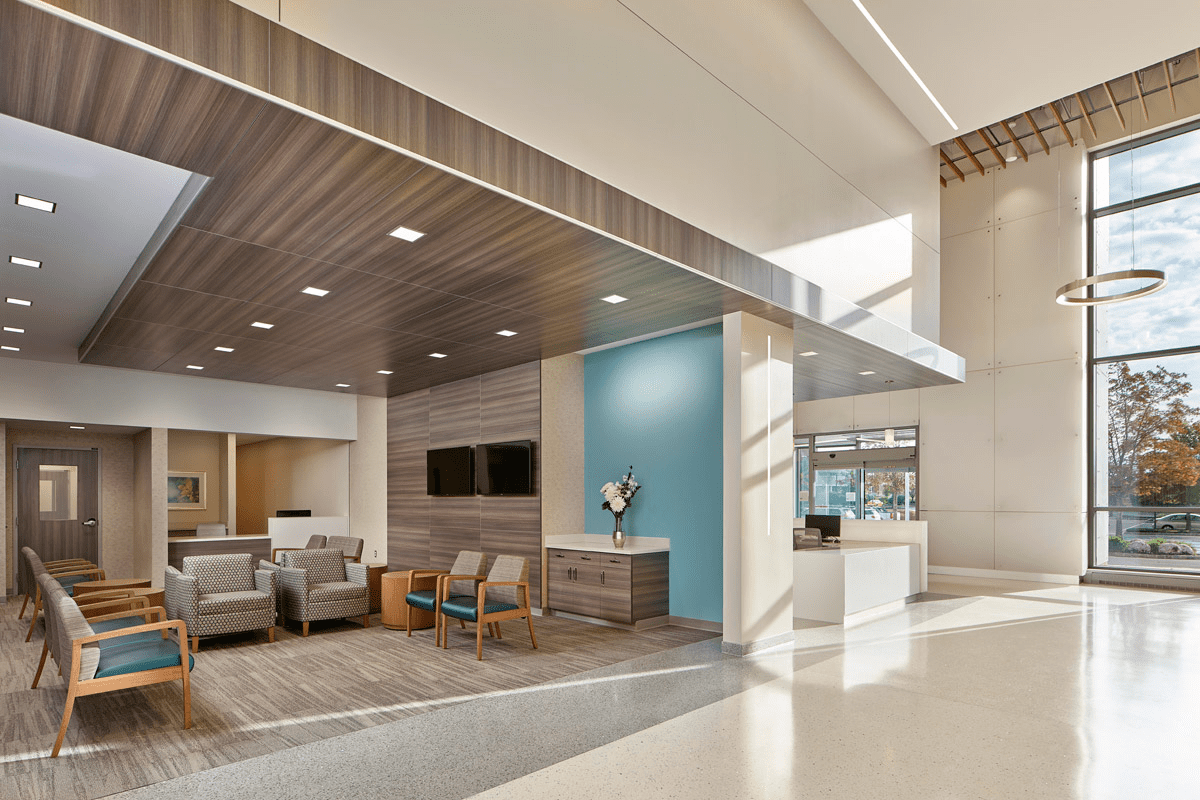
Knowing the difference between atherosclerotic coronary artery disease and atherosclerosis is key to good heart health. At LivHospital, we focus on patient care with the latest methods.
Atherosclerosis is when plaque builds up in the arteries, causing heart problems. When this happens in the coronary arteries, it’s called atherosclerotic coronary artery disease or coronary artery disease.
We understand the need to treat these conditions differently. Our care plan includes both preventing and treating heart issues.
Key Takeaways
- It’s important to know the difference between atherosclerosis and atherosclerotic coronary artery disease.
- Atherosclerosis is a condition where plaque builds up in any artery.
- Atherosclerotic coronary artery disease is when plaque builds up in the coronary arteries.
- LivHospital is committed to giving top-notch cardiovascular care.
- Good management means using both prevention and treatment.
The Fundamentals of Cardiovascular Disease

The heart relies on the coronary arteries to get the blood it needs. This system is key for delivering oxygen and nutrients to the heart. It helps the heart pump blood well throughout the body.
The Coronary Arterial System
The coronary arteries branch off from the aorta, the main artery from the heart. They circle the heart, bringing blood to different areas. The left and right coronary arteries split into smaller branches, like the left anterior descending artery and the circumflex artery.
| Coronary Artery | Region Supplied | Function |
| Left Coronary Artery | Anterior and lateral walls of the left ventricle | Supplies blood to a significant portion of the left ventricle |
| Right Coronary Artery | Right ventricle, parts of the left ventricle, and the atria | Supplies blood to the right ventricle and parts of the left ventricle |
| Left Anterior Descending Artery | Anterior wall of the left ventricle and the anterior two-thirds of the interventricular septum | Critical for supplying blood to the anterior wall and septum |
Importance of Coronary Blood Flow
Coronary blood flow is vital for the heart’s function. A decrease in blood flow can cause ischemia, where the heart muscle lacks oxygen and nutrients. This can lead to a heart attack if not addressed.
Factors Affecting Coronary Blood Flow:
- Atherosclerosis: Plaque buildup in the coronary arteries
- Thrombosis: Formation of blood clots within the coronary arteries
- Vasospasm: Sudden constriction of the coronary arteries
Knowing these factors helps in managing and preventing coronary artery disease. A healthy lifestyle and addressing risk factors can lower the chance of cardiovascular disease.
What Is Atherosclerotic Coronary Artery Disease?

Atherosclerotic coronary artery disease is a serious condition. It happens when plaque builds up in the coronary arteries. This buildup causes the arteries to narrow and harden.
Definition and Pathophysiology
This disease affects the coronary arteries, which carry blood to the heart. Atherosclerosis is when plaque, made of fat, cholesterol, and more, builds up in these arteries.
The disease’s causes are complex. They include:
- Endothelial dysfunction
- Inflammation
- Lipid accumulation
- Smooth muscle cell proliferation
- Calcification
Plaque Composition and Development
Atherosclerotic plaques are made of different parts. They include a lipid core, a fibrous cap, and inflammatory cells. Plaque development is slow and can be influenced by many factors.
This disease can cause different symptoms. These include:
- Stable angina
- Acute coronary syndromes (ACS)
- Myocardial infarction
Knowing the difference between stable and unstable plaques is key. We will explore the clinical implications and how to manage it in the next sections.
Atherosclerosis vs. Coronary Artery Disease: Understanding the Distinction
Atherosclerosis and coronary artery disease are often confused, but they’re not the same. Knowing the difference is key to treating heart diseases well.
Atherosclerosis as a Systemic Process
Atherosclerosis is a widespread condition where plaque builds up in arteries all over the body. This can happen in arteries of the heart, brain, and legs. The plaque is made of cholesterol, fats, calcium, and more.
Key features of atherosclerosis include:
- Systemic involvement of multiple arterial beds
- Plaque formation and progression
- Potential for complications such as thrombosis and embolism
Coronary Artery Disease as a Specific Manifestation
Coronary artery disease (CAD) is a part of atherosclerosis that affects the heart’s blood supply. It happens when the heart’s arteries get narrowed or blocked by plaque. This reduces blood flow to the heart.
The clinical implications of CAD include:
- Angina pectoris (chest pain)
- Myocardial infarction (heart attack)
- Heart failure
Clinical Terminology and Distinctions
In medical terms, atherosclerosis and coronary artery disease describe different parts of heart disease. Atherosclerosis is the broader term for the disease’s widespread nature. Coronary artery disease, on the other hand, focuses on the heart’s arteries.
It’s important for doctors to understand these differences. This helps them diagnose and treat heart diseases better. By knowing atherosclerosis’s widespread nature and CAD’s specific effects, doctors can tailor treatments for better patient care.
The Progressive Nature of Atherosclerotic Coronary Artery Disease
It’s key to grasp how atherosclerotic coronary artery disease progresses. This disease starts with plaque formation and can lead to unstable lesions. Knowing this helps in managing the disease effectively.
Stages of Plaque Formation
Plaque formation in atherosclerotic coronary artery disease is complex. It begins with lipid accumulation in the arterial wall. Then, inflammatory cells join in.
As the plaque grows, it can become fibrotic. This happens with the formation of a fibrous cap.
The stages of plaque formation are:
| Stage | Description |
| Initial | Lipid accumulation and inflammatory cell recruitment |
| Progression | Plaque growth with continued lipid accumulation and inflammation |
| Complication | Plaque destabilization with possible rupture |
From Stable to Unstable Plaques
Plaques can change from stable to unstable. Stable plaques have a thick fibrous cap and are less likely to rupture. On the other hand, unstable plaques have a thin cap and are more likely to rupture, causing heart attacks.
What makes a plaque unstable includes:
- Increased inflammation
- More lipid accumulation
- A weaker fibrous cap
Understanding these changes is vital for managing atherosclerotic coronary artery disease.
Epidemiology and Global Impact
Atherosclerotic coronary artery disease is a big problem worldwide. It causes a lot of sickness and death. It also puts a big strain on healthcare systems everywhere.
Prevalence Rates in the United States and Worldwide
This disease is a big worry in the United States and around the world. More people are getting it because of aging, lifestyle changes, and more risk factors like high blood pressure and diabetes.
In the United States, it’s one of the top heart diseases, affecting millions. It’s expected to get worse because of more older people and more obesity and other heart risks.
Mortality and Economic Burden
This disease has a big impact, not just on how many people get it. It also affects how many die and the economy. It’s a top cause of death, leading to big healthcare costs and lost work.
| Region | Mortality Rate (per 100,000) | Economic Burden (billion USD) |
| United States | 120 | 200 |
| Europe | 150 | 250 |
| Global | 180 | 500 |
The costs include direct medical expenses and lost work. Knowing this helps us make better plans to fight this disease.
Risk Factors for Developing Atherosclerotic Coronary Artery Disease
It’s important to know the risk factors for atherosclerotic coronary artery disease. This knowledge helps in preventing and managing the condition. We focus on these factors to lower the risk of getting this disease.
Modifiable Risk Factors
Modifiable risk factors are things we can change. They include lifestyle choices and medical treatments. The main modifiable risk factors are:
- High Cholesterol: High levels of LDL cholesterol can cause artery plaque.
- Hypertension: High blood pressure can harm artery walls, making them more prone to plaque.
- Diabetes: Diabetes, mainly type 2, raises the risk of atherosclerotic coronary artery disease due to metabolic changes.
- Smoking: Smoking is a big risk factor as it harms the heart and reduces blood flow.
Changing these risk factors through healthy living can greatly reduce the risk of atherosclerotic coronary artery disease.
Non-Modifiable Risk Factors
Non-modifiable risk factors are things we can’t change. These include:
- Genetics: A family history of coronary artery disease increases your risk.
- Age: The risk of atherosclerotic coronary artery disease grows with age.
- Gender: Men are generally at higher risk than women, but women’s risk increases after menopause.
Even though we can’t change non-modifiable risk factors, knowing them helps in creating effective prevention plans and monitoring.
By tackling both modifiable and non-modifiable risk factors, we can take a complete approach to preventing and managing atherosclerotic coronary artery disease.
Clinical Manifestations and Diagnostic Approaches
It’s important to know the signs of atherosclerotic coronary artery disease early. This disease can show no symptoms or cause serious problems like a heart attack.
Symptoms and Warning Signs
People with this disease might feel chest pain (angina pectoris), shortness of breath, or fatigue. These feelings happen because the heart doesn’t get enough blood. This is due to plaque in the coronary arteries.
It’s key to notice these signs and get help right away. We should teach patients to seek medical help if they have these symptoms.
Non-Invasive Diagnostic Methods
There are ways to check for this disease without surgery. These include:
- Electrocardiogram (ECG): This test shows the heart’s electrical activity. It can spot signs of heart problems.
- Stress Test: This test checks how the heart works when it’s stressed. It uses exercise or medicine.
- Coronary Computed Tomography Angiography (CCTA): This test gives clear pictures of the heart’s arteries. It helps see how much plaque there is.
These tests help find out who is at risk. They guide what steps to take next.
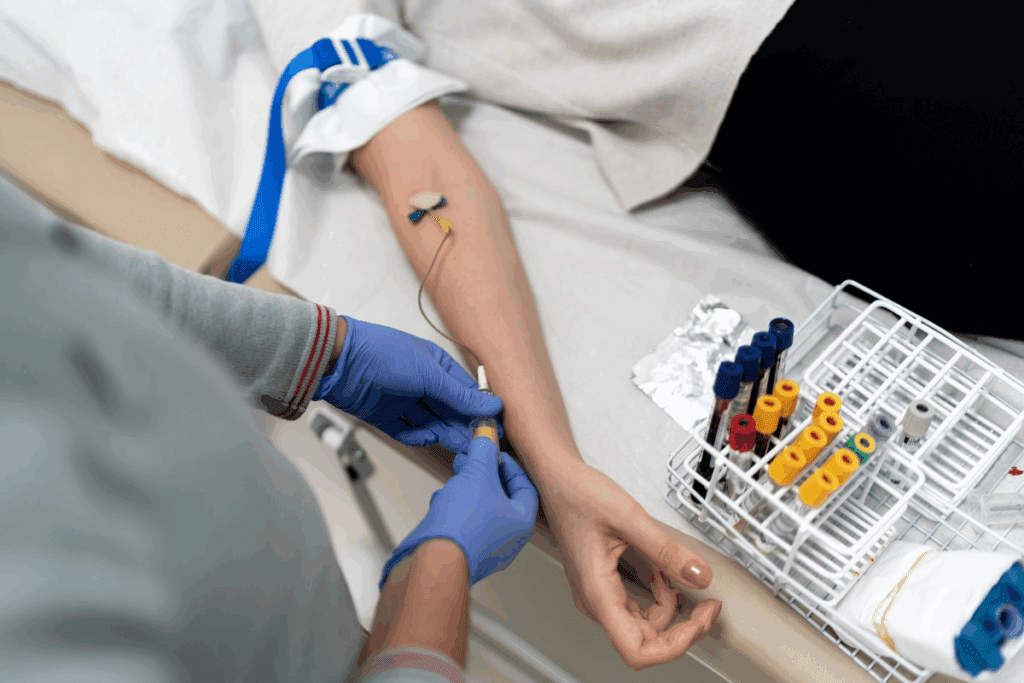
Invasive Diagnostic Procedures
Sometimes, we need to do more to figure out the disease. This is when we use invasive tests.
The main invasive test is Coronary Angiography. It uses contrast to see inside the arteries. It shows if there are blockages.
| Diagnostic Method | Description | Clinical Utility |
| Electrocardiogram (ECG) | Records heart electrical activity | Identifies ischemia or infarction |
| Stress Test | Evaluates heart function under stress | Assesses coronary artery disease severity |
| Coronary Angiography | Visualizes coronary artery lumen | Identifies stenoses or occlusions |
By using these tests together, we can find and treat the disease well.
Comprehensive Management Strategies
Managing atherosclerotic coronary artery disease needs a mix of lifestyle changes, medical treatments, and procedures. We’ll cover the key strategies for this condition. It’s all about working together to care for patients.
Lifestyle Modifications
Making lifestyle changes is key in managing atherosclerotic coronary artery disease. These changes can slow the disease, lessen symptoms, and boost heart health.
- Dietary changes: Eating a diet full of fruits, veggies, whole grains, and lean proteins can control cholesterol and blood pressure.
- Physical activity: Regular exercise, like brisk walking, can make your heart stronger and lower risk.
- Smoking cessation: Quitting smoking is vital to lower heart disease risk and slow disease growth.
- Weight management: Keeping a healthy weight through diet and exercise can manage disease risk factors.
Pharmacological Interventions
Medicines are a big part of managing atherosclerotic coronary artery disease. They can control symptoms, slow disease, and lower heart event risk.
| Medication Class | Primary Use | Examples |
| Statins | Lowering LDL cholesterol | Atorvastatin, Simvastatin |
| Beta-blockers | Reducing myocardial oxygen demand | Metoprolol, Atenolol |
| Antiplatelet agents | Preventing thrombosis | Aspirin, Clopidogrel |
Revascularization Procedures
Revascularization procedures are vital for getting blood to the heart in severe disease. These procedures can save lives and improve life quality.
Key revascularization techniques include:
- Coronary artery bypass grafting (CABG): A surgery that uses grafts to bypass blocked arteries.
- Percutaneous coronary intervention (PCI): A less invasive method that uses stents to open blocked arteries.
By combining lifestyle changes, medicines, and procedures, healthcare teams can offer full care for atherosclerotic coronary artery disease. This approach improves outcomes and life quality for patients.
Conclusion: Prevention and Future Directions in Atherosclerotic Heart Disease
Prevention and early action are key to fighting atherosclerotic heart disease. We’ve looked into the details of this disease, from what it is to how to manage it. This includes its causes and how to treat it.
It’s important to see atherosclerosis as a whole-body issue. This means treating it with a wide-ranging approach. This includes changing our lifestyle and using medicine.
New research and treatments are on the horizon. These could greatly help those with atherosclerotic heart disease. By focusing on prevention and keeping up with new findings, we can lessen the disease’s global impact.
The link between atherosclerosis and CAD is complex. By tackling the disease’s causes and progression, we can find better ways to prevent and treat it.
FAQ
What is the difference between atherosclerosis and coronary artery disease?
Atherosclerosis is a condition where plaque builds up in arteries. Coronary artery disease is a specific case of atherosclerosis. It affects the arteries that supply blood to the heart.
Is atherosclerosis coronary artery disease?
No, not exactly. Atherosclerosis is a wider condition that can happen in any artery. Coronary artery disease is a specific case of it, affecting the heart’s arteries.
What is atherosclerotic coronary artery disease?
Atherosclerotic coronary artery disease is when the heart’s arteries narrow or get blocked. This is due to plaque buildup. It can reduce blood flow to the heart and might cause a heart attack.
What are the risk factors for developing atherosclerotic coronary artery disease?
High blood pressure, high cholesterol, smoking, and diabetes are modifiable risk factors. Non-modifiable factors include age, family history, and genetics.
How is atherosclerotic coronary artery disease diagnosed?
Diagnosis uses non-invasive tests like electrocardiograms and stress tests. It also involves invasive procedures, such as coronary angiography.
What are the symptoms of atherosclerotic coronary artery disease?
Symptoms include chest pain or discomfort, shortness of breath, and fatigue. Some people might not show symptoms until they have a heart attack.
How is atherosclerotic coronary artery disease managed?
Management includes lifestyle changes, medicines, and procedures like angioplasty. Coronary artery bypass grafting is also used.
Can atherosclerotic coronary artery disease be prevented?
Yes, prevention is possible. It involves a healthy lifestyle, managing risk factors, and medical interventions.
What is the difference between coronary atherosclerosis and coronary artery disease?
Coronary atherosclerosis is the buildup of plaque in the heart’s arteries. Coronary artery disease is a broader term. It includes the effects of this buildup, like angina and heart attacks.
Is coronary artery atherosclerosis the same as coronary artery disease?
While often used the same way, coronary artery atherosclerosis refers to plaque buildup. Coronary artery disease is a broader term. It includes the clinical effects of this buildup.
References:
Falk, E., Kaul, S., et al. (2020). 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease. Journal of the American College of Cardiology, 74(10), 1376-1434. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7089587/