Last Updated on December 4, 2025 by Ugurkan Demir

Knowing which blood thinner drugs doctors often use is key. At Liv Hospital, we focus on your safety. We make sure you get the best anticoagulant medications out there.
Conditions like atrial fibrillation and deep vein thrombosis need careful handling. Common anticoagulant medications are vital in stopping these clots and strokes. We’ll look at top anticoagulant list of drugs, like warfarin, enoxaparin, and dabigatran.
Key Takeaways
- Anticoagulant medications are key in stopping blood clots in many health issues.
- Liv Hospital puts patients first in managing blood clot risks.
- Warfarin, enoxaparin, and dabigatran are often prescribed.
- It’s important to know the different anticoagulant types for good management.
- At Liv Hospital, getting you the safest and most effective drugs is our top goal.
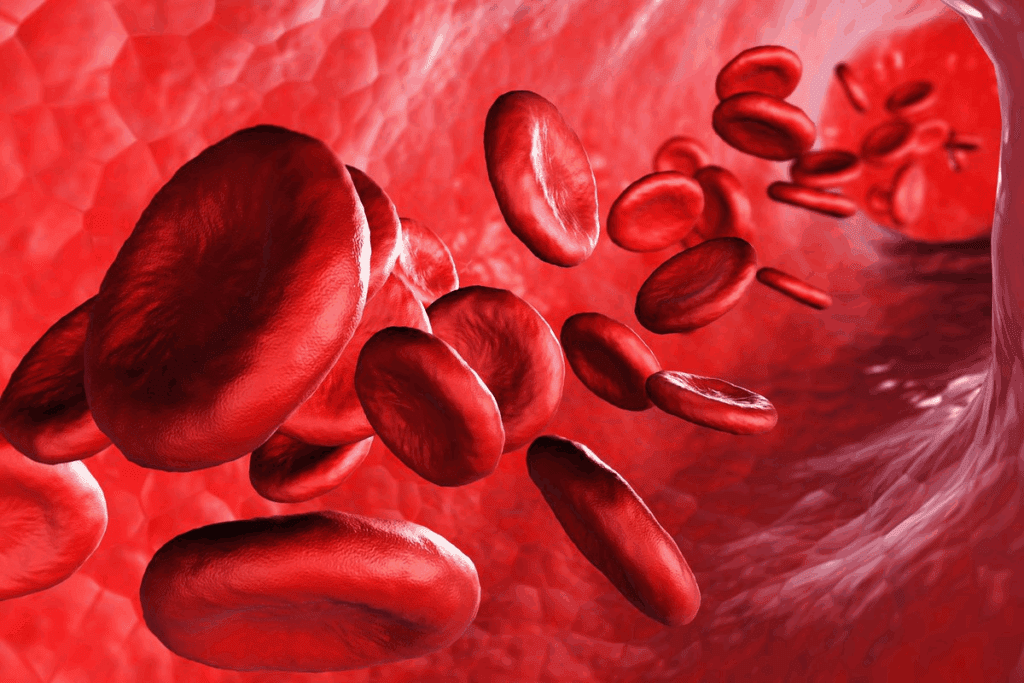
Understanding Blood Thinners in Modern Medicine

Blood thinners are key in modern medicine. They help prevent and treat heart conditions. These medicines improve patient outcomes and quality of life.
The Science Behind Anticoagulation Therapy
Anticoagulation therapy uses medicines to stop blood clots. Anticoagulants block the steps that lead to clotting. This reduces the risk of blood clots.
The coagulation cascade has three main pathways. Anticoagulants target these pathways. For example, warfarin stops certain clotting factors. Dabigatran and rivaroxaban directly block clotting factors.
Medical Conditions Requiring Blood Thinners
Blood thinners are used for conditions that raise clot risk. These include atrial fibrillation, DVT, PE, and mechanical heart valves. In atrial fibrillation, they prevent stroke by stopping heart clots.
Those with DVT or PE take anticoagulants to avoid future clots. The treatment length depends on the cause and risk factors. People with mechanical heart valves need lifelong treatment to avoid valve problems.
The Evolution of Anticoagulant Medications
Anticoagulant therapy has changed a lot over time. Old medicines like warfarin and heparin need regular checks. Newer medicines, called DOACs, offer better options.
DOACs, like dabigatran and rivaroxaban, are easier to use. They don’t need constant monitoring. This makes treatment simpler for patients and doctors.
12 Common Anticoagulant Examples and Their Classifications
Anticoagulant therapy has grown a lot, giving many choices for patients. We’ll look at different types of anticoagulants, how they are given, and why they are chosen for certain health issues.
Overview of Major Anticoagulant Classes
Anticoagulants fall into several main groups based on how they work. These include vitamin K antagonists, low molecular weight heparins, and direct oral anticoagulants. Each group has its own benefits and uses.
Vitamin K antagonists, like warfarin, have been around for a long time. But, they need regular checks because their effect can be too narrow. On the other hand, direct oral anticoagulants (DOACs) like apixaban and rivaroxaban offer steady protection without needing constant monitoring.
Prescription vs. Over-the-Counter Options
Most anticoagulants need a doctor’s prescription because of their side effects and interactions with other drugs. Prescription anticoagulants include warfarin, enoxaparin, dabigatran, apixaban, rivaroxaban, and edoxaban. There are no over-the-counter anticoagulants approved for long-term use.
But, some anticoagulants, like aspirin, are sold without a prescription. Yet, aspirin works differently by preventing platelets from sticking together, not by acting as a traditional anticoagulant.
Parenteral vs. Oral Anticoagulants
Anticoagulants can be given either by injection or orally. Parenteral anticoagulants, such as heparin and low molecular weight heparins, are used in urgent situations or for those who can’t take pills.
Oral anticoagulants, including warfarin and the newer DOACs, are better for long-term use. They are easier for patients to take and stick to.
Selecting the Right Anticoagulant for Specific Conditions
Choosing the right anticoagulant depends on several things. These include the patient’s health, kidney function, risk of bleeding, and drug interactions. For example, DOACs like apixaban or rivaroxaban are often chosen for patients with atrial fibrillation because they have a good balance of benefits and risks.
For patients having surgery, low molecular weight heparins or fondaparinux are often used to prevent blood clots. The table below shows some common anticoagulants and their usual uses:
| Anticoagulant Class | Examples | Common Indications |
| Vitamin K Antagonists | Warfarin | Atrial fibrillation, mechanical heart valves |
| Low Molecular Weight Heparins | Enoxaparin, Dalteparin | DVT prophylaxis, acute coronary syndromes |
| Direct Oral Anticoagulants (DOACs) | Apixaban, Rivaroxaban, Dabigatran | Atrial fibrillation, DVT/PE treatment |
| Parenteral Anticoagulants | Heparin, Fondaparinux | Acute thrombosis, surgical prophylaxis |
The world of anticoagulant therapy is complex and varied. Knowing about these categories and their uses is key for doctors to make the best choices.
“The introduction of new anticoagulants has significantly impacted the management of thromboembolic disorders, giving more options for patients and doctors alike.”
Vitamin K Antagonists: The Traditional Blood Thinners
Vitamin K antagonists have been used for decades to prevent blood clots. They work by stopping the liver from making clotting factors. This prevents blood clots from forming.
Warfarin (Coumadin, Jantoven)
Warfarin, also known as Coumadin, is a key blood thinner. It’s used to stop deep vein thrombosis, pulmonary embolism, and stroke in people with atrial fibrillation.
Key characteristics of warfarin include:
- Narrow therapeutic index, requiring regular monitoring of INR (International Normalized Ratio)
- Dietary interactions, with foods high in vitamin K
- Potential for numerous drug interactions
Blood Thinners Starting with “C”: Coumadin and Its History
Coumadin, the brand name for warfarin, has a long history. It was first used in the 1940s as a rodenticide. Later, it was used for humans, marking a big step in treating blood clots.
Other Vitamin K Antagonists in Clinical Use
Warfarin is the most used vitamin K antagonist, but others like acenocoumarol and phenindione are also used. They work in a similar way but have different effects on the body.
| Drug Name | Half-life | Common Brand Names |
| Warfarin | 20-60 hours | Coumadin, Jantoven |
| Acenocoumarol | 8-11 hours | Sinthrome, Sintrom |
| Phenindione | 5-10 hours | Dindevan, Pindione |
The choice of vitamin K antagonist depends on the patient, what’s available, and doctor guidelines.
Unfractionated Heparin and Its Brand Names
Unfractionated heparin is key in fighting blood clots. It’s given by injection and comes under different names.
Heparin Sodium: The Original Injectable Anticoagulant
Heparin sodium is a top choice for stopping blood clots. It’s been around for years and works well in hospitals.
Hepalean and Other Unfractionated Heparin Brand Names
Unfractionated heparin is known by names like Hepalean and Heparin Sodium. These names change based on where you are.
Monitoring Parameters and Dosage Adjustments
Using unfractionated heparin needs close watch because it’s tricky. APTT tests help check if it’s working right. If not, doctors adjust the dose to avoid bleeding.
| Monitoring Parameter | Target Range | Action for Out-of-Range Values |
| aPTT | 1.5-2.5 times control | Adjust heparin dose; consult protocol |
| Hemoglobin/Hematocrit | Within normal limits | Investigate signs of bleeding |
Heparin-Induced Thrombocytopenia Concerns
Heparin can cause a serious problem called HIT. It’s important to watch platelet counts. A big drop means HIT might be happening.
Low Molecular Weight Heparins in Clinical Practice
Low molecular weight heparins (LMWHs) have changed how we prevent and treat blood clots. They are safer and more effective than traditional heparin. This makes them a key part of modern medicine.
Enoxaparin (Lovenox): The Most Widely Used LMWH
Enoxaparin is a top choice for preventing and treating blood clots. It’s known for its easy use and low risk of side effects. This makes it a favorite among doctors and patients alike.
Key benefits of enoxaparin include:
- Reliable anticoagulation with a single daily dose
- Reduced risk of heparin-induced thrombocytopenia (HIT)
- Effective in both prophylactic and therapeutic settings
Dalteparin (Fragmin): Applications in Oncology
Dalteparin is also widely used, but it shines in cancer treatment. It helps prevent blood clots and may even help patients live longer.
Clinical studies have demonstrated that dalteparin can improve outcomes in certain cancer patients by reducing the risk of thromboembolic complications and potentially influencing tumor progression.
Other LMWHs and Their Specific Indications
Other LMWHs like tinzaparin and nadroparin also have their uses. Each has its own role in treating blood clots. The right choice depends on the patient’s needs and health.
The choice of LMWH depends on various factors, including the patient’s clinical condition, renal function, and the specific thrombotic risk profile.
Monitoring Considerations for LMWH Therapy
LMWHs are known for their predictable effect, making monitoring less common. But, some patients might need their levels checked to make sure they’re getting the right dose.
Monitoring is recommended for patients with kidney problems, obesity, or who are pregnant. It’s also important for kids to ensure they’re getting the best treatment.
By understanding how to use LMWHs, we can improve patient care. This helps reduce the risk of blood clots and improves health outcomes.
Direct Thrombin Inhibitors: Targeted Anticoagulation
Direct thrombin inhibitors are a big step forward in fighting blood clots. They target thrombin, a key player in blood clotting, without needing other helpers. This makes them a more precise way to prevent clots.
Dabigatran: The First Approved Oral Direct Thrombin Inhibitor
Dabigatran, sold as Pradaxa, was the first oral direct thrombin inhibitor approved. It’s great at stopping strokes and blood clots in people with a certain heart rhythm problem. It’s better than older treatments because it’s easier to use and doesn’t need constant checks.
Argatroban: A Solution for Heparin-Allergic Patients
Argatroban is a direct thrombin inhibitor for those allergic to heparin. It’s a safe choice for patients who can’t take heparin. It works well even when other treatments don’t because it doesn’t rely on antithrombin.
Bivalirudin: Use in Acute Coronary Syndromes
Bivalirudin, or Angiomax, is used in heart procedures and emergencies. It’s good because it works well and doesn’t last too long in the body. This makes it perfect for use in urgent situations.
Comparing Direct Thrombin Inhibitors to Traditional Anticoagulants
Direct thrombin inhibitors have big advantages over older treatments. They’re more reliable, need less monitoring, and interact less with other drugs. But, they also have challenges, like not having a quick fix to reverse their effects (except for dabigatran).
Choosing between direct thrombin inhibitors and traditional anticoagulants depends on the situation. Each patient is different, and the right choice depends on their health, risk of bleeding, and what other medicines they take.
Factor Xa Inhibitors: Modern Anticoagulant Options
Factor Xa inhibitors are a big step forward in fighting blood clots. They work better and are safer than older treatments.
Apixaban (Eliquis): Balanced Efficacy and Safety Profile
Apixaban, or Eliquis, is a top choice for blood clot prevention. It’s known for being safe and effective. Studies show it lowers stroke risk in people with atrial fibrillation.
Apixaban is taken twice a day, which helps patients stick to their treatment. It also has a lower risk of serious bleeding, making it safer.
Rivaroxaban (Xarelto): Once-Daily Dosing Advantage
Rivaroxaban, or Xarelto, is another popular option. It’s taken once a day, making it easier for patients. It prevents blood clots and is used to stop strokes in atrial fibrillation patients.
Rivaroxaban’s steady effect makes it reliable for long-term use. But, it’s important to watch for bleeding signs.
Edoxaban (Savaysa, Lixiana): Newer Factor Xa Inhibitor
Edoxaban, known as Savaysa in the US and Lixiana elsewhere, is a newer choice. It’s known for being safe and effective. Edoxaban is taken once a day and is as good as warfarin in preventing strokes.
Edoxaban is safer than warfarin, which is good for those at risk of bleeding.
Fondaparinux (Arixtra): The Synthetic Pentasaccharide
Fondaparinux, or Arixtra, is a synthetic drug that acts like a factor Xa inhibitor. It’s used to prevent and treat blood clots. Fondaparinux works by blocking factor Xa without affecting thrombin.
Fondaparinux is given by injection, mainly in hospitals for surgery patients. Its predictable action means no need for constant blood tests.
In summary, factor Xa inhibitors like apixaban, rivaroxaban, edoxaban, and fondaparinux are big steps forward. They offer easy dosing and are safer, making them great for long-term treatment.
Clinical Management of Patients on Anticoagulant Therapy
Managing patients on anticoagulant therapy is key to avoiding blood clots and bleeding. Anticoagulants are vital for treating heart conditions like atrial fibrillation and blood clots in veins and lungs.
Initiating and Transitioning Between Anticoagulants
Starting anticoagulant therapy requires careful thought. Doctors must consider the patient’s kidney and liver health and any drug interactions. Sometimes, patients need to switch anticoagulants due to health changes or surgery.
For example, a patient on warfarin might switch to a direct oral anticoagulant (DOAC) if INR levels are hard to manage. On the other hand, a DOAC user might switch to warfarin for surgeries that need easy reversal.
| Anticoagulant | Transition Strategy | Key Considerations |
| Warfarin to DOAC | Stop warfarin when INR | Monitor INR during transition |
| DOAC to Warfarin | Start warfarin and continue DOAC until INR is therapeutic | Overlap therapy to ensure adequate anticoagulation |
Managing Bleeding Complications
Dealing with bleeding in patients on anticoagulants needs quick action. The bleeding’s severity guides the treatment, from stopping the drug to using reversal agents.
Minor Bleeding: Minor issues like nosebleeds or bruises might just need local care and a break from the drug.
Major Bleeding: Severe bleeding calls for immediate action. This includes stopping the drug, considering reversal agents, and giving supportive care.
Reversal Agents and Antidotes
Reversal agents have greatly improved managing bleeding from anticoagulants. For example, idarucizumab reverses dabigatran, and andexanet alfa works for factor Xa inhibitors.
Perioperative Management Strategies
Managing patients on anticoagulants before surgery is complex. It’s about weighing the risk of blood clots against bleeding risks. Doctors might stop the drug before surgery, use heparin as a bridge, or start it again after surgery.
Each patient needs a tailored approach to reduce risks of blood clots and bleeding during surgery.
Conclusion: Navigating the Complex World of Anticoagulants
Understanding anticoagulants is key to managing blood clotting disorders. We’ve looked at different types, like warfarin (Coumadin, Jantoven) and dabigatran (Pradaxa). We also talked about heparins and newer options.
Choosing the right anticoagulant is important. It depends on the patient’s needs and the risks. New blood thinners are being developed all the time.
Healthcare providers need to know about these medications. This helps them treat patients better. It also reduces risks and improves outcomes.
As we learn more about anticoagulants, keeping up with new drugs is important. This ensures we can give the best care to our patients.
FAQ
What are anticoagulant medications used for?
Anticoagulant medications help prevent blood clots. They also treat clots to lower the risk of stroke and heart attack. This is important for heart health.
What are some common anticoagulant examples?
Some well-known anticoagulants are warfarin (Coumadin), enoxaparin (Lovenox), dabigatran (Pradaxa), apixaban (Eliquis), and rivaroxaban (Xarelto).
How do vitamin K antagonists work?
Vitamin K antagonists, like warfarin, stop the liver from making clotting factors. This makes blood less likely to clot.
What is the difference between unfractionated heparin and low molecular weight heparins?
Unfractionated heparin needs regular blood tests to check its effect. Low molecular weight heparins, like enoxaparin, don’t need as much testing because they work more predictably.
What are direct oral anticoagulants (DOACs)?
DOACs, such as dabigatran, apixaban, and rivaroxaban, directly block clotting factors. They are easier to use and more reliable than older anticoagulants.
How are bleeding complications managed in patients on anticoagulant therapy?
To handle bleeding, doctors first check how bad it is. Then, they might stop or reverse the anticoagulant. They use special drugs to reverse the effect, like idarucizumab for dabigatran.
What are some common brand names of anticoagulant medications?
Well-known brands include Coumadin (warfarin), Lovenox (enoxaparin), Pradaxa (dabigatran), Eliquis (apixaban), and Xarelto (rivaroxaban).
Can anticoagulant medications be used in patients with kidney disease?
Yes, but patients with kidney disease might need their doses adjusted. This is because some medications are cleared by the kidneys.
How are patients transitioned between different anticoagulant medications?
Switching medications requires careful planning. Doctors consider how each medication works to avoid problems like clots or bleeding.
What are some common oral anticoagulants?
Common ones include warfarin (Coumadin), dabigatran (Pradaxa), apixaban (Eliquis), rivaroxaban (Xarelto), and edoxaban (Savaysa, Lixiana).
What is heparin-induced thrombocytopenia?
It’s a serious condition caused by an immune reaction to heparin. It leads to low platelet counts and an increased risk of blood clots.
How are factor Xa inhibitors used in clinical practice?
Factor Xa inhibitors, like apixaban and rivaroxaban, are used to prevent and treat blood clots. They are a convenient and effective choice for many patients.
References
- Lung, K., & Lui, F. (2023). Anatomy, Abdomen and Pelvis: Arteries. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK525959/