When the heart can’t pump blood well, it leads to a serious condition called decompensated heart failure. This happens when heart failure symptoms get so bad that quick medical help is needed to stop things from getting worse.
Heart failure occurs when the heart muscle doesn’t pump blood as it should. This causes blood to back up and fluid to build up in the lungs, leading to shortness of breath. At Liv Hospital, we know how serious this condition is. We offer top-notch treatment with a focus on our patients.
Decompensated heart failure is a serious condition that needs immediate attention. We are committed to delivering world-class healthcare. We also provide full support for our international patients.
Key Takeaways
- Decompensated heart failure is a severe and life-threatening condition.
- It requires immediate medical attention to prevent further deterioration.
- Liv Hospital offers advanced treatment with a patient-focused approach.
- Understanding the causes and symptoms is key for effective treatment.
- Our team is dedicated to providing complete care for international patients.
Understanding Heart Failure Fundamentals
To understand decompensated heart failure, we need to know the basics of heart failure. The heart pumps blood all over the body. It brings oxygen and nutrients to our tissues. This is key for our health.
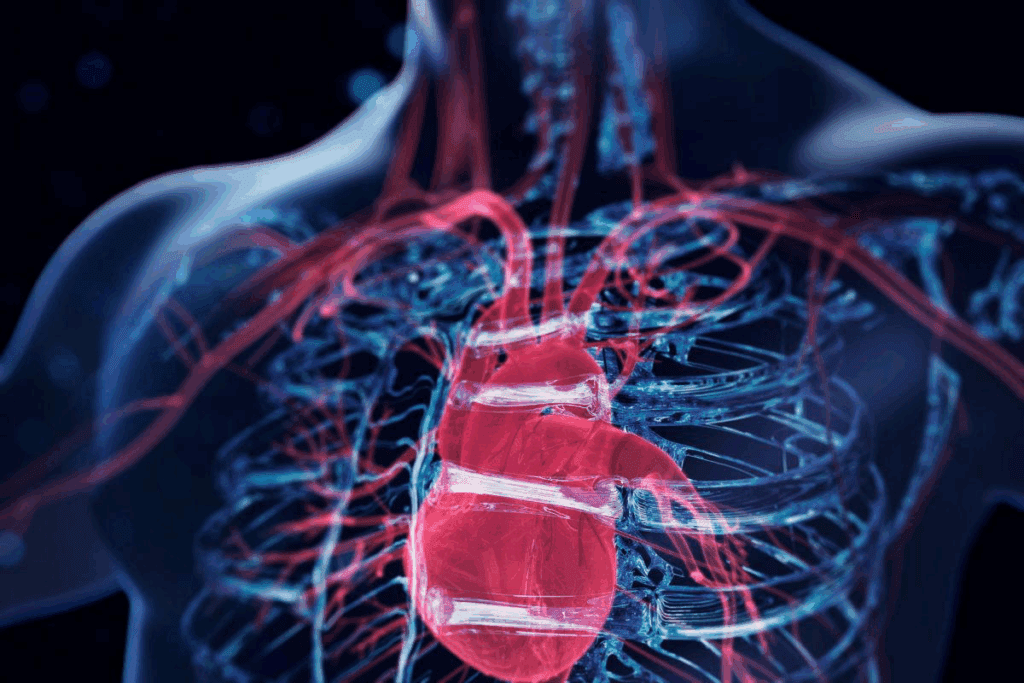
The Normal Heart Function
The heart has two upper chambers (atria) and two lower chambers (ventricles). The atria take in blood, and the ventricles push it out. This teamwork makes sure blood flows well everywhere in the body.
When the heart works right, it pumps enough blood. This meets our body’s need for oxygen and nutrients.
Chronic Heart Failure Overview
Chronic heart failure means the heart can’t pump blood as well. This can happen due to many reasons like heart disease, high blood pressure, diabetes, and valve issues. When the heart can’t pump well, fluid builds up in the lungs and body.
This can cause symptoms like shortness of breath, tiredness, and swollen legs. Knowing these basics is important. They help us understand decompensated heart failure better.
What Decompensated Heart Failure Means
Decompensated heart failure means the heart can’t pump blood well. This is a serious stage of heart failure. It leads to severe symptoms that need quick medical help.
Clinical Definition and Terminology
Decompensated heart failure happens when the heart can’t keep up with its reduced function. It’s marked by symptoms like shortness of breath, tiredness, and swelling. These symptoms mean you need to see a doctor right away.
Doctors use terms like “acute decompensated heart failure” and “chronic decompensated heart failure.” These terms help them tell if symptoms got worse suddenly or gradually.
Difference Between Compensated and Decompensated States
The main difference is how well the heart pumps blood. In compensated heart failure, the heart manages to pump enough blood, even if it’s weak. But in decompensated heart failure, the heart can’t keep up anymore.
Here are the main differences:
- Symptoms: Decompensated heart failure has more severe and sudden symptoms.
- Circulation: The heart can’t pump blood well in decompensated heart failure.
- Urgency: You need to see a doctor right away for decompensated heart failure. Compensated heart failure might need ongoing treatment and checks.
It’s important for doctors and patients to know the difference. This helps get the right care and spot when things are getting worse.
Types of Decompensated Heart Failure
Decompensated heart failure comes in different types, each with its own challenges and treatments. Knowing these types helps healthcare providers give better care and improve patient results.
Acute Decompensated Heart Failure
Acute decompensated heart failure happens suddenly, often needing quick hospital care. It’s a serious situation that needs fast action to keep the patient stable. Symptoms include severe breathing trouble, trouble breathing while lying down, and sudden breathing problems at night.
Chronic Decompensated Heart Failure
Chronic decompensated heart failure gets worse slowly over time. It’s linked to a heart that’s not working as well as it should, even with treatment. Patients may feel more tired, have swelling, and breathe harder, affecting their life quality. We help manage these symptoms and adjust treatments to slow the disease.
Both types of decompensated heart failure need careful management and watching. Knowing the differences helps us tailor care to each patient. This way, we can improve their care and outcomes.
Epidemiology and Impact
It’s important to understand how decompensated heart failure affects people. This condition is a big reason why heart failure patients end up in the hospital.
Prevalence in the United States
In the US, about 6.2 million adults have heart failure. Decompensated heart failure is a main cause of hospital stays for these patients. This shows we need strong healthcare systems to handle these cases.
Hospitalization Rates and Economic Burden
Decompensated heart failure causes a lot of hospital visits. This puts a big strain on healthcare budgets. The costs include hospital stays and ongoing care.
The economic impact gets worse because patients often need to go back to the hospital. They also have to deal with other health issues. Efficient management strategies are key to reducing these costs.
We know decompensated heart failure greatly affects patients’ lives and health outcomes. So, it’s vital to understand its spread to create better care plans.
Recognizing the Signs and Symptoms
It’s key to spot the signs and symptoms of decompensated heart failure early. This condition can come on suddenly or slowly, with different signs that need different treatments.
Acute Symptoms Requiring Immediate Attention
Acute decompensated heart failure shows up with serious and dangerous symptoms. These include:
- Sudden severe shortness of breath, often with coughing up frothy mucus.
- Rapid weight gain from fluid buildup.
- Confusion or altered mental state in severe cases.
Gradual Worsening of Chronic Symptoms
Chronic decompensated heart failure shows up with symptoms that get worse over time. Common signs are:
- Swelling in the legs, ankles, and feet from fluid buildup.
- Getting more tired and weak, making everyday tasks hard.
- Shortness of breath during simple tasks or when lying down.
Keeping an eye on these symptoms is important for managing the condition well.
By knowing and spotting these signs, patients and doctors can better manage decompensated heart failure together.
Pathophysiology of Decompensation in Heart Failure
When heart failure moves from a stable to a decompensated state, it’s due to many changes. At first, the heart tries to keep working by using special tricks. But when these tricks don’t work anymore, the heart’s performance drops a lot.
Failure of Compensatory Mechanisms
The heart uses tricks like beating faster and tightening blood vessels to keep pumping. These tricks work for a while but can hurt the heart more in the long run. For example, beating too fast can weaken the heart, and tightening blood vessels makes it harder for the heart to work.
Key Compensatory Mechanisms and Their Limitations:
| Mechanism | Initial Effect | Long-term Consequence |
| Increased Heart Rate | Maintains cardiac output | Leads to tachycardia-induced cardiomyopathy |
| Vasoconstriction | Maintains blood pressure | Increases afterload, reducing cardiac efficiency |
| Ventricular Hypertrophy | Compensates for increased workload | Can lead to fibrosis and reduced cardiac function |
Neurohormonal Changes During Decompensation
Changes in hormones play a big role in decompensated heart failure. The RAAS and the sympathetic nervous system kick in when the heart can’t pump enough. They help keep blood pressure up and organs getting enough blood, but they also cause more heart damage over time.
“Activation of the renin-angiotensin-aldosterone system and sympathetic nervous system is a double-edged sword in heart failure, providing short-term support but contributing to long-term cardiac damage.”
Understanding these changes is key to managing decompensated heart failure. We need to act fast to stop the heart from getting worse.
It’s important to know how these changes work together. This helps us create better treatments that fix the heart’s problems and symptoms.
Common Triggers and Risk Factors
Many factors can cause decompensated heart failure. It’s important to know these triggers to prevent and manage heart failure well.
Acute Cardiac Events
Events like myocardial infarction can trigger decompensated heart failure. These events put a lot of stress on the heart. Quick medical help is key to lessen the damage.
Other heart events, like arrhythmias and acute coronary syndromes, can also harm the heart. We need to act fast and use the right treatments.
Medication Non-Adherence
Not taking heart medications as directed is a big risk for decompensated heart failure. Telling patients why they must take their meds is a big part of managing heart failure.
- Making medication plans easier can help.
- Seeing doctors regularly can check if patients are taking their meds.
- Helping with the cost of meds is also important.
Infections and Other Non-Cardiac Triggers
Infections like pneumonia and sepsis can also cause heart failure. These infections stress the heart a lot. Getting vaccinated against flu and pneumococcus can help prevent these infections.
“Infections are a major precipitant of acute decompensated heart failure, highlighting the need for preventive measures and prompt treatment.”
Other non-heart triggers include anemia, thyroid issues, and kidney problems. Managing these can help avoid heart failure.
Knowing and tackling these common triggers and risks can help us stop decompensated heart failure. This can lead to better outcomes for patients.
Diagnostic Approach to Decompensated Heart Failure
Diagnosing decompensated heart failure requires a detailed strategy. This includes clinical assessment and various diagnostic tests. When a patient shows signs of decompensated heart failure, we must thoroughly evaluate them. This helps confirm the diagnosis and guide treatment.
Initial Assessment in Emergency Settings
In emergency settings, the initial assessment is key. It involves a quick check of the patient’s clinical status. This includes:
- Clinical History: We gather information about the patient’s medical history. This includes previous heart failure episodes, comorbidities, and current medications.
- Physical Examination: We look for signs of heart failure like jugular venous distension, peripheral edema, and pulmonary congestion.
- Vital Signs: We monitor vital signs, including blood pressure, heart rate, respiratory rate, and oxygen saturation.
Laboratory Tests and Biomarkers
Laboratory tests are vital in diagnosing decompensated heart failure. Key tests include:
- Complete Blood Count (CBC): This test helps identify infections or anemia that could worsen heart failure.
- Basic Metabolic Panel: It assesses electrolyte levels, renal function, and other metabolic parameters.
- B-type Natriuretic Peptide (BNP) or N-terminal pro b-type natriuretic peptide (NT-proBNP): These biomarkers are elevated in heart failure. They help diagnose and assess the severity of the condition.
Imaging Studies and Other Diagnostics
Imaging studies are essential for evaluating the heart’s structure and function. Commonly used imaging modalities include:
- Echocardiography: It provides information on cardiac structure, function, and hemodynamics.
- Chest X-ray: It helps assess pulmonary congestion and cardiac size.
- Electrocardiogram (ECG): It is useful for identifying arrhythmias or ischemia that may contribute to decompensated heart failure.
By combining the results of these diagnostic approaches, we can accurately diagnose decompensated heart failure. This allows us to develop an effective treatment plan tailored to the patient’s needs.
Emergency Treatment Strategies
Emergency treatment strategies are key in managing decompensated heart failure. They help improve patient outcomes. The main goal is to stabilize the patient and ease symptoms.
Stabilization Techniques
Stabilization techniques are vital in the early treatment of decompensated heart failure. These include:
- Positioning the patient upright to reduce respiratory distress
- Administering supplemental oxygen to improve oxygenation
- Using non-invasive ventilation techniques, such as CPAP or BiPAP, to reduce the workload on the heart
Oxygen Therapy and Ventilatory Support
Oxygen therapy is essential in treating decompensated heart failure. It helps by:
- Correcting hypoxemia and improving tissue oxygenation
- Reducing the heart’s workload by decreasing the need for high cardiac output
- Alleviating symptoms such as dyspnea and orthopnea
In severe cases, ventilatory support may be needed. This can include non-invasive ventilation or, in critical cases, invasive mechanical ventilation.
Immediate Pharmacological Interventions
Immediate pharmacological interventions are vital in managing decompensated heart failure. These interventions typically include:
- Diuretics, such as loop diuretics, to reduce fluid overload and alleviate congestion
- Vasodilators to decrease the heart’s workload by reducing preload and afterload
- Inotropes, in certain cases, to enhance cardiac contractility
The American Heart Association stresses the importance of prompt treatment. It’s critical for improving patient outcomes and reducing mortality.
We must tailor these interventions to each patient’s needs. This includes their medical history, current condition, and response to initial therapy.
Hospital-Based Management Approaches
For patients with decompensated heart failure, hospital care is key for recovery. This care includes watching the patient closely, using advanced treatments, and planning for when they go home.
Inpatient Monitoring and Care
Inpatient monitoring is vital for managing heart failure. We check the patient’s heart function, fluid levels, and kidney health. We use different methods to watch over the patient and make treatment choices.
Close monitoring helps us catch any changes fast. This lets us act quickly to stop things from getting worse. It’s important for keeping patients safe and improving their health.
Advanced Therapies for Severe Cases
For very severe heart failure, advanced therapies might be needed. These include medicines given through an IV to help the heart and reduce swelling. Sometimes, we use machines to support the heart.
- IV medicines to help the heart work better and reduce swelling
- Mechanical support for patients with very bad heart failure
- Ultrafiltration or other treatments for the kidneys as needed
Determining Readiness for Discharge
Before sending a patient home, we check if they’re ready. We look at their fluid levels, kidney function, and overall health. We also make sure their medicines are right and teach them and their family about managing heart failure at home.
By using a detailed hospital-based management plan, we can help patients with heart failure get better. This reduces the chance of them needing to come back to the hospital and improves their life quality.
Long-Term Management After an Episode
After a heart failure episode, managing it long-term is key to avoid future problems. We know managing this condition needs a full plan. This includes changing medications, making lifestyle changes, and following up regularly.
Medication Adjustments and Optimization
Adjusting medications is a big part of managing heart failure long-term. We make sure patients get the right medicines to control their condition. This might mean changing doses, switching medicines, or adding new ones.
“The right medication strategy can significantly improve outcomes for patients with decompensated heart failure.”
Medication adherence is also key. We help patients understand why taking their medicines is so important. This helps lower the chance of future heart failure episodes.
Lifestyle Modifications
Making lifestyle changes is important for managing heart failure long-term. We tell patients to eat better, like cutting down on salt and eating heart-healthy foods. We also encourage them to exercise, but in a way that’s safe for them.
We also push for smoking cessation and limiting alcohol consumption. These changes can greatly improve a patient’s life and lower the risk of more heart problems.
Follow-up Care Protocol
Having a good follow-up care plan is vital. It helps us keep track of how patients are doing and make changes when needed. We see patients regularly to check on them, adjust their treatment, and answer any questions.
By using these long-term management strategies, we can help patients with heart failure live better lives. They can enjoy better health and overall well-being.
Conclusion
Decompensated heart failure is a serious condition that can be life-threatening. We’ve looked at what heart failure is, the terms used for decompensated heart failure, and its types and triggers.
Knowing the signs and symptoms, and how to diagnose and treat it, is key. This knowledge helps both healthcare providers and patients. By understanding the causes and risk factors, people can prevent decompensation and manage their heart failure better.
In summary, decompensated heart failure is a complex issue that needs careful care. We hope this article has helped you understand it better. This way, you can make informed decisions about your treatment and improve your health.
FAQ
What is decompensated heart failure?
Decompensated heart failure is a serious condition. It happens when the heart can’t pump blood well. This leads to fluid buildup in the lungs and body.
What is the difference between compensated and decompensated heart failure?
Compensated heart failure means the heart can pump enough blood, even if it’s weak. Decompensated heart failure is when the heart can’t pump blood well anymore. It’s a worse state.
What are the types of decompensated heart failure?
There are two types. Acute decompensated heart failure happens suddenly. Chronic decompensated heart failure gets worse over time.
What are the symptoms of decompensated heart failure?
Symptoms include sudden, severe shortness of breath and swelling in the legs. These signs need quick medical help or ongoing care.
What triggers decompensated heart failure?
Many things can trigger it. This includes heart attacks, infections, and not taking medicine as directed.
How is decompensated heart failure diagnosed?
Doctors use several steps to diagnose it. They start with an emergency check-up. Then, they do blood tests and imaging like echocardiography.
What is the treatment for decompensated heart failure?
Treatment aims to stabilize the patient. It includes oxygen therapy, ventilatory support, and medicines to ease the heart’s work.
How is decompensated heart failure managed in the long term?
Long-term care involves adjusting medicines and making lifestyle changes. It also includes regular follow-ups to prevent future problems.
What is the impact of decompensated heart failure on healthcare systems?
It has a big impact on healthcare systems. It leads to high costs due to hospital stays and ongoing care, mainly in the U.S.
What is the impact of decompensated heart failure on healthcare systems?
It has a big impact on healthcare systems. It leads to high costs due to hospital stays and ongoing care, mainly in the U.S.
What is uncompensated heart failure?
Uncompensated heart failure is another name for decompensated heart failure. It means the heart can’t pump blood well.
What are the risk factors for decompensated heart failure?
Risk factors include heart attacks, infections, and not following medication instructions. These can all lead to heart failure.
References:
- Chaudhry, R. (2022). Physiology, Cardiovascular. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK493197/



































