Hardening of the arteries in the brain is a major cause of vascular dementia. It’s the second most common form of dementia after Alzheimer’s. Knowing the early signs is key to getting the right care.
At Liv Hospital, we teach families about the 7 main symptoms of hardening of the arteries in the brain. This knowledge helps families make better treatment choices and care decisions.
Key Takeaways
- Vascular dementia is the second most common form of dementia.
- Hardening of the arteries in the brain is a leading cause.
- Understanding early signs is key for quick care.
- Liv Hospital offers patient-focused, world-class care.
- Knowing the symptoms helps families guide treatment.
Understanding Cerebral Arteriosclerosis and Its Impact

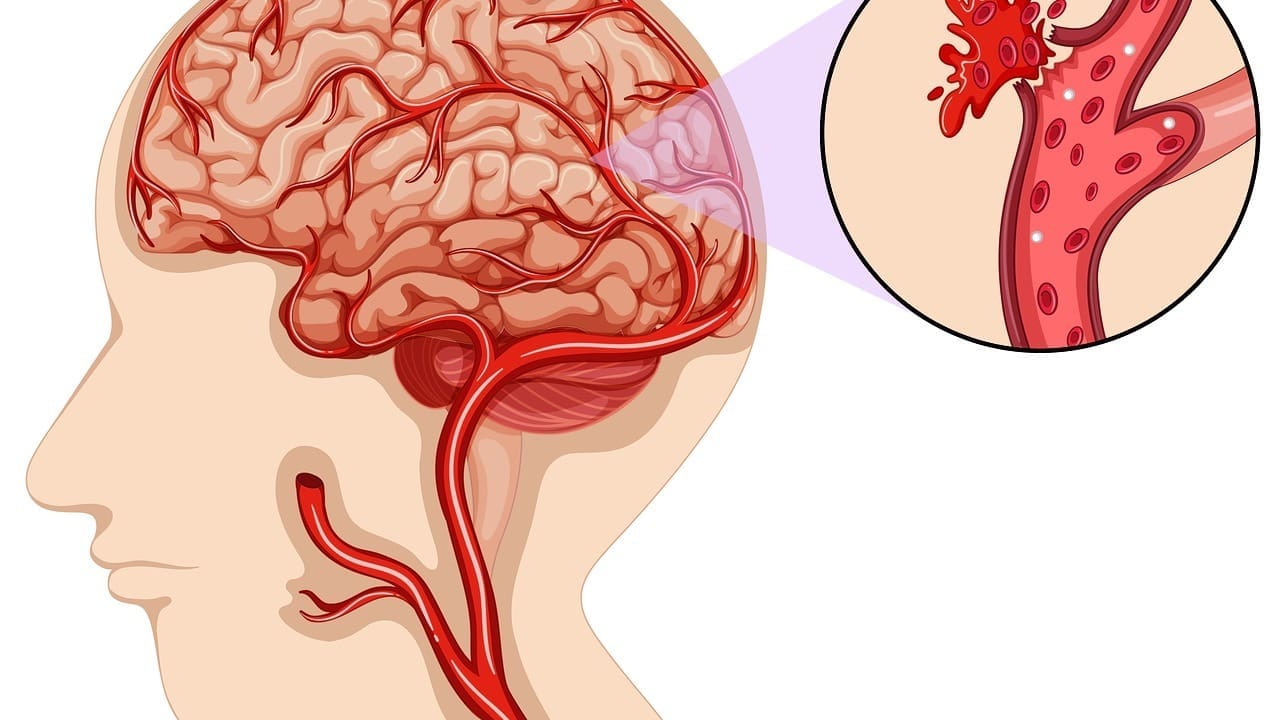
Cerebral arteriosclerosis affects the brain deeply. It’s when the brain’s arteries harden. This can cut down on blood and oxygen to brain cells.
What Causes Hardening of the Arteries in the Brain
The main cause is atherosclerosis. It’s when plaque builds up in artery walls. This makes arteries thick, narrow, and stiff, blocking blood flow.
Atherosclerosis happens over time. It’s influenced by high blood pressure, diabetes, high cholesterol, and smoking. As arteries harden, the brain gets less oxygen and nutrients, causing cognitive decline.
Vascular Dementia as the Second Most Common Form of Dementia
Vascular dementia comes from reduced blood flow to the brain. It’s often due to cerebral arteriosclerosis. It’s the second most common dementia after Alzheimer’s. Knowing about vascular dementia helps in diagnosing and managing it.
| Condition | Causes | Impact |
|---|---|---|
| Cerebral Arteriosclerosis | Atherosclerosis, high blood pressure, diabetes, high cholesterol, smoking | Reduced blood flow to the brain, cognitive decline |
| Vascular Dementia | Reduced blood flow to the brain due to cerebral arteriosclerosis | Cognitive decline, memory loss, difficulty with communication |
Understanding cerebral arteriosclerosis helps us grasp vascular dementia. It shows why managing risk factors is key to preventing or slowing its progression.
Hardening of the Arteries in the Brain Symptoms: The 7 Key Warning Signs

Hardening of the arteries in the brain can cause many symptoms. These symptoms are linked to vascular dementia, affecting memory and thinking. Knowing these signs is key to early detection and treatment.
Difficulty Concentrating and Attention Problems
One major symptom is trouble focusing and paying attention. People might find it hard to stay on task or follow conversations. This can really affect daily life and happiness.
Slowed Thinking and Processing Speed
Another symptom is slower thinking and processing. It can take longer to answer questions or solve problems. This makes it hard to keep up with conversations.
Mood and Personality Changes
Changes in mood and personality are common too. These can include being more irritable, anxious, or depressed. These changes can upset both the person and their family.
Memory Problems and Cognitive Decline
Memory and thinking problems are big signs of vascular dementia. People might forget recent things or struggle to learn new stuff. These problems get worse over time.
Other signs include headaches, confusion, and trouble with balance. Spotting these symptoms early can help slow down dementia’s progress.
The Meaning of Vascular Dementia: Beyond the Basics
Understanding vascular dementia is more than just knowing what it is. It’s about seeing how it affects thinking and daily life. It’s the second most common dementia after Alzheimer’s disease, touching millions of lives worldwide.
How Vascular Dementia Differs from Alzheimer’s Disease
Vascular dementia and Alzheimer’s disease are similar but different. Alzheimer’s is caused by amyloid plaques and tau tangles in the brain. Vascular dementia, on the other hand, is caused by poor blood flow to the brain due to diseased blood vessels.
The main differences are:
- Cause: Vascular dementia is caused by poor blood flow, while Alzheimer’s is caused by amyloid plaques and tau tangles.
- Progression: Vascular dementia has sudden declines, while Alzheimer’s progresses steadily.
- Symptoms: Both affect memory and thinking. But vascular dementia can also cause physical symptoms like weakness or paralysis.
The Connection Between Blood Vessel Damage and Brain Function
Blood vessel damage is key to vascular dementia. When blood vessels in the brain are damaged, brain tissue can die. This leads to the cognitive problems seen in vascular dementia.
The link between blood vessel damage and brain function is clear:
- Reduced Blood Flow: Diseased blood vessels reduce blood to the brain, causing tissue damage.
- Infarctions: Blockages or ruptures in blood vessels can cause dead tissue in the brain.
- White Matter Changes: Small vessel disease can change the brain’s white matter, affecting thinking.
By understanding vascular dementia and its differences from Alzheimer’s, we can improve diagnosis, treatment, and care for those affected.
How Does Vascular Dementia Progress? Understanding the Trajectory
It’s important for patients and caregivers to understand how vascular dementia progresses. This condition often goes through stages, and how fast it moves can differ from person to person.
The Step-Wise Progression Pattern
Vascular dementia progresses in steps, not smoothly. This is because of small strokes or changes in blood vessels in the brain.
This pattern includes:
- Periods of stability or slight improvement
- Sudden declines in cognitive or functional abilities
- Plateaus where the condition remains relatively stable for a period
Fluctuating Symptoms and “Good Days, Bad Days”
Another key feature is the ups and downs in symptoms, known as “good days, bad days.” On good days, patients might seem fine. But on bad days, they may find it hard to think or do things.
This back-and-forth can be due to:
- Changes in blood pressure
- Medication effects
- Co-existing medical conditions
Does Vascular Dementia Progress Quickly?
The speed at which vascular dementia gets worse can vary a lot. Some people might decline quickly, while others might take longer.
Several things can affect how fast it gets worse, including:
| Factor | Impact on Progression |
|---|---|
| Extent of blood vessel damage | More extensive damage can lead to faster progression |
| Presence of other health conditions | Co-existing conditions like diabetes or hypertension can accelerate progression |
| Lifestyle and management of risk factors | Effective management can potentially slow down progression |
Managing vascular dementia needs a full plan, including medical care, lifestyle changes, and support for patients and caregivers. Knowing how it progresses and what affects it helps us tailor care to each person’s needs.
Stages of Vascular Dementia Progression
It’s important for patients and caregivers to know about the stages of vascular dementia. This knowledge helps them prepare and manage symptoms. Each stage brings its own challenges and symptoms.
Early Stage Manifestations
In the early stage, symptoms are mild. They can include:
- Difficulty with planning and organization
- Slowed thinking and processing speed
- Mood changes, such as depression or anxiety
- Mild memory problems
At this point, people can usually do daily tasks on their own. But they might need help with more complex tasks.
Middle Stage Challenges
The middle stage brings more severe symptoms. People may experience:
- Increased memory loss and confusion
- Difficulty with communication and language
- Problems with spatial awareness and judgment
- Changes in personality and behavior
During this stage, patients need more help with daily tasks. Caregivers play a bigger role in managing their care.
Late Stage Symptoms and Care Needs
In the late stage, symptoms are severe. People may face:
- Significant loss of speech and communication skills
- Near-total loss of memory
- Difficulty with swallowing and eating
- Increased risk of infections and other medical complications
At this stage, patients need full-time care. Caregivers must provide emotional support and manage physical needs.
Special Considerations: Sundowning and Post-Stroke Symptoms
As vascular dementia gets worse, patients and caregivers face special challenges. These include sundowning syndrome and the effects of stroke. These factors can greatly affect the quality of life and managing the condition.
Sundowning Syndrome in Vascular Dementia Patients
Sundowning syndrome, also known as sundowners syndrome, is when people with dementia, including vascular dementia, get more agitated, confused, and restless in the late afternoon or early evening. This can be really tough for caregivers, as they may need more help and strategies to manage.
The exact cause of sundowning syndrome is not fully known. It’s thought to be due to a mix of factors, like disruptions in the body’s internal clock, fatigue, and environmental influences. Creating a calm and predictable environment can help lessen these symptoms.
How Symptoms Typically Worsen After Stroke Events
Stroke events can greatly affect vascular dementia, leading to a noticeable decline in cognitive and functional abilities. After a stroke, patients may struggle with confusion, speech, and mood changes.
Managing post-stroke symptoms needs a complete approach, including medical treatment, rehabilitation, and supportive care. Knowing symptoms can worsen after a stroke helps patients and caregivers prepare for the challenges ahead.
It’s key to work closely with healthcare providers to create a care plan that meets each patient’s unique needs, after a stroke event.
Less Common Symptoms and Complications
Some people with vascular dementia face more than just the usual symptoms. These less common symptoms can really affect their quality of life. They need special care.
Vascular Dementia and Seizure Activity
Seizures are a less common but serious issue for some with vascular dementia. Seizures happen because of brain damage from blood vessel problems. A study in Neurology found seizures are more common in vascular dementia patients than in others.
“The occurrence of seizures in vascular dementia patients is a critical aspect that clinicians need to be aware of, as it can significantly affect the management and prognosis of the disease.”
Seizures can show up in different ways, like convulsions or loss of consciousness. To manage seizures, doctors use medicine and suggest lifestyle changes.
Impact on Reading and Language Processing
Vascular dementia can also mess with reading and language skills. Patients might find it hard to understand written or spoken words. This can make it tough for them to talk or read.
How reading and language skills are affected can vary a lot. Some patients might struggle to get what’s written or spoken. Others might find it hard to say what they mean. Speech therapy can help with these problems.
Other Neurological Manifestations
Vascular dementia can also cause other brain problems. These include changes in how the body moves, like weakness or trouble balancing. These symptoms can make it hard for patients to move around safely.
- Motor function changes
- Coordination and balance issues
- Potential for falls and injuries
These symptoms can make it hard for patients to live on their own. They might fall or get hurt more easily. A good care plan that includes physical therapy and safety steps can help.
Diagnosing Vascular Dementia: The Process
To diagnose vascular dementia, doctors use many tools and methods. This detailed approach is needed because of the condition’s complexity and its similarity to other dementias.
Medical Tests and Evaluations
Diagnosing vascular dementia involves several medical tests and evaluations. Imaging tests like MRI or CT scans are key to spotting brain damage from reduced blood flow. We also use cognitive and neuropsychological tests to check memory, language, and problem-solving skills.
These tests help us see how much cognitive decline has happened and if it’s specific to vascular dementia. For example, a patient might take memory tests to see if they can remember recent events or learn new things.
Differentiating from Other Forms of Dementia
One big challenge in diagnosing vascular dementia is telling it apart from other dementias, like Alzheimer’s disease. We do this by looking closely at the patient’s medical history, symptoms, and test results.
Vascular dementia often shows a step-wise decline in cognitive function, matching the timing of strokes. Alzheimer’s disease, on the other hand, starts more slowly. Knowing these differences is key for a correct diagnosis.
“The diagnosis of vascular dementia is not just about identifying cognitive decline but understanding its underlying cause.”
When to Seek Medical Attention
If you or a loved one is showing symptoms like memory loss, confusion, or trouble with communication, get medical help. Early diagnosis can lead to better management of the condition.
We suggest talking to a healthcare professional if you see big changes in cognitive function or worry about stroke or vascular disease risks.
Is Vascular Dementia Progressive and Can It Be Reversed?
Knowing if vascular dementia gets worse is key. It’s caused by less blood to the brain, harming thinking skills a lot.
We’ll look at if vascular dementia gets worse, if symptoms can stop or get better, and what treatment hopes are.
The Progressive Nature of the Condition
Vascular dementia usually gets worse over time. Symptoms get worse because of less blood to the brain. This can happen from more strokes or small vessel disease.
Key factors influencing the progression include:
- Presence of underlying vascular risk factors such as hypertension and diabetes
- Occurrence of further stroke events
- The extent of small vessel disease in the brain
Stabilizing vs. Reversing Symptoms
Even though vascular dementia can’t be reversed, some symptoms can be managed. By controlling risk factors and using the right treatments, we can slow it down.
It’s important to know that while some symptoms might get better, vascular dementia itself can’t be reversed.
The goal of treatment is to manage symptoms and slow the disease’s progress.
Realistic Expectations for Treatment
Treatment for vascular dementia includes many steps. This includes medicine, lifestyle changes, and managing risk factors. These steps can’t reverse the disease but can help keep symptoms stable and improve life quality.
Realistic expectations for treatment include:
- Slowing the progression of cognitive decline
- Managing behavioral symptoms
- Improving overall quality of life through supportive care
By knowing how vascular dementia progresses and what treatments are out there, we can face its challenges better.
Managing Vascular Dementia: Treatment Approaches
Managing vascular dementia needs a mix of medical care, lifestyle changes, and managing risk factors. Every patient is different, so a treatment plan that fits them is key.
Medical Interventions and Medications
Medical care is vital in managing vascular dementia. Medications like cholinesterase inhibitors and memantine help with thinking problems. We also treat conditions like high blood pressure and diabetes, which can lead to vascular dementia.
We might use drugs to prevent strokes in people with vascular dementia. The right medicine and treatment plan depend on the patient’s health and their dementia type.
Lifestyle Modifications to Slow Progression
Changing your lifestyle is a big part of managing vascular dementia. Regular physical activity can help your brain and body. We suggest fun activities like walking, swimming, or tai chi.
Eating right is also important. A healthy diet with lots of fruits, veggies, and lean proteins can help. We tell patients to eat less saturated fats, cholesterol, and salt.
Risk Factor Management
Controlling risk factors is key to slowing down vascular dementia. This means managing high blood pressure, diabetes, and high cholesterol. We also stress the need to stop smoking and drink less alcohol.
Keeping your mind active is also important. Activities like reading, puzzles, and socializing can help your brain stay sharp. These can slow down thinking problems.
With a full treatment plan that includes medicine, lifestyle changes, and managing risk factors, we can make life better for people with vascular dementia. We aim to slow down the disease’s progress.
Conclusion: Living with Vascular Dementia
Vascular dementia is the second most common dementia type. It brings unique challenges. We’ve looked at its symptoms, how it progresses, and how to manage it.
Dealing with vascular dementia needs a full plan. This includes medical care, lifestyle changes, and support. Knowing about the condition helps improve life quality for those affected.
Good support for vascular dementia comes from a team. This team includes doctors, family, and caregivers. Together, we can find ways to handle symptoms, slow the disease, and boost well-being.
Even though vascular dementia gets worse, we can manage its symptoms. The right support and care can greatly improve life for those with it.
What is vascular dementia?
Vascular dementia is the second most common dementia type. It happens when blood flow to the brain is reduced. This often results from a stroke or hardening of brain arteries.
What are the symptoms of hardening of the arteries in the brain?
Symptoms include trouble concentrating and thinking slowly. You might also have memory issues, mood changes, and other cognitive problems.
Is vascular dementia the same as Alzheimer’s disease?
No, they are different. Vascular dementia is caused by blood vessel damage. Alzheimer’s is a degenerative brain disorder.
How does vascular dementia progress?
It progresses in steps, getting worse after strokes or vascular incidents. Symptoms can also change.
Does vascular dementia progress quickly?
Progression varies. Some people progress slowly, while others decline faster, often after a big stroke.
Can vascular dementia be reversed?
Some symptoms can be managed, but it’s generally a progressive condition. Yet, lifestyle changes and interventions can slow it down.
What are the stages of vascular dementia?
It’s divided into early, middle, and late stages. Each stage has different symptoms and care needs.
What is sundowning syndrome in vascular dementia?
Sundowning is a state of confusion, agitation, and aggression. It happens in the late afternoon or early evening.
Can vascular dementia cause seizures?
Yes, it can increase seizure risk. This is due to brain damage and reduced blood flow.
How is vascular dementia diagnosed?
Diagnosis involves medical tests and evaluations. It helps differentiate it from other dementias and find the cause.
What are the treatment approaches for managing vascular dementia?
Treatments include medical interventions, lifestyle changes, and managing risk factors. These help slow progression and manage symptoms.
Can reading difficulties occur in vascular dementia?
Yes, it can affect reading and language skills. This is due to cognitive decline from the condition.
How can symptoms worsen after a stroke?
Symptoms can worsen after a stroke. This is because of more brain damage, leading to increased cognitive decline and other symptoms.


































