Last Updated on November 25, 2025 by Ugurkan Demir
Choosing the right anticoagulant medication is key for heart health and preventing strokes. At Liv Hospital, we guide you with care, helping you understand your options.
Blood thinners, or anticoagulants and antiplatelet agents, are vital. They help lower the risk of deadly blood clots in people with heart issues and deep vein thrombosis.
We’ll look at the top 20 anticoagulant medications. You’ll learn their names, brands, and how they stack up. Knowing the different blood thinners is key to making smart choices for your health.
Key Takeaways
- Understanding the different types of blood thinners is vital for heart health.
- Anticoagulants and antiplatelet agents prevent blood clots in specific conditions.
- Liv Hospital offers expert care and guidance for those needing blood thinners.
- The top 20 anticoagulant medications will be discussed, including their names, brands, and comparisons.
- Making informed decisions about your care is essential for optimal health outcomes.
What Blood Thinners Are and How They Work
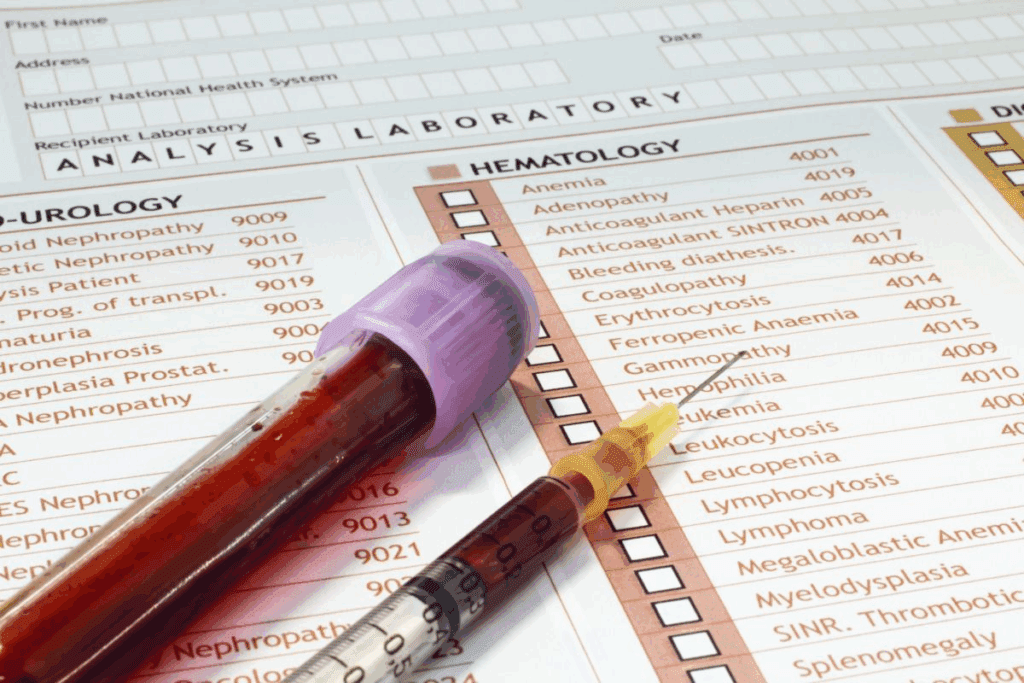
Blood thinners, also known as anticoagulants and antiplatelet agents, help prevent blood clots. They are important for managing conditions that could lead to serious health problems. These include heart attacks and strokes.
Definition and Purpose of Anticoagulants and Antiplatelet Medications
Anticoagulants and antiplatelet agents are two types of blood thinners. They work differently but share the same goal: stopping blood clots. Anticoagulants stop blood clots from forming. Antiplatelet agents stop platelets from clumping together.
These medications are key to keeping the heart healthy. They prevent blood clots that can block blood flow to important organs. This reduces the risk of heart attacks and strokes.
The Blood Clotting Process
The blood clotting process is complex. It starts with an injury to a blood vessel. This injury activates platelets and starts the coagulation cascade. The result is a fibrin clot that seals the injured vessel.
Knowing how blood clots form helps us understand how blood thinners work. The clotting process involves chemical reactions that lead to clot formation. Blood thinners interrupt these reactions to prevent clotting.
Medical Conditions Requiring Blood Thinners
Blood thinners are used for conditions that raise the risk of blood clots. These include atrial fibrillation, deep vein thrombosis (DVT), pulmonary embolism, and mechanical heart valves. Patients with these conditions are at higher risk of serious health problems.
Blood thinners play a vital role in managing these conditions. They prevent blood clots and reduce the risk of complications. The right blood thinner depends on the condition, the patient’s health, and other factors.
Types of Blood Thinners: Anticoagulants vs. Antiplatelet Agents

There are two main types of medications to prevent blood clots: anticoagulants and antiplatelet agents. Knowing the difference between them is key to managing heart conditions well.
Anticoagulants: Preventing Clot Formation
Anticoagulants stop blood clots from forming or growing. They are for people with heart issues like atrial fibrillation or those with mechanical heart valves. These drugs block the coagulation process, lowering clot risk. Examples include warfarin, apixaban, and rivaroxaban.
Antiplatelet Agents: Preventing Platelet Aggregation
Antiplatelet agents, by contrast, stop platelets from clumping together. They are for those with atherosclerosis or who have had heart attacks or strokes. Aspirin is a well-known example, along with clopidogrel and ticagrelor.
Key Differences in Mechanism and Clinical Applications
Anticoagulants and antiplatelet agents work differently. Anticoagulants block the coagulation process, while antiplatelet agents prevent platelet clumping. This difference is important for choosing the right medication for a patient’s needs.
| Characteristics | Anticoagulants | Antiplatelet Agents |
| Mechanism of Action | Inhibit coagulation cascade | Prevent platelet aggregation |
| Primary Conditions Treated | Atrial fibrillation, venous thromboembolism, mechanical heart valves | Atherosclerosis, history of heart attack or stroke |
| Examples | Warfarin, apixaban, rivaroxaban | Aspirin, clopidogrel, ticagrelor |
The 20 Most Popular Blood Thinners in the United States
Knowing the most popular blood thinners in the U.S. is key for doctors and patients. The choice of anticoagulants and antiplatelet agents is complex. It depends on how well they work, how safe they are, and the patient’s health.
Overview of Prescription Trends
Top anticoagulant drugs globally include warfarin (Coumadin), apixaban (Eliquis), and rivaroxaban (Xarelto). These drugs lead in preventing blood clots. Their popularity shows they are effective.
Some trends in prescriptions are:
- More use of Direct Oral Anticoagulants (DOACs) because they are easy to use and don’t need constant checks.
- Warfarin is also used for some patients.
- There’s a preference for drugs taken once a day, like rivaroxaban.
Factors Influencing Medication Selection
Choosing a blood thinner depends on several things. These include the patient’s health history, the condition being treated, and the risk of bleeding. For example:
- Patients with atrial fibrillation might get DOACs like apixaban or dabigatran.
- Those having surgery might get low molecular weight heparins like enoxaparin.
- Patients with deep vein thrombosis might be treated with rivaroxaban or edoxaban.
Evolution of Blood Thinner Usage Over Time
The use of blood thinners has changed a lot over time. DOACs have changed anticoagulant therapy. They offer safer and easier options than traditional drugs like warfarin.
Key developments include:
- New anticoagulants with better safety.
- More use of anticoagulants in different patients.
- Advances in reversing DOACs, making them safer.
As we learn more about blood thinners, prescriptions will likely change. This will help improve patient care.
Traditional Anticoagulants: Vitamin K Antagonists and Heparins
Vitamin K antagonists and heparins are key in preventing and treating blood clots. They have been used for many years. Their safety and effectiveness are well-known in medical practice.
Warfarin (Coumadin): The Long-Standing Standard
Warfarin is a vitamin K blocker that stops the liver from making certain clotting factors. It’s used to prevent and treat blood clots. This is true for people with heart problems and blood clots in the veins.
Key characteristics of warfarin include:
- Narrow therapeutic index, requiring regular INR monitoring
- Dietary restrictions due to vitamin K interactions
- Potential for numerous drug interactions
Unfractionated Heparin: Hospital-Based Treatment
Unfractionated heparin (UFH) is fast-acting and used in hospitals for blood clots. It works by boosting antithrombin, which stops clotting factors.
Advantages of UFH include:
- Rapid onset of action
- Reversibility with protamine sulfate
- Effective in a wide range of clinical scenarios
Enoxaparin (Lovenox): Low Molecular Weight Heparin
Enoxaparin is a low molecular weight heparin (LMWH) with a more stable effect. It’s used to prevent and treat blood clots in the legs and lungs. It’s also used during surgeries.
Benefits of enoxaparin include:
- Predictable pharmacokinetics, reducing the need for routine monitoring
- Subcutaneous administration
- Effective for both prophylaxis and treatment of thromboembolic events
Dalteparin (Fragmin): Oncology Applications
Dalteparin is a LMWH studied in cancer patients. It helps prevent blood clots in cancer patients. It may also improve survival in some cancers.
| Anticoagulant | Mechanism of Action | Primary Uses | Monitoring Requirements |
| Warfarin | Vitamin K antagonist | Atrial fibrillation, mechanical heart valves, VTE | Regular INR monitoring |
| Unfractionated Heparin | Antithrombin enhancement | Acute VTE, surgical anticoagulation | aPTT monitoring |
| Enoxaparin | Factor Xa inhibition | VTE prophylaxis and treatment | Generally not required |
| Dalteparin | Factor Xa inhibition | VTE prophylaxis in cancer patients | Generally not required |
Direct Oral Anticoagulants (DOACs): Factor Xa Inhibitors
DOACs, like apixaban and rivaroxaban, make managing blood thinners easier than old methods. They are key in treating blood clots and need less monitoring.
Apixaban (Eliquis): Features and Benefits
Apixaban is a Factor Xa inhibitor for preventing strokes in people with atrial fibrillation. It’s also used for treating deep vein thrombosis and pulmonary embolism. It’s taken twice a day, making it easy to stick to.
Studies show apixaban has less bleeding risk than warfarin.
Rivaroxaban (Xarelto): Once-Daily Dosing Advantage
Rivaroxaban is a Factor Xa inhibitor taken once a day in some cases. It’s good for preventing strokes, treating blood clots, and preventing clots after surgery. It’s easy for patients to follow.
Edoxaban (Savaysa): Clinical Applications
Edoxaban is a once-daily Factor Xa inhibitor for preventing strokes and treating blood clots. It works as well as warfarin but with fewer food restrictions and less monitoring.
Betrixaban (Bevyxxa): Extended-Duration Prophylaxis
Betrixaban is for long-term prevention of blood clots in sick patients. It’s taken once a day without the need for constant blood tests.
To understand the differences and similarities among these DOACs, let’s look at their key features in the table below:
| DOAC | Dosing Frequency | Primary Indications | Bleeding Risk |
| Apixaban (Eliquis) | Twice daily | Stroke prevention in AFib, DVT/PE treatment | Lower compared to warfarin |
| Rivaroxaban (Xarelto) | Once or twice daily, depending on indication | Stroke prevention in AFib, DVT/PE treatment, thromboprophylaxis in orthopedic surgery | Variable, generally comparable to warfarin |
| Edoxaban (Savaysa) | Once daily | Stroke prevention in AFib, DVT/PE treatment | Generally lower than warfarin |
| Betrixaban (Bevyxxa) | Once daily | Extended-duration thromboprophylaxis in acutely ill medical patients | Higher risk of bleeding compared to enoxaparin |
DOACs have similarities but also unique features and uses. The right choice depends on the patient’s health, medications, and risk of bleeding or stroke.
Direct Thrombin Inhibitors
Direct thrombin inhibitors are a big step forward in fighting blood clots. They work by stopping thrombin, a key player in blood clotting. This makes them more reliable than older treatments.
Dabigatran (Pradaxa): The First DOAC
Dabigatran, or Pradaxa, was the first DOAC to hit the market. It’s used to prevent strokes in people with atrial fibrillation and to treat and prevent blood clots.
Key benefits of dabigatran include:
- Predictable anticoagulant effect without the need for regular monitoring
- Reduced risk of intracranial hemorrhage compared to warfarin
- Convenient oral administration
Argatroban: For Heparin-Induced Thrombocytopenia
Argatroban is a direct thrombin inhibitor for treating heparin-induced thrombocytopenia (HIT). It’s given through an IV and checked with aPTT.
“Argatroban provides a critical alternative for patients with HIT, where other anticoagulants may be contraindicated.” –
Clinical Guidelines for HIT Management
Bivalirudin (Angiomax): Interventional Cardiology Uses
Bivalirudin, or Angiomax, is for heart procedures like PCI. It has a quick and reversible effect, making it safer for these procedures.
Advantages of bivalirudin in PCI include:
| Feature | Benefit |
| Direct thrombin inhibition | Rapid onset of action |
| Reversible effect | Improved safety profile |
| Reduced risk of bleeding | Potential for better outcomes |
Desirudin (Iprivask): Orthopedic Surgery Applications
Desirudin, or Iprivask, is for preventing DVT in hip surgery patients. It’s given under the skin and has shown to cut down on blood clot risks.
In conclusion, direct thrombin inhibitors are a valuable group of anticoagulants. They have many uses thanks to dabigatran, argatroban, bivalirudin, and desirudin. Knowing their benefits helps doctors choose the right treatment for each patient.
Selective Factor Xa Inhibitors and Other Parenteral Anticoagulants
Selective factor Xa inhibitors are a big step forward in fighting blood clots. They work by targeting specific parts of the blood clotting process. This makes them more effective and safer than older treatments, which can cause more bleeding.
Fondaparinux (Arixtra): Synthetic Pentasaccharide
Fondaparinux is a man-made medicine that stops blood clots from forming. It’s used to prevent and treat blood clots in the legs and lungs. Because it works in a predictable way, doctors don’t need to check blood levels as often.
Key Benefits of Fondaparinux:
- Once-daily dosing regimen
- No requirement for routine coagulation monitoring
- Reduced risk of heparin-induced thrombocytopenia (HIT)
Tinzaparin (Innohep): Once-Daily LMWH
Tinzaparin is a type of low molecular weight heparin given once a day. It helps prevent and treat blood clots in the legs and lungs. It’s also good for people with cancer who are at risk of blood clots. Tinzaparin is safer than some other treatments because it causes less bleeding.
Clinical Applications of Tinzaparin:
| Condition | Dosing Regimen | Monitoring Requirements |
| DVT/PE Treatment | Once daily | Anti-Xa levels (in certain cases) |
| Cancer Patients | Once daily | Clinical monitoring |
| Post-operative Thromboprophylaxis | Once daily | No routine monitoring |
Nadroparin (Fraxiparine): European Alternative
Nadroparin is a low molecular weight heparin used in Europe for preventing and treating blood clots. It comes in different forms and doses, making it flexible for different needs. Nadroparin is effective in preventing blood clots in surgery patients and treating existing clots.
These anticoagulants, including fondaparinux, tinzaparin, and nadroparin, give doctors many options for managing blood clots. Their targeted action and consistent effects make them key tools in preventing and treating blood clots.
Common Antiplatelet Medications
Antiplatelet medications are key for those at risk of heart problems. They stop platelets from sticking together, which helps prevent blood clots.
Aspirin: The Original Antiplatelet
Aspirin is a long-standing choice for heart protection. It blocks a key enzyme, which stops platelets from clumping. This makes it a cornerstone in preventing heart attacks and strokes.
Aspirin’s benefits are:
- It’s affordable and easy to find.
- There’s a lot of research backing its use.
- It’s simple to take.
Clopidogrel (Plavix): P2Y12 Receptor Inhibition
Clopidogrel stops platelets from sticking together by blocking a specific receptor. It’s often given to those with heart attacks or undergoing heart procedures.
Clopidogrel’s advantages are:
- It cuts down on heart problems in heart attack patients.
- It works better when taken with aspirin.
- It’s been studied a lot and is considered safe.
Ticagrelor (Brilinta): Reversible Binding Properties
Ticagrelor is a newer option that works fast and doesn’t stick around as long as clopidogrel. It’s for people with heart attacks to prevent more problems.
Ticagrelor’s notable features are:
- It starts working quickly and stops just as fast.
- It might be more effective for some patients.
- It needs to be taken twice a day.
Prasugrel (Effient): Potent Platelet Inhibition
Prasugrel is another strong option for heart attack patients. It blocks platelet receptors for a long time. It’s used for those getting heart procedures.
Prasugrel’s key traits are:
- It stops platelets from sticking together more effectively than clopidogrel.
- It helps prevent heart problems.
- It can increase the risk of bleeding.
In summary, these medications are essential for heart health. Knowing how they work and their benefits and risks helps doctors care for their patients better.
Specialized and Newer Antiplatelet Agents
The world of antiplatelet therapy is changing with new agents. These drugs have unique ways of working and are used in certain situations to stop blood clots.
Dipyridamole (Persantine and Aggrenox)
Dipyridamole stops platelets from sticking together. It’s often paired with aspirin in Aggrenox. This combo is used to prevent strokes.
Ticlopidine (Ticlid): First-Generation Thienopyridine
Ticlopidine was a big step forward in fighting blood clots. Even though newer drugs like clopidogrel are preferred, it’s part of antiplatelet history.
Vorapaxar (Zontivity): PAR-1 Antagonist
Vorapaxar blocks a receptor that makes platelets stick together. It helps people who have had heart attacks or artery disease by lowering the risk of more heart problems.
Cilostazol (Pletal): Phosphodiesterase Inhibitor
Cilostazol is a drug that stops platelets from sticking and also widens blood vessels. It’s mainly used to help people with leg pain due to artery disease walk farther.
To understand these newer antiplatelet drugs better, let’s look at how they compare in a table.
| Medication | Mechanism of Action | Primary Indication | Notable Feature |
| Dipyridamole | Inhibits platelet activation and aggregation | Stroke prevention | Often used in combination with aspirin |
| Ticlopidine | Thienopyridine, inhibits ADP receptor | Stroke prevention, coronary stenting | First-generation thienopyridine |
| Vorapaxar | PAR-1 antagonist, inhibits thrombin-induced aggregation | Reducing thrombotic cardiovascular events | Unique mechanism targeting PAR-1 |
| Cilostazol | Phosphodiesterase 3 inhibitor | Intermittent claudication | Improves walking distances |
These new antiplatelet drugs are big steps forward in treating blood clotting problems. They give doctors more options to help each patient in their own way.
Comparing Blood Thinners: Efficacy, Safety, and Practical Considerations
Looking at blood thinners is complex. We need to understand their effectiveness, safety, and how easy they are to use. It’s key to look at several important factors when choosing one for treatment.
Bleeding Risk Profiles
When we pick blood thinners, we worry about bleeding risks. Each medicine has its own risk level. For example, warfarin needs regular checks because it can change how it works in different people.
Newer medicines like apixaban and rivaroxaban are more predictable. This might lower the chance of serious bleeding.
A study showed apixaban has less major bleeding than warfarin. But, the risk can change based on the patient, like age or kidney function.
Reversibility Options and Antidotes
Having reversal agents is important when choosing a blood thinner. Warfarin has clear reversal methods using vitamin K and PCC. Newer medicines have specific antidotes: idarucizumab for dabigatran and andexanet alfa for apixaban and rivaroxaban. These help make newer medicines safer.
- Idarucizumab quickly reverses dabigatran‘s effects.
- Andexanet alfa works well to reverse factor Xa inhibitors, but it’s more complex.
Drug Interactions and Dietary Restrictions
Blood thinners can interact with other drugs and foods differently. Warfarin is known for many interactions, mainly with foods high in vitamin K. Newer medicines have fewer interactions, but some, like rivaroxaban, need caution with certain drugs.
Dietary rules also vary. Warfarin needs a steady intake of vitamin K foods. But DOACs don’t have specific food rules, making them easier for patients.
Monitoring Requirements and Convenience
Monitoring needs differ among blood thinners. Warfarin needs regular INR checks. But most DOACs don’t need these checks, making them more convenient and helping patients stick to their treatment.
Yet, some patients, like those with kidney problems or very high or low body weight, might need drug level checks, even with DOACs.
Conclusion: The Future of Blood Thinners
The market for blood thinners is changing fast. New trends and medicines are coming out. This means we have more options for treating different health issues.
New medicines like direct oral anticoagulants (DOACs) are making a big difference. They work better and are safer. This is good news for the future of blood thinners.
More research and new medicines are on the way. This will help doctors and patients find the best treatments. Keeping up with these changes will help us all get better care.
FAQ
What are blood thinners, and how do they work?
Blood thinners stop blood clots from forming or growing. They work by blocking the blood’s ability to clot. This is done by stopping the production of clotting factors or preventing platelets from sticking together.
What are the different types of blood thinners?
Blood thinners are divided into two main types. Anticoagulants, like warfarin and apixaban, stop clotting by blocking clotting factors. Antiplatelet agents, such as aspirin and clopidogrel, stop platelets from sticking together.
What are the most common blood thinners?
Common blood thinners include warfarin (Coumadin), apixaban (Eliquis), and rivaroxaban (Xarelto). Aspirin and clopidogrel (Plavix) are also widely used.
What are the names of some popular blood thinner brands?
Well-known brands include Coumadin (warfarin), Eliquis (apixaban), and Xarelto (rivaroxaban). Plavix (clopidogrel) and Pradaxa (dabigatran) are also popular.
What are the top blood thinners used in the United States?
In the U.S., the most used blood thinners are warfarin, apixaban, and rivaroxaban. Dabigatran and aspirin are also common.
How do Direct Oral Anticoagulants (DOACs) work?
DOACs, like apixaban and rivaroxaban, directly block specific clotting factors. This includes factor Xa.
What are the benefits of using DOACs?
DOACs have several benefits. They reduce bleeding risks, have fewer dietary restrictions, and need less monitoring than traditional anticoagulants like warfarin.
What are the risks associated with blood thinners?
Blood thinners can increase bleeding risks. Some may also interact with other medications or have dietary restrictions.
How are blood thinners monitored?
Some, like warfarin, need regular blood tests to check clotting levels. Others, like DOACs, don’t require regular monitoring.
Can blood thinners be used long-term?
Yes, many blood thinners are safe for long-term use. The decision depends on the patient’s health and medical conditions.
Are there any new developments in blood thinner medications?
Yes, researchers are always working on new blood thinners. These aim to be safer and more effective.
What is the most popular blood thinner?
The most popular blood thinner varies by medical condition. Warfarin and apixaban are often prescribed.
What are some common antiplatelet medications?
Common antiplatelet medications include aspirin, clopidogrel, ticagrelor, and prasugrel.
How do antiplatelet medications work?
Antiplatelet medications stop platelets from sticking together. This is key in preventing blood clots.
What are the differences between anticoagulants and antiplatelet agents?
Anticoagulants stop clotting by blocking clotting factors. Antiplatelet agents prevent platelets from sticking together.
References
- Chaudhry, R. (2022). Physiology, Cardiovascular. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK493197/