At Liv Hospital, we know how serious Acute Decompensated Heart Failure (ADHF) is. It’s when heart failure symptoms suddenly get worse. This happens because of fluid buildup and higher pressure in the heart, needing quick and skilled medical help. Understand acute decompensated CHF, its symptoms, and treatment management tips.
We focus on our patients at Liv Hospital. Our team uses the latest methods to diagnose and treat ADHF. We aim to give the best care possible, supporting patients from all over the world. Our goal is to provide care that is based on solid evidence and a caring environment.
Key Takeaways
- ADHF is a critical condition requiring immediate medical attention.
- Liv Hospital provides patient-centered care and advanced treatment protocols.
- Timely management of ADHF is key to avoiding more problems.
- Our hospital is dedicated to delivering top-notch healthcare.
- We offer full support for patients from other countries.
Understanding Acute Decompensated CHF: Definition and Overview

Acute decompensated heart failure (ADHF) is a serious condition. It happens when heart failure symptoms suddenly get worse. This is often due to heart problems like ischemia or arrhythmias.
What Defines Acute Decompensated Heart Failure
ADHF is marked by quick onset or worsening of symptoms like dyspnea, fatigue, and fluid retention. These signs mean the heart is not pumping well anymore. They call for quick medical help.
- Dyspnea at rest or on exertion
- Rapid weight gain due to fluid retention
- Fatigue and weakness
- Swelling in legs, ankles, and feet
The Transition from Stable to Decompensated State
The shift from stable to decompensated heart failure is complex. It’s caused by things like cardiac ischemia, arrhythmias, infections, and not taking medicine as directed. Knowing these causes helps in preventing and treating ADHF.
- Cardiac ischemia or myocardial infarction
- Arrhythmias, like atrial fibrillation
- Infections and inflammatory conditions
- Not following the heart failure medication plan
- Drinking too much fluid or sodium
Understanding ADHF’s definition, symptoms, and causes helps doctors manage it better. This can lead to better outcomes for patients.
Epidemiology and Impact of ADHF
It’s key to grasp the spread of ADHF to better handle its effects on health and healthcare costs. ADHF hits a big chunk of the world’s population, mainly the elderly.
Prevalence and Demographics
ADHF leads to most heart failure hospital stays globally. It grows more common with age, hitting older folks hard. Research links it to a lot of sickness and death, mainly in the elderly.
Demographic traits of ADHF patients often include:
- Advanced age
- Comorbid conditions like hypertension, diabetes, and kidney issues
- History of heart failure
This shows we need special care plans for ADHF patients. Plans that meet their unique needs.
Healthcare Burden and Costs
The healthcare load of ADHF is huge, with big expenses for hospital stays, treatments, and after-care. It puts a big dent in healthcare budgets, making efficient management key to cut costs.
| Aspect | Description | Impact |
| Hospitalization Rates | High rates of hospitalization due to ADHF | Increased healthcare costs and resource utilization |
| Length of Stay | Prolonged hospital stays for ADHF management | Higher costs and increased risk of hospital-acquired complications |
| Post-discharge Care | Need for ongoing care and monitoring post-discharge | Additional healthcare costs and resource utilization |
Knowing how ADHF spreads and affects us helps healthcare workers. They can then craft better plans to help patients and lessen the financial weight of this condition.
Pathophysiology of Acute Decompensation
To understand ADHF, we must look at the changes in blood flow and the body’s hormonal responses. These changes happen when the heart suddenly fails to work right. It’s a mix of blood flow issues and hormonal shifts.
Hemodynamic Alterations
The way blood flows changes a lot in ADHF. This leads to more fluid in the body, causing swelling and fluid buildup in the lungs. The heart can’t pump enough blood, making things worse.
- Increased venous pressure
- Fluid accumulation and redistribution
- Pulmonary congestion
- Peripheral edema
The hemodynamic changes affect more than just fluid levels. They also mess with the heart’s ability to pump and the blood vessels’ resistance. This creates a cycle that can make things even harder for the patient.
Neurohormonal Mechanisms
Neurohormonal changes are also key in ADHF. The body’s stress response and the RAAS system get activated. This leads to blood vessels tightening, holding onto sodium, and more fluid buildup. These changes start as a way to help but end up making heart failure worse.
- Activation of RAAS
- Sympathetic nervous system activation
- Vasoconstriction and sodium retention
The mix of blood flow and hormonal changes makes ADHF complex. Knowing about these processes helps us find better ways to treat it.
Common Triggers and Precipitating Factors
Heart failure can suddenly get worse due to many factors. Knowing what causes this is key to managing and preventing it.
Cardiac-Related Triggers
Heart problems are a main reason for ADHF. These include:
- Cardiac Ischemia: Myocardial ischemia or infarction can significantly impair cardiac function, leading to decompensation.
- Arrhythmias: Both tachyarrhythmias and bradyarrhythmias can precipitate ADHF by disrupting the heart’s normal rhythm and reducing its efficiency.
- Valvular Dysfunction: Acute or worsening valvular disease can lead to ADHF by causing sudden changes in cardiac hemodynamics.
Non-Cardiac Precipitants
Other factors also play a big role in ADHF. These include:
- Infections: Severe infections, like pneumonia and sepsis, can cause ADHF by leading to inflammation and instability.
- Uncontrolled Hypertension: High blood pressure can make the heart work too hard, leading to ADHF.
- Renal Dysfunction: Kidney problems can cause fluid buildup and imbalances, leading to ADHF.
Lifestyle and Environmental Factors
Lifestyle and environment can also affect ADHF. These include:
- Dietary Indiscretion: Eating too much salt and fluid can cause volume overload and ADHF.
- Medication Non-Adherence: Not taking heart failure meds as directed can lead to worsening symptoms.
- Environmental Factors: Extreme weather and high altitudes can also trigger ADHF in some people.
Knowing these triggers helps doctors create better plans to prevent and manage ADHF. This can greatly improve patient care.
Clinical Presentation and Symptoms of ADHF
ADHF shows a mix of symptoms that show how serious it is and how it affects the body. These symptoms need quick medical attention.
Pulmonary Congestion Manifestations
Pulmonary congestion is key in ADHF. It causes shortness of breath, trouble breathing when lying down, and waking up with breathlessness. These happen because fluid builds up in the lungs, making it hard to breathe.
Systemic Congestion Signs
Systemic congestion in ADHF shows up as swelling in the legs and ankles, fluid in the belly, and a big jugular vein. These signs mean there’s too much fluid and high venous pressure.
The table below lists common signs and symptoms of systemic congestion in ADHF:
| Signs and Symptoms | Description |
| Peripheral Edema | Swelling in the legs, ankles, and feet due to fluid accumulation |
| Ascites | Fluid accumulation in the abdominal cavity, leading to abdominal distension |
| Jugular Venous Distension | Enlargement of the jugular vein due to increased venous pressure |
Low Cardiac Output Symptoms
Low cardiac output in ADHF causes fatigue, weakness, and less ability to exercise. This is because the heart can’t pump enough blood, leading to poor blood flow to important organs.
It’s important to recognize these symptoms and signs early. Quick action can help manage ADHF, improve patient outcomes, and lower the chance of serious problems.
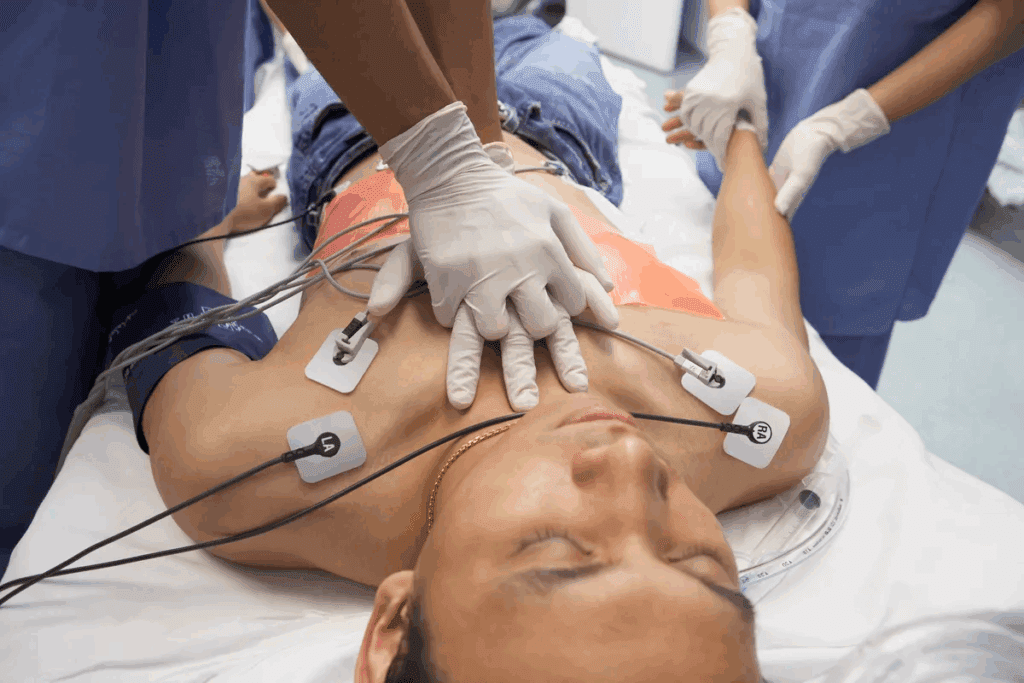
Diagnostic Approach to Acute Decompensated Heart Failure
Getting a correct diagnosis for acute decompensated heart failure is key. It needs a mix of clinical checks, lab tests, and imaging. A detailed diagnostic plan is vital for good care.
Initial Clinical Assessment
The first step in diagnosing ADHF is very important. It includes a detailed medical history and physical check-up. These help spot heart failure signs like shortness of breath and swelling in legs.
Doctors must watch for these signs to start more tests right away.
- Looking at the patient’s history for heart issues or past episodes
- Checking for symptoms like breathing trouble, tiredness, and weight gain
- Doing a physical exam to find fluid buildup signs
Laboratory Evaluation
Lab tests are key in diagnosing ADHF. Tests like natriuretic peptides (BNP or NT-proBNP) show heart failure. Other tests, like troponin, check for heart damage.
Lab tests confirm the diagnosis and show how severe ADHF is.
“Biomarkers like BNP are invaluable in the diagnosis of heart failure, providing a quantitative measure of ventricular stress.”
Imaging and Hemodynamic Assessment
Imaging, like echocardiography, is vital for checking the heart’s shape and how it works. It finds out why ADHF happened, like heart muscle problems or valve issues.
Echocardiography is key in diagnosing ADHF. It shows how the heart is working and what treatments might help.
Classification and Risk Stratification in ADHF
Understanding ADHF classification and risk stratification is key for managing patients well. It involves identifying clinical profiles and phenotypes. Risk stratification uses prognostic indicators to assess patient risk.
Clinical Profiles and Phenotypes
ADHF clinical profiles are based on congestion, perfusion status, and cardiac function. We identify several phenotypes, including:
- Patients with predominantly pulmonary congestion
- Those with systemic congestion
- Patients presenting with low cardiac output
Knowing these phenotypes helps tailor management to each patient’s needs.
Prognostic Indicators and Risk Assessment
Risk stratification in ADHF involves assessing prognostic indicators to predict outcomes. Key indicators include:
- Biomarkers such as natriuretic peptides
- Hemodynamic parameters like blood pressure and cardiac output
- Renal function and evidence of organ dysfunction
By evaluating these indicators, we can spot high-risk patients. We then intensify their management.
Immediate Management Strategies for ADHF
When ADHF is diagnosed, the first step is to stabilize the patient. This is done through medicine and supportive care. It’s key to improve patient outcomes and lower the risk of complications.
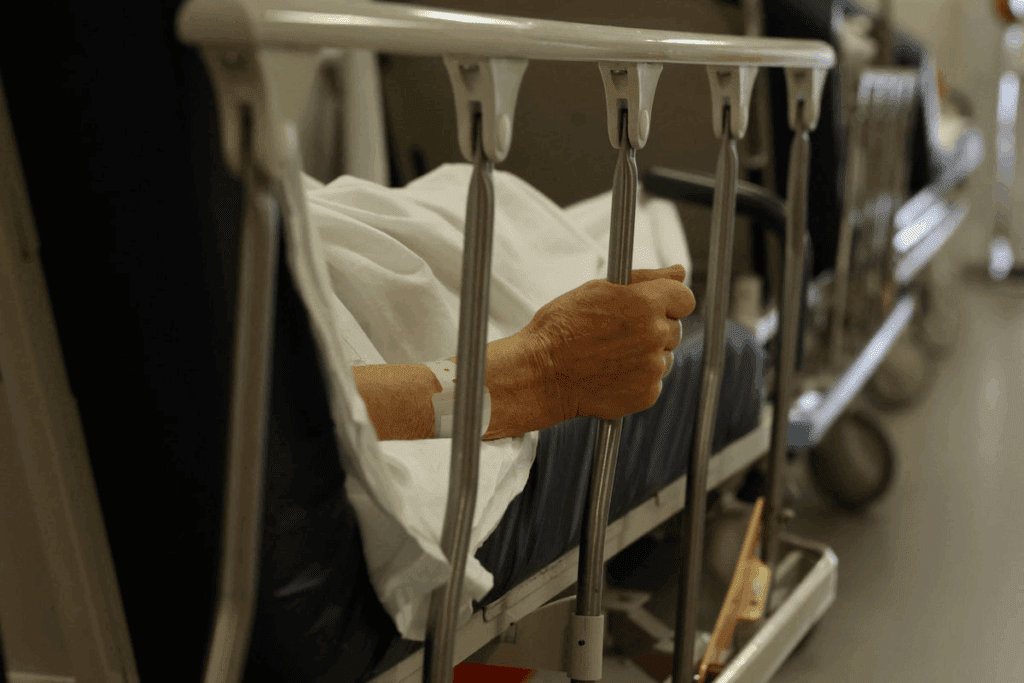
Initial Stabilization Measures
The first step in managing ADHF is to check the patient’s health and stabilize them. This includes oxygen therapy to help with low oxygen levels, positioning the patient to reduce blood flow, and diuretics to ease congestion.
It’s also important to watch the patient’s vital signs and symptoms closely. This helps make changes to the treatment plan as needed. Early spotting of complications is key to stop things from getting worse.
Diuretic Therapy Approaches
Diuretics are a main part of treating ADHF. They help reduce fluid buildup and ease congestion. Loop diuretics, like furosemide, are often used because they work well.
- They are given intravenously for quick results.
- The dose is adjusted based on how the patient responds and their kidney function.
- It’s important to watch for side effects, like imbalances in electrolytes.
The goal is to find the right balance. Too much diuresis can cause dehydration and lower heart output.
Vasodilator and Vasopressor Treatment
Along with diuretics, vasodilators and vasopressors may be used. Vasodilators help lower blood pressure and improve heart function. Vasopressors are used for severe low blood pressure to keep blood pressure up.
The choice of these medicines depends on the patient’s health, blood pressure, heart function, and organ perfusion. It’s important to adjust them carefully to avoid bad effects.
Advanced Therapeutic Interventions
Managing Acute Decompensated Heart Failure often needs advanced treatments. These are key for patients who don’t get better with first treatments or need close care.
Inotropic Support
Inotropic agents boost the heart’s strength, helping it pump better in ADHF patients. Common inotropes are dobutamine and milrinone. They help most in patients with low heart output.
- Dobutamine: Makes the heart stronger and slightly widens blood vessels.
- Milrinone: Boosts heart strength and widens blood vessels, lowering blood pressure.
But, inotropes are used only for a short time because of possible side effects. These can include heart rhythm problems and higher heart oxygen need.
Mechanical Circulatory Support Options
Mechanical circulatory support (MCS) devices help a failing heart, keeping blood flowing well. These devices can be lifesaving for patients waiting for a heart transplant or with heart failure that can be fixed.
- Intra-aortic balloon pump (IABP): Helps blood flow better to the heart and lowers blood pressure.
- Left ventricular assist devices (LVADs): Help the left ventricle pump better, increasing blood flow.
- Extracorporeal membrane oxygenation (ECMO): Provides temporary support for both heart and lung failure.
Ultrafiltration and Dialysis
Ultrafiltration and dialysis help manage fluid overload in ADHF patients, mainly those not responding to diuretics. Ultrafiltration removes extra fluid without big changes in electrolytes, while dialysis fixes electrolyte imbalances and removes waste.
- Ultrafiltration: Good for quick fluid removal in severe cases.
- Dialysis: Helps in patients with kidney failure or severe electrolyte issues.
Choosing the right patient for these treatments and closely watching them is important. This helps get the most benefits and avoid risks.
Transitioning Care: Care Hospital to Home Management
When ADHF patients are ready to go home, a smooth transition is key. This phase is vital for ongoing care and support. It helps them manage their condition well.
Discharge Planning and Readiness Assessment
Good discharge planning is essential for a smooth move. It checks if the patient is ready to leave. It also makes sure they and their caregivers know the care plan. And it sets up follow-up care.
Key components of discharge planning include:
- Checking if the patient is clinically stable
- Teaching patients and caregivers about medication and lifestyle changes
- Setting up follow-up appointments and home care services
Medication Reconciliation and Optimization
Medication reconciliation is a key step. It checks the patient’s medications for accuracy and effectiveness.
| Medication Management Task | Description |
| Medication Review | Checking the patient’s medications for interactions or duplicates |
| Medication Adjustment | Changing dosages or medications to improve treatment |
| Patient Education | Telling patients about their medications, including how to take them and possible side effects |
Follow-up Care Coordination
Coordinating follow-up care is important. It ensures the patient gets ongoing support and monitoring. This includes setting up follow-up visits and talking with other healthcare providers.
Good follow-up care can prevent readmissions by catching and fixing problems early.
By focusing on discharge planning, medication review, and follow-up care, we can help ADHF patients transition smoothly from the hospital to home.
Conclusion: Future Directions in ADHF Management
Managing Acute Decompensated Heart Failure (ADHF) is complex. We’ve looked at its causes, symptoms, and current treatments. Now, we focus on what’s next in managing ADHF.
New research aims to create better, more personalized treatments for ADHF. We expect studies to reveal more about ADHF’s causes. This will help doctors tailor care to each patient. Also, new tech like wearable devices and remote monitoring will improve patient care.
The future of ADHF management will combine new evidence, tech, and treatments. We’re dedicated to providing top-notch care for ADHF patients. We’re excited for the advancements that will enhance patient outcomes and quality of life.
FAQ
What is Acute Decompensated Heart Failure (ADHF)?
ADHF is when heart failure symptoms suddenly get worse. This includes trouble breathing, swelling in legs or feet, and feeling very tired. It’s a serious condition that needs quick medical help.
What are the common triggers of ADHF?
ADHF can be triggered by heart problems like heart attacks or irregular heartbeats. It can also be caused by non-heart issues like infections, anemia, or not taking medication as directed.
How is ADHF diagnosed?
Doctors use a few ways to diagnose ADHF. They look at symptoms, run lab tests, and do imaging studies like echocardiograms. These help check how well the heart is working and if there’s fluid buildup.
What are the immediate management strategies for ADHF?
First, doctors stabilize ADHF patients with oxygen and diuretics to reduce fluid. They also use medicines to control blood pressure and help the heart pump better.
What is the role of inotropic support in ADHF management?
In ADHF, inotropic support helps the heart pump stronger. It’s used when patients are very sick but is only for short-term use because of its risks.
How is care transitioned from hospital to home for ADHF patients?
When ADHF patients go home, doctors plan their care carefully. They make sure medications are right and set up follow-up visits. This helps prevent them from getting sicker again.
What is the significance of risk stratification in ADHF?
Risk stratification helps doctors find out who is most at risk. This lets them focus on those who need the most help and watch them closely to improve their chances of getting better.
How does Liv Hospital approach the management of ADHF?
Liv Hospital uses a detailed plan to manage ADHF. We use the latest treatments and care that puts the patient first. This way, we offer top-notch care to patients from around the world.
What are the future directions in ADHF management?
For ADHF, we’re looking at new treatments and better ways to support the heart. We also want to use digital health to improve care and results for patients.
References:
- Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766.https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312


































