Last Updated on December 4, 2025 by Ugurkan Demir

Understand dysrhythmia define meaning, its causes, and types of irregular heart rhythms in detail. A dysrhythmia is an irregular heart rhythm. It can be slow or fast. This happens when the heart’s electrical system gets disrupted.
Knowing what dysrhythmia is and what it means is key. It helps us understand its health risks. Dysrhythmias come in various types, with atrial fibrillation being the most common.
Spotting dysrhythmia early and treating it right is critical. It helps avoid serious issues like stroke or sudden death. At Liv Hospital, we focus on new research and ways to manage dysrhythmias better.
Key Takeaways
- Understanding dysrhythmia is key to knowing its health risks.
- Dysrhythmias have different types based on their cause and heart rate.
- Atrial fibrillation is the most common type of dysrhythmia.
- Early detection and treatment are vital to avoid serious problems.
- Liv Hospital stresses the need for ongoing research and new ways to manage dysrhythmias.
Understanding the Medical Meaning of Dysrhythmia

The term dysrhythmia is often misunderstood. It refers to an abnormal heart rhythm. This can be too fast, too slow, or irregular. Knowing its medical meaning means understanding its pronunciation, its relation to arrhythmia, and its history in cardiology.
Dysrhythmia Pronunciation Guide
The correct way to say dysrhythmia is dis-rith-mee-uh. Getting it right is key for clear communication in healthcare. Mispronunciation can cause confusion, which is bad in stressful medical situations.
Dysrhythmia vs. Arrhythmia: Terminology Clarification
Dysrhythmia and arrhythmia both describe irregular heartbeats. But “dys-” means bad, and “a-” means without. So, dysrhythmia is about an abnormal rhythm, while arrhythmia is about a lack of rhythm. Both terms describe heartbeats that are too fast, too slow, or irregular.
| Term | Prefix Meaning | Clinical Implication |
| Dysrhythmia | Bad or difficult | Abnormal heart rhythm |
| Arrhythmia | Without | Lack of normal heart rhythm |
Historical Context in Cardiology
The study of heart rhythms started in the early 20th century with electrocardiography (ECG). Over time, our knowledge of dysrhythmias has grown. This is thanks to new technology and research, leading to better treatments.
Exploring dysrhythmia shows how important it is to understand it well. By knowing how to say it, its meaning, and its history, we can better grasp its impact on heart health.
How to Define Dysrhythmia in Clinical Practice
To understand dysrhythmia in clinical practice, we need to know about the heart’s normal electrical system. Dysrhythmia, or irregular heartbeat, happens when this system is disrupted. This leads to abnormal heart rhythms.
The Normal Cardiac Conduction System
The heart’s electrical system is complex. It starts with the sinoatrial (SA) node, the heart’s natural pacemaker. It sends the first electrical impulse.
This impulse goes to the atrioventricular (AV) node, where it’s delayed. Then, it moves to the ventricles through the bundle of His and bundle branches. The impulse reaches the Purkinje fibers, making the ventricles contract. This results in a normal heartbeat.
Characterizing Abnormal Heart Rhythms
Abnormal heart rhythms, or dysrhythmias, happen when the heart’s electrical system is disrupted. This can cause irregular heartbeats. Dysrhythmias can be fast (tachycardia), slow (bradycardia), or irregular.
To understand these rhythms, doctors look at ECG patterns, symptoms, and medical history. This helps them diagnose and treat dysrhythmias effectively. It improves patient care.
The Physiological Basis of Cardiac Dysrhythmias
It’s key to know how cardiac dysrhythmias work to treat them well. These issues happen when the heart’s electrical system gets messed up. This leads to irregular heartbeats.
The heart’s electrical system is quite complex. It has many paths that help the heartbeat stay regular. The sinoatrial (SA) node, or the heart’s natural pacemaker, starts the heartbeat. Then, the signal goes through the atrioventricular (AV) node and down to the ventricles.
Electrical Pathways of the Heart
The heart’s electrical paths are vital for a regular heartbeat. The SA node sends out an electrical signal. This signal goes through the atria, making them contract.
The signal then hits the AV node. This node delays the signal before it reaches the ventricles. This delay helps the ventricles contract in sync.
Mechanisms of Dysrhythmic Events
Dysrhythmic events happen when the heart’s electrical paths get disrupted. This can be caused by many things, like abnormal automaticity or re-entry circuits. Knowing how these happen helps doctors diagnose and treat dysrhythmias better.
| Mechanism | Description | Examples |
| Abnormal Automaticity | Altered pacemaker activity | Ectopic beats, tachycardia |
| Triggered Activity | Abnormal electrical activity triggered by afterdepolarizations | Triggered arrhythmias |
| Re-entry Circuits | Electrical signal re-entering a pathway | Atrial flutter, ventricular tachycardia |
Understanding the heart’s electrical system and how dysrhythmias occur helps doctors treat these conditions better. They can then create specific plans to manage these heart issues.
Classification of Dysrhythmias by Rate and Origin
Understanding dysrhythmias is key for diagnosis and treatment. They are grouped by heart rate (slow or fast) and where they start in the heart (supraventricular or ventricular).
Bradycardic Dysrhythmias: When the Heart Beats Too Slowly
Bradycardic dysrhythmias mean the heart beats less than 60 times a minute. This can cause blood and oxygen to not reach organs well. Symptoms include dizziness, fatigue, and shortness of breath. Causes range from problems with the sinus node to certain medicines.
A study in a cardiology journal says, “Bradycardia is common, mainly in the elderly. It often shows there’s a bigger problem with the heart or body.”
“The management of bradycardia depends on its cause and severity, ranging from observation to pacemaker implantation.”
Tachycardic Dysrhythmias: Rapid Heart Rhythms
Tachycardic dysrhythmias have heart rates over 100 beats per minute. These fast rhythms can make the heart less efficient. Symptoms are palpitations, chest pain, and in severe cases, loss of consciousness. Tachycardic dysrhythmias need quick evaluation and treatment.
| Characteristics | Bradycardic Dysrhythmias | Tachycardic Dysrhythmias |
| Heart Rate | Fewer than 60 beats per minute | More than 100 beats per minute |
| Common Symptoms | Dizziness, fatigue, shortness of breath | Palpitations, chest pain, loss of consciousness |
| Causes | Sinus node dysfunction, certain medications | Supraventricular or ventricular origins, electrolyte imbalances |
Supraventricular vs. Ventricular Origins
The origin of a dysrhythmia is key in its classification. Supraventricular dysrhythmias start above the ventricles, like in the atria. Ventricular dysrhythmias start in the ventricles.
Knowing if a dysrhythmia is supraventricular or ventricular is vital for treatment. For example, supraventricular tachycardia might be treated with vagal maneuvers or medicines. Ventricular tachycardia often needs more serious treatments, like cardioversion or defibrillation.
In conclusion, classifying dysrhythmias by rate and origin helps understand these complex heart conditions. Recognizing the types and origins helps doctors create effective treatment plans for each patient.
Common Types of Dysrhythmias and Their Characteristics
Dysrhythmias come in many forms, each with its own traits and health impacts. Knowing these differences is key for correct diagnosis and treatment.
Atrial Fibrillation: The Most Prevalent Dysrhythmia
Atrial fibrillation causes an irregular and often fast heart rate. It raises the risk of stroke, heart failure, and other heart issues. The irregular heartbeat can lead to blood clots forming in the heart, which may dislodge and travel to the brain, causing a stroke. It’s more common in older adults and those with heart disease.
Atrial Flutter and Supraventricular Tachycardia
Atrial flutter has a rapid but regular heartbeat. It happens when there’s a short circuit in the heart’s upper chambers. Supraventricular tachycardia (SVT) is a fast heartbeat that starts above the ventricles. Both can cause symptoms like palpitations, shortness of breath, and fatigue. SVT episodes can be triggered by stress, caffeine, or certain medications.
Ventricular Tachycardia and Fibrillation
Ventricular tachycardia is a serious condition with a fast heart rate starting in the ventricles. If not treated quickly, it can turn into ventricular fibrillation. This can lead to cardiac arrest if immediate medical intervention is not provided. Ventricular fibrillation is a medical emergency needing immediate defibrillation.
Heart Blocks and Other Conduction Disorders
Heart blocks happen when there’s a delay or block in the electrical pathway between the heart’s upper and lower chambers. The severity can range from mild to complete heart block, where signals from the upper chambers can’t reach the lower chambers. Other conduction disorders include bundle branch blocks, which affect the electrical conduction system of the heart. These can cause symptoms like dizziness, fainting, and fatigue, and may need a pacemaker.
Causes and Risk Factors for Developing Dysrhythmias
It’s important to know what causes dysrhythmias to prevent and manage them well. Dysrhythmias, or abnormal heart rhythms, come from many factors. These include heart, non-heart, and genetic issues.
Cardiac-Related Causes
Heart problems are a big reason for dysrhythmias. Conditions like coronary heart disease and heart valve issues can mess up the heart’s rhythm. Heart muscle damage from coronary heart disease can lead to abnormal rhythms. Heart valve problems can also disrupt the heart’s electrical system, causing dysrhythmias.
Heart failure and cardiomyopathy are other heart issues that can cause dysrhythmias. Heart failure means the heart can’t pump enough blood. Cardiomyopathy is a disease of the heart muscle that can disrupt electrical activity, leading to dysrhythmias.
Non-Cardiac Causes and Environmental Factors
Non-heart and environmental factors also play a big role. Electrolyte imbalances can affect the heart’s electrical activity. Problems with electrolytes like potassium, sodium, and calcium can disrupt the heart’s rhythm. Some medications used for heart conditions can also cause dysrhythmias as a side effect.
Lifestyle choices like drinking too much alcohol and smoking can raise the risk of dysrhythmias. Environmental toxins and high stress levels can also contribute to the risk.
Genetic Predispositions and Inherited Conditions
Genetic factors and inherited conditions are also key. Some people are born with heart electrical system issues like long QT syndrome or Brugada syndrome. These can increase the risk of dangerous dysrhythmias.
Family history is important for identifying risk. If you have a family history of dysrhythmias or related conditions, talk to your doctor. They can help with preventive measures.
Clinical Presentation and Diagnosis of Dysrhythmias
Understanding dysrhythmias is key to correct diagnosis and treatment. Dysrhythmias, or abnormal heart rhythms, show up in many ways. This makes diagnosing them a complex task.
Recognizing Symptoms Across Different Types
Dysrhythmias can cause a range of symptoms. Common signs include palpitations, dizziness, and shortness of breath. Some people might also feel fatigue, chest pain, or fainting spells. Spotting these symptoms is the first step to figuring out the problem.
A study in a top cardiology journal said that symptoms can vary a lot. This highlights the need for a detailed check-up.
“The variability in symptoms shows how important a detailed patient history and tests are.”
Diagnostic Tools and Procedures
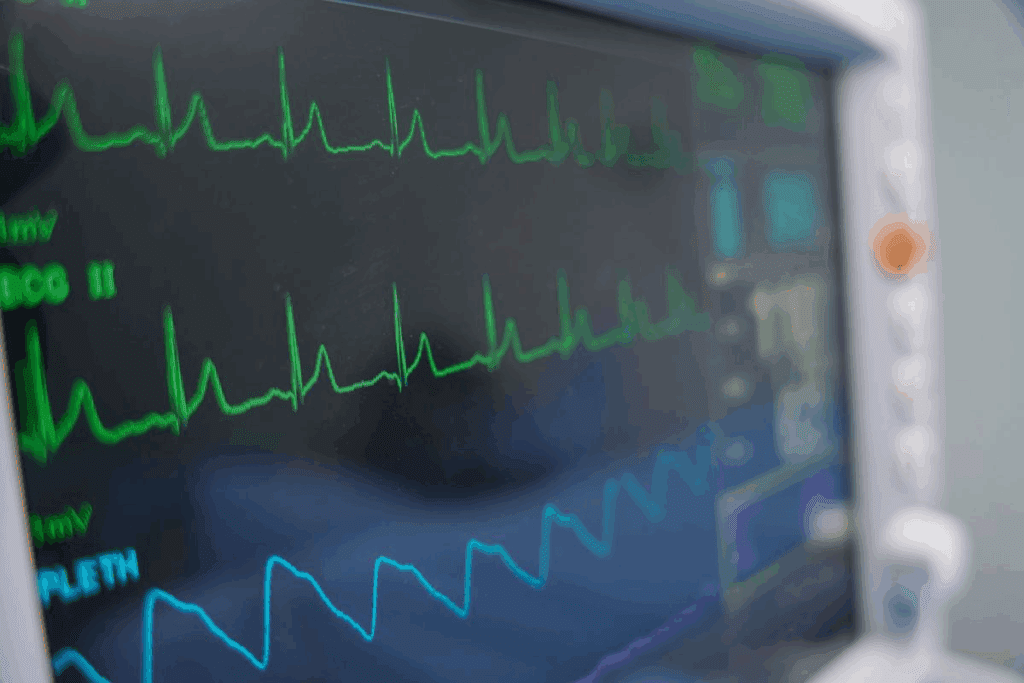
Diagnosing dysrhythmias uses several tools and methods. The most common is the electrocardiogram (ECG), which tracks the heart’s electrical activity. Other tools include Holter monitors, event recorders, and electrophysiological studies.
| Diagnostic Tool | Description | Use in Dysrhythmia Diagnosis |
| Electrocardiogram (ECG) | Records the heart’s electrical activity | Initial diagnosis and monitoring |
| Holter Monitor | 24-48 hour continuous ECG recording | Monitoring intermittent symptoms |
| Event Recorder | Long-term ECG recording activated by symptoms | Diagnosing infrequent dysrhythmias |
Interpreting Electrocardiogram Patterns
Reading ECG patterns is vital for diagnosing dysrhythmias. ECGs show the type, origin, and severity of the rhythm problem. For example, atrial fibrillation has an irregular rhythm, while ventricular tachycardia shows fast ventricular beats.
By understanding ECG patterns, along with symptoms and patient history, doctors can accurately diagnose and treat dysrhythmias.
Dysrhythmia Define: Medical Implications and Complications
It’s important to know the health risks of dysrhythmias. These abnormal heart rhythms can cause serious problems if not treated right.
Stroke Risk and Prevention Strategies
Dysrhythmias, like atrial fibrillation, increase stroke risk. The irregular heartbeat can cause blood clots. These clots can travel to the brain, leading to a stroke.
To lower this risk, doctors use anticoagulant drugs. They also do cardioversion and catheter ablation to fix the heart rhythm.
| Prevention Strategy | Description | Benefits |
| Anticoagulant Therapy | Use of medications to prevent blood clot formation | Reduces stroke risk |
| Cardioversion | Procedure to restore normal heart rhythm | Can reduce stroke risk and improve symptoms |
| Catheter Ablation | Minimally invasive procedure to destroy abnormal electrical pathways | Can provide long-term relief from dysrhythmia symptoms |
Heart Failure as a Consequence
Long-term dysrhythmias can cause heart failure. This is when the heart can’t pump enough blood. The irregular rhythm stresses the heart too much.
To avoid heart failure, managing dysrhythmias is key. Doctors use medicines, lifestyle changes, and sometimes devices like pacemakers.
Sudden Cardiac Death: Risk Assessment and Prevention
Some dysrhythmias, like ventricular tachycardia and fibrillation, can cause sudden cardiac death. Doctors check the heart’s health and look for any underlying conditions to assess this risk.
To prevent sudden cardiac death, doctors use ICDs. They also prescribe medicines and suggest lifestyle changes.
Understanding dysrhythmia’s health risks helps doctors create better care plans. This improves patient outcomes.
Treatment Approaches for Various Dysrhythmias
Managing dysrhythmias needs a detailed plan based on the type and severity. We’ll look at different treatments, their uses, and benefits.
Pharmacological Management Options
Medicine is key in treating dysrhythmias. Anti-arrhythmic drugs help control heart rhythm. They fall into groups like beta-blockers and calcium channel blockers.
The right drug depends on the dysrhythmia, other health issues, and possible side effects.
Catheter Ablation and Other Interventional Procedures
Catheter ablation is a procedure to fix abnormal heart paths. It’s great for supraventricular tachycardia and some ventricular tachycardia. Another method is cardioversion, which uses an electrical shock to fix rhythm.
Device Therapies: Pacemakers and Defibrillators
Devices are vital for managing dysrhythmias, mainly for serious risks. Pacemakers help with slow heart rates. Implantable cardioverter-defibrillators (ICDs) catch and fix dangerous arrhythmias.
These devices can save lives and improve life quality for those with severe dysrhythmias.
Living with Dysrhythmia: Management and Quality of Life
Learning to live with dysrhythmia can greatly improve your life. It’s about using daily strategies, making lifestyle changes, and knowing when to get medical help.
Daily Management Strategies
Managing dysrhythmia every day needs a proactive mindset. Here’s what we recommend:
- Check your heart rate and rhythm as your doctor tells you to.
- Keep a log of any symptoms or irregular heartbeats to talk about with your doctor.
- Stick to your medication as prescribed.
Following your treatment plan is key to managing dysrhythmia well. It’s important to listen to your doctor and go to all follow-up appointments.
Lifestyle Modifications for Dysrhythmia Patients
Changing your lifestyle can help manage dysrhythmia. Here are some suggestions:
- Eat a healthy diet full of fruits, vegetables, and whole grains.
- Do regular physical activity, as your doctor advises.
- Avoid caffeine and nicotine.
Lowering stress is also important. Try meditation, yoga, or deep breathing to help.
Psychological Impact and Coping Mechanisms
Dysrhythmia can affect your mind, leading to anxiety or depression. We suggest:
- Get support from family, friends, or support groups.
- Talk about your feelings with your healthcare provider.
- Do things that make you happy and take your mind off worries.
“The psychological impact of living with a chronic condition like dysrhythmia should not be underestimated. Support and understanding are key to coping.” – A healthcare professional
When to Seek Emergency Care
Knowing when to get emergency care is important. Seek help right away if you have:
- Severe chest pain or discomfort.
- Difficulty breathing.
- Severe dizziness or fainting.
By using these strategies and staying aware of your condition, you can live better with dysrhythmia.
Conclusion: Advances in Dysrhythmia Research and Care
As we learn more about dysrhythmias, care for patients is getting better. Liv Hospital is leading the way with top-notch care. We use the newest research and tech to help our patients.
The future of treating dysrhythmias looks bright. New research and ideas are making treatments better. This means patients can live better lives.
We at Liv Hospital are always looking to improve. We use the latest research and tech to give our patients the best care. This way, we make sure each patient gets care that’s just right for them.
FAQ
What is a dysrhythmia, and how is it pronounced?
Dysrhythmia is a term for an irregular heartbeat. It’s pronounced as dis-rith-mee-uh.
What is the difference between dysrhythmia and arrhythmia?
Dysrhythmia and arrhythmia both describe irregular heart rhythms. The main difference is in how they’re said.
What are the common types of dysrhythmias?
Common types include atrial fibrillation and atrial flutter. Also, supraventricular tachycardia, ventricular tachycardia, ventricular fibrillation, and heart blocks.
What causes dysrhythmias?
Dysrhythmias can be caused by heart problems like coronary heart disease. Heart valve disorders also play a role. Non-heart issues and environmental factors, like electrolyte imbalances and certain meds, can also cause them.
How are dysrhythmias diagnosed?
Doctors use tools like electrocardiograms (ECGs) to diagnose dysrhythmias. They look at ECG patterns to understand the problem.
What are the medical implications of dysrhythmias?
Dysrhythmias, like atrial fibrillation, can lead to stroke, heart failure, and sudden death.
How are dysrhythmias treated?
Treatment options include medicines, catheter ablation, and devices like pacemakers and ICDs.
What lifestyle modifications can help manage dysrhythmia?
Making lifestyle changes can improve life for those with dysrhythmia. Understanding the condition is key.
When should someone seek emergency care for dysrhythmia?
It’s important to know when to seek emergency care. This is to avoid serious complications.
How can dysrhythmias be prevented?
Knowing the causes and risk factors helps in prevention. This includes genetic and environmental factors.
What is the role of ongoing research in managing dysrhythmias?
Research and innovation are vital. They help improve understanding and treatment of dysrhythmias, leading to better outcomes.
References
- O’Rourke, M. F. (2018). Structure and function of systemic arteries: reflections on the vascular wall and blood flow. Vascular Medicine, 23(4), 316-323. https://pubmed.ncbi.nlm.nih.gov/30016416/