Last Updated on December 4, 2025 by Ugurkan Demir
Coronary artery disease is a serious condition that can lead to heart attacks and other life-threatening complications. Restoring healthy blood flow to the heart is key in managing this condition. We use a coronary artery bypass grafting (CABG) procedure to do this.
CABG is a surgical method that uses a blood vessel from another part of the body. It creates a detour around a blocked or narrowed coronary artery. This life-saving innovation is trusted by top medical centers like Liv Hospital. They use it to improve heart health with advanced, patient-focused care.
By creating a bypass graft, we can restore blood flow to areas of the heart that were previously deprived of oxygen and nutrients. This bypass graft significantly improves heart function and overall quality of life.
Key Takeaways
- CABG is a surgical procedure to restore blood flow to the heart.
- It involves using a blood vessel from another part of the body to bypass a blocked or narrowed coronary artery.
- The procedure is performed to manage coronary artery disease and prevent heart attacks.
- CABG can significantly improve heart function and overall quality of life.
- Top medical centers, such as Liv Hospital, offer advanced CABG surgery with patient-focused care.
Understanding Coronary Artery Bypass Graft Surgery

Coronary artery bypass grafting is a key surgery for heart disease. It helps by making a new path for blood to the heart. This is done using a healthy blood vessel from another part of the body.
Definition and Purpose of Bypass Graft Procedure
The main goal of CABG is to improve blood flow to the heart. It does this by bypassing blocked or narrowed parts of the coronary arteries. A healthy vessel, often from the leg, arm, or chest, is grafted onto the artery.
CABG is a surgical procedure that grafts a healthy blood vessel onto a coronary artery. This restores blood flow to the heart. It helps to ease symptoms of heart disease and lower the risk of heart attack.
Prevalence and Significance in Cardiac Surgery
CABG is a common major heart surgery worldwide. It is very important in cardiac surgery. It offers a vital treatment for patients with severe heart disease.
- CABG is a lifesaving procedure for many patients with severe coronary artery disease.
- The surgery has seen big improvements, making outcomes better and recovery times shorter.
- CABG is often suggested for patients who haven’t responded to other treatments or have complex disease.
CABG Terminology and Abbreviations
It’s important to know the terms and abbreviations of CABG. CABG stands for Coronary Artery Bypass Grafting. It’s also called “cabbage surgery” in medical terms.
Some key terms and abbreviations include:
- CABG: Coronary Artery Bypass Grafting
- LIMA: Left Internal Mammary Artery, a common graft source
- Saphenous Vein Graft (SVG): A graft taken from the leg
Knowing these terms helps patients understand their diagnosis and treatment options better.
Preoperative Assessment and Patient Selection

Before surgery, we carefully check who is best for CABG. This helps us lower risks and improve results.
Coronary Angiography and Imaging Evaluation
Coronary angiography is key for CABG prep. It shows us the heart’s arteries and finds blockages. We also use echocardiography and stress tests to check the heart’s function.
These tests help us choose the right surgery and grafts. For example, we often use the left internal mammary artery and saphenous vein because they work well.
Risk Stratification and Comorbidity Assessment
We look at each patient’s health and surgery risks. This includes checking for diabetes, high blood pressure, and COPD. Knowing these details helps us plan the surgery and care better for each patient.
| Comorbidity | Impact on CABG Surgery | Management Strategy |
| Diabetes | Increased risk of infection and slower healing | Optimize blood glucose control preoperatively and postoperatively |
| Hypertension | Potential for increased bleeding and cardiovascular stress | Monitor blood pressure closely and manage with medication as needed |
| COPD | Increased risk of respiratory complications | Preoperative pulmonary rehabilitation and careful postoperative respiratory management |
Informed Consent and Patient Education
Getting informed consent is very important. We make sure patients and families know about CABG. This includes its benefits, risks, and possible problems.
Teaching patients also helps them get ready for recovery. They learn what to expect and how to take care of themselves.
By doing a good job in preoperative assessment and patient selection, we make CABG safer and more effective. This leads to better results for our patients.
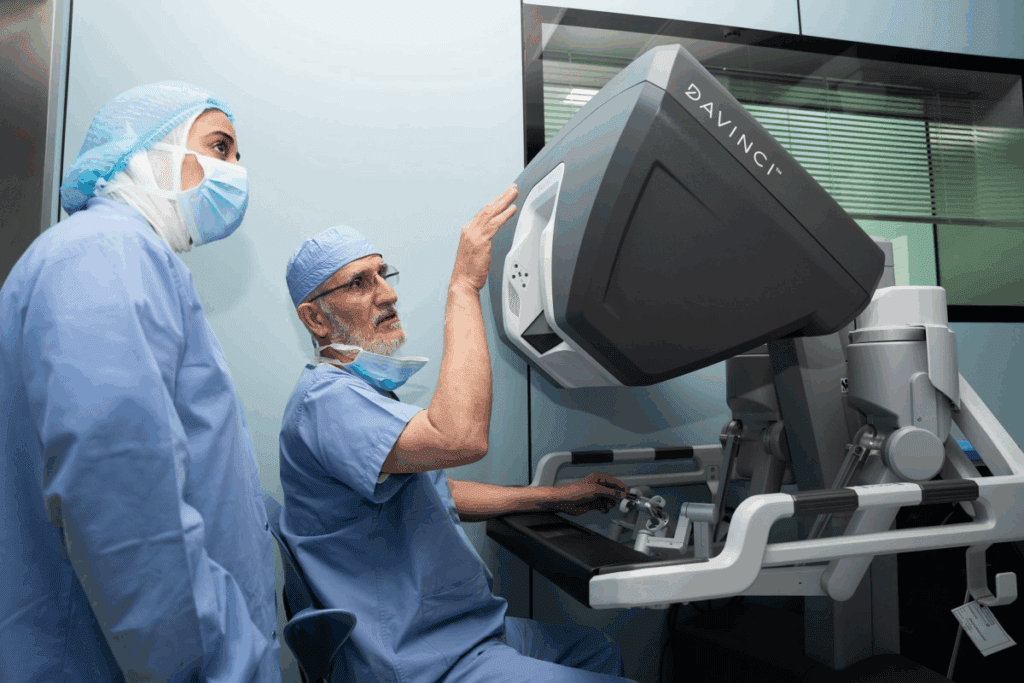
Surgical Team Preparation and Operating Room Setup
Getting ready for a CABG procedure is very detailed. It makes sure the surgical team and the operating room are ready for the complex surgery. The success of the surgery depends on the team’s skills and the setup’s precision.
Required Medical Personnel and Roles
The CABG surgical team is made up of many healthcare professionals. Each one has a key role in the surgery. The cardiovascular surgeon does the surgery. Anesthesiologists give anesthesia and watch the patient’s vital signs.
Nurses help the surgeon and watch the patient. Perfusionists run the heart-lung machine that takes over the heart and lungs’ job during surgery.
Key Roles and Responsibilities:
- Cardiovascular Surgeon: Performs the CABG surgery.
- Anesthesiologists: Administer anesthesia and monitor vital signs.
- Nurses: Assist the surgeon and monitor patient condition.
- Perfusionists: Operate the heart-lung machine.
Essential Equipment and Instrument Preparation
The operating room needs the right tools and equipment for CABG surgery. This includes surgical tools, monitoring gear, and the heart-lung machine. Getting these ready is key for a smooth surgery.
| Equipment | Purpose |
| Surgical Instruments | For performing the CABG surgery. |
| Monitoring Equipment | For monitoring the patient’s vital signs. |
| Heart-Lung Machine | For taking over the function of the heart and lungs. |
Sterile Field Establishment
Creating a sterile field is very important to avoid infections during CABG surgery. The team follows strict rules to keep everything clean and sterile. This means cleaning the room, sterilizing tools, and wearing sterile gowns and gloves.
By making sure everything is sterile and the team is ready, we can lower the risks of CABG surgery. CABG nursing is also key in recovery, monitoring, and catching any problems early. This shows how important a detailed and coordinated care plan is.
Anesthesia Protocol and Patient Positioning
To make CABG surgery go smoothly, we focus on the right anesthesia and patient positioning. This is key for the surgery’s success and the patient’s safety.
Anesthetic Agents and Administration
Choosing the right anesthetic agents is vital in CABG surgery. We mix different agents to keep the patient pain-free and asleep. The choice depends on the patient’s health and the team’s preference.
Some common anesthetic agents include:
- Propofol
- Fentanyl
- Midazolam
Hemodynamic Monitoring Setup
Hemodynamic monitoring is key for managing the patient’s heart during CABG surgery. We use tools like arterial lines and central venous catheters. These help us watch the patient’s blood pressure and heart function closely.
The main parts of hemodynamic monitoring are:
- Arterial blood pressure monitoring
- Central venous pressure monitoring
- Cardiac output monitoring
Optimal Patient Positioning for Sternotomy
Getting the patient’s position right is essential for a successful sternotomy. We place them on their back with arms secured for chest access. The neck is slightly bent to make the incision easier.
The benefits of the right patient position are:
- Improved surgical access
- Reduced risk of complications
- Enhanced patient safety
Harvesting Bypass Graft Vessels
In CABG surgery, picking and harvesting graft vessels is key to success. The left internal mammary artery and saphenous vein are top choices. The right one depends on the patient’s body and the surgeon’s style.
Left Internal Mammary Artery (LIMA) Harvesting Technique
The LIMA is a top pick because it works well over time and helps patients live longer. We carefully dissect the LIMA from the thoracic wall, making sure not to harm it or the nearby tissues. Using LIMA in CABG lowers the chance of heart problems and boosts survival chances.
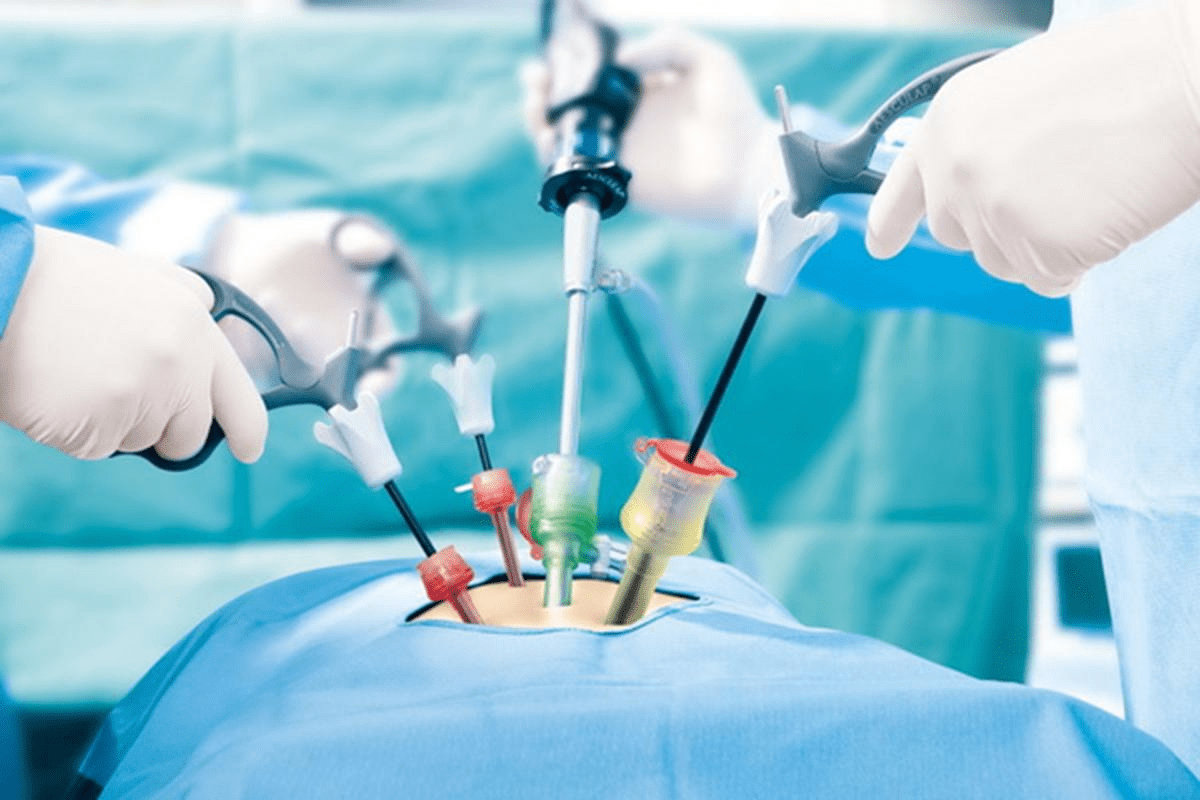
Saphenous Vein Extraction and Preparation
The saphenous vein is also a common choice for CABG. We use a minimally invasive method to get the saphenous vein, cutting down on risks and speeding up recovery. We then get it ready for grafting by removing branches and valves and checking for leaks.
| Graft Type | Advantages | Considerations |
| Left Internal Mammary Artery (LIMA) | High long-term patency rates, improved patient survival | Technical challenge in harvesting, limited length |
| Saphenous Vein | Easily accessible, sufficient length for multiple grafts | Lower long-term patency compared to arterial grafts |
Alternative Conduits: Radial Artery and Right Internal Mammary Artery
In some cases, we use the radial artery and Right Internal Mammary Artery (RIMA) as alternatives. The radial artery is great for patients at risk of vein graft disease. RIMA is used in bilateral internal mammary artery grafting, which benefits some patients.
“The choice of graft vessel is critical in CABG surgery, influencing both short-term and long-term outcomes.”
— Cardiac Surgery Expert
Knowing the pros and cons of each graft helps us customize CABG for each patient. This approach improves outcomes and enhances life quality.
Establishing Cardiopulmonary Bypass
Cardiopulmonary bypass is key in CABG surgery. It lets surgeons work on a heart that’s not beating. This method is vital for the success of the surgery, making grafting precise and reducing risks.
Aortic and Venous Cannulation Techniques
Cannulation is when tubes are put into the aorta and veins to divert blood. Aortic cannulation means putting a tube in the aorta’s top part. Venous cannulation usually involves putting a tube in the right atrium or vena cava.
The choice of cannulation depends on the patient’s body and the surgeon’s choice. Getting cannulation right is key to effective bypass and avoiding problems.
Initiating and Managing the Bypass Circuit
After cannulation, the bypass circuit starts. The perfusionist is important here, watching flow rate, pressure, and temperature.
| Parameter | Normal Range | Significance |
| Flow Rate | 2.4-4.0 L/min/m^2 | Ensures adequate perfusion of vital organs |
| Mean Arterial Pressure | 50-70 mmHg | Maintains optimal blood pressure during bypass |
| Temperature | 32-36°C | Reduces metabolic rate and oxygen demand |
Myocardial Protection and Cardioplegia Administration
Protecting the heart is vital in CABG surgery. Cardioplegia is used to stop the heart and lower its activity. It’s given through the heart’s blood vessels to cool it and stop its electrical activity.
Cardioplegia is given at set times to keep the heart safe during the surgery. The solution used can change based on the hospital’s rules and the patient’s needs.
Understanding and setting up cardiopulmonary bypass well helps surgeons do CABG safely and effectively. This improves the patient’s chances of a good outcome.
Step-by-Step Bypass Grafting Procedure
Coronary artery bypass graft surgery is a detailed process. It starts with picking the right spots on the coronary arteries. Then, it moves to the distal and proximal anastomoses.
Coronary Artery Target Site Selection and Preparation
The first step is to choose the right spots on the coronary arteries. The surgeon looks for areas most damaged by disease. They use coronary angiography to find these spots.
Preparing these spots is key for success. It means removing plaque and making sure the area is ready for stitches.
Distal Anastomosis Technique and Suturing Methods
After preparing the spots, the surgeon does the distal anastomosis. This is when they sew the graft to the coronary artery. The method used here is very important for the graft’s success.
Surgeons use different ways to sew, like continuous or interrupted suturing. The choice depends on the surgery and the surgeon’s style.
Proximal Anastomosis to the Aorta
Next, the surgeon works on the proximal anastomosis. This is where the graft connects to the aorta. It’s vital for the bypass to work right.
The surgeon carefully sews the graft to the aortic wall. This makes sure the connection is strong and won’t leak.
Sequential and Multiple Grafting Approaches
In some cases, surgeons use sequential or multiple grafting. Sequential grafting uses one graft for many branches. Multiple grafting uses several grafts for different blockages.
- Sequential grafting can make the surgery simpler and use fewer grafts.
- Multiple grafting can cover more areas, which is good for severe disease.
Choosing between these methods depends on the patient’s health and the surgeon’s skills.
Off-Pump vs. On-Pump CABG Techniques
CABG surgeries are divided into off-pump and on-pump types. Off-pump CABG is done on a beating heart without a bypass. On-pump CABG uses a bypass to keep blood flowing during the surgery.
Indications for Off-Pump CABG
Off-pump CABG is chosen for patients with certain risks. These include:
- Patients with severe atherosclerosis of the aorta
- Those with a history of stroke or significant carotid disease
- Patients with renal insufficiency or other comorbid conditions
Surgeons pick off-pump CABG for those at high risk from the bypass.
Stabilization Techniques for Beating Heart Surgery
Stabilizing the heart during off-pump CABG is a big challenge. To solve this, several techniques and devices have been created:
- Mechanical stabilizers that immobilize the heart area where the graft is attached
- Intracoronary shunts to keep blood flowing through the coronary artery during the anastomosis
These tools help surgeons do off-pump CABG safely and precisely.
Comparative Outcomes and Selection Criteria
Choosing between off-pump and on-pump CABG depends on many factors. These include patient selection, surgeon experience, and what the hospital prefers. Studies show both methods can work well, but the best choice varies by patient:
“The choice between off-pump and on-pump CABG should be based on a thorough look at the patient’s risk and the surgeon’s skill.”
— Journal of Cardiac Surgery
Important factors include the patient’s health, the complexity of their heart disease, and the surgeon’s experience with both methods.
In summary, both off-pump and on-pump CABG have roles in heart surgery. The right choice depends on careful patient selection and understanding the benefits and drawbacks of each method.
Managing Complications During CABG Surgery
Managing complications during CABG surgery is key to keeping patients safe and improving outcomes. CABG is a top treatment for coronary artery disease but comes with risks. We tackle these risks with careful planning, precise techniques, and quick action when needed.
Bleeding Control and Management
Bleeding is a big worry during CABG surgery. It can lead to serious problems if not handled right away. We use several methods to control bleeding, like careful surgery, special agents, and watching the patient’s blood clotting.
| Strategy | Description | Benefits |
| Meticulous Surgical Technique | Careful handling of tissues and precise suturing | Reduces risk of bleeding |
| Hemostatic Agents | Use of agents like Surgicel or Tisseel | Promotes clot formation |
| Coagulation Monitoring | Regular assessment of coagulation parameters | Enables timely intervention |
Addressing Hemodynamic Instability
Hemodynamic instability can happen for many reasons during CABG surgery. This includes bleeding, heart problems, or issues with anesthesia. We keep a close eye on the patient’s heart and blood pressure. We also use medicines and fluids to keep them stable.
Graft Failure Recognition and Intervention
Graft failure is a serious issue that can happen during or after CABG surgery. We watch the graft closely to catch any problems early. If the graft fails, we act fast. This might mean fixing the graft or using a different one.
In summary, handling complications during CABG surgery needs a team effort. Knowing the risks and having plans to deal with them helps us give our patients the best care possible.
Conclusion: Postoperative Care and Long-Term Outcomes
After a coronary artery bypass graft (CABG) procedure, postoperative care is key. It affects how well a patient does after surgery. We stress the need for full care, like watching over patients in the ICU, managing pain well, and setting up rehab plans that fit each patient.
The success of CABG surgery depends on many things. These include how well the graft works and if patients follow health advice. Also, managing other health issues is important for the best long-term results.
Knowing about CABG and what it means helps patients follow doctor’s orders better. This leads to better long-term health. By focusing on care after surgery and long-term management, we can greatly improve patients’ lives after CABG.
FAQ
What is a Coronary Artery Bypass Graft (CABG) procedure?
A CABG procedure is a surgery that helps the heart by bypassing blocked arteries. It treats coronary artery disease.
What is the purpose of a bypass graft procedure?
The goal of a bypass graft procedure is to improve blood flow to the heart. It helps reduce chest pain and shortness of breath. It also lowers the risk of heart attacks.
What does CABG stand for?
CABG stands for Coronary Artery Bypass Grafting. It’s a surgery that grafts a healthy blood vessel onto a blocked artery.
Is CABG considered open-heart surgery?
Yes, CABG is open-heart surgery. It involves opening the chest to access the heart.
What is the difference between on-pump and off-pump CABG?
On-pump CABG uses a heart-lung machine to circulate blood. Off-pump CABG is done on a beating heart without a machine.
What are the risks associated with CABG surgery?
Risks of CABG surgery include bleeding, infection, and graft failure. Hemodynamic instability is also a risk.
How is patient selection done for CABG surgery?
Choosing patients for CABG involves a detailed preoperative assessment. This includes coronary angiography and risk stratification. It helps decide if the patient is a good candidate for the surgery.
What is the role of informed consent in CABG surgery?
Informed consent is key in CABG surgery. It ensures patients know the risks, benefits, and alternatives. This helps them make an informed choice.
What is cardioplegia administration during CABG surgery?
Cardioplegia administration stops the heart from beating. It reduces metabolic activity and protects the heart during surgery.
What are the long-term outcomes after CABG surgery?
Long-term outcomes after CABG surgery include better survival rates and reduced symptoms. Quality of life improves. But, outcomes can vary based on patient health and lifestyle changes.
References
- Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312