Last Updated on November 25, 2025 by Ugurkan Demir
Dilated cardiomyopathy (DCM) makes the heart muscle weak. The heart chambers get bigger, making it hard to pump blood. At Liv Hospital, we provide complete care for DCM patients. It’s a top reason for heart failure and transplants.
Knowing about DCM is key for managing it well. We’ll look at important facts about DCM. This includes its causes, symptoms, how to diagnose it, and treatment choices. Our aim is to offer reliable, patient-focused care and the newest ways to handle cardiomiopatia dilatada and DCM heart disease.
Key Takeaways
- Dilated cardiomyopathy (DCM) is a condition where the heart muscle weakens and the chambers get bigger.
- DCM is a major cause of heart failure and heart transplants.
- Managing DCM well means knowing its causes, symptoms, diagnosis, and treatment options.
- Liv Hospital offers full care for DCM patients.
- Patient-centered care is essential for handling DCM effectively.
What Is an Enlarged Heart? DCM Explained
Dilated Cardiomyopathy (DCM) is a heart condition where the heart’s pumping ability is reduced. This happens because the heart’s chambers get bigger. In simple terms, the heart gets too big and can’t pump blood well.
Definition and Medical Terminology
DCM is a heart muscle disease. The term “cardiomyopathy” comes from Greek words. It means heart muscle disease. Dilated Cardiomyopathy is when the heart’s chambers get too big, making it hard to pump blood.
Doctors diagnose DCM when the heart’s chambers are too big and don’t pump well. This is without other heart problems like blockages or high blood pressure.
The Mechanics of Cardiac Dilation
The heart’s ventricles pump blood all over the body. In DCM, these ventricles get too big. This makes it hard for them to pump blood well.
This dilation causes problems, like heart failure. The heart can’t keep up with the body’s needs.
Understanding how DCM works is key to finding treatments. Knowing about DCM helps us see why early diagnosis and treatment are so important. Next, we’ll look at how common DCM is, what causes it, and its symptoms.
Key Fact #1: Prevalence and Epidemiology of DCM Heart Disease
It’s important to know about DCM heart disease for doctors and patients. Dilated cardiomyopathy (DCM) makes it hard for the heart to pump blood. This can lead to serious health problems.
Looking at global DCM numbers helps us understand its impact. Studies show DCM affects between 42 and 118 people per 100,000 adults. This range shows how different places and people can be affected differently.
Global Statistics and Incidence Rates
DCM is a big problem worldwide, affecting many adults. It’s a top reason for heart failure, which is a big challenge for health systems everywhere.
Many things can increase the chance of getting DCM. These include genes, environment, and other health issues. Knowing these helps us find better ways to help people.
Demographics: Who’s Most at Risk
Some groups are more likely to get DCM. Men are more at risk than women. It can happen at any age, but it’s more common in middle-aged people.
Other things that raise the risk include family history, high blood pressure, diabetes, and certain toxins or medicines. Spotting these risk factors early is key to managing the disease.
By knowing who’s most at risk, doctors can screen and prevent DCM better. This helps protect people’s health.
Key Fact #2: Genetic Origins of Dilated Cardiomyopathy
It’s important to know the genetic roots of Dilated Cardiomyopathy to spot risks early. About 20-40% of DCM cases run in families. This shows how genetics play a big role in its cause.
Hereditary Patterns in Primary Cardiomyopathy
DCM often follows an autosomal dominant pattern. This means just one mutated gene can cause the disease. It’s why some families see many members affected by DCM over time.
Familial DCM is when two or more family members have DCM, or a first-degree relative dies suddenly before 35. Spotting these patterns is key to catching and treating the disease early.
Common Genetic Mutations
Many genes are linked to DCM, like those for sarcomere, cytoskeleton, and nuclear envelope proteins. The TTN gene, which makes titin, is a top cause of DCM.
Other genes like LMNA, MYH7, and TNNT2 are also involved. This variety shows how complex DCM’s genetics are.
Family Screening Recommendations
For families with DCM history, screening is advised to find at-risk individuals. This includes clinical checks, echocardiograms, and ECGs.
If a harmful mutation is found, genetic tests can show if family members carry it. This info is key for managing and watching over them.
Family screening is suggested for those with a first-degree relative with DCM. This is more urgent if the relative was young or if there’s a history of sudden cardiac death.
Key Fact #3: Acquired Causes of Dilated Heart Disease
Genetics play a big role in Dilated Cardiomyopathy. But, we also need to look at the acquired causes. These are factors that come up over a person’s life, not passed down from parents.
Toxic and Medication-Induced DCM
Some toxins and medicines can harm the heart, leading to Dilated Cardiomyopathy. Alcohol is a known heart toxin, mainly for those who drink too much over time. Drugs like anthracyclines, used in chemotherapy, also raise the risk of DCM.
Other substances that might cause DCM include certain chemotherapeutic agents and illicit drugs like cocaine. They can damage heart cells directly or indirectly through metabolic pathways.
| Toxin/Medication | Mechanism of Action | Risk Factors |
| Alcohol | Direct cardiotoxicity | Chronic excessive consumption |
| Anthracyclines | Generation of free radicals | Cumulative dose, age |
| Cocaine | Coronary vasoconstriction, hypertension | Frequency and amount of use |
Infectious and Inflammatory Triggers
Infections and inflammation can also lead to DCM. Myocarditis, an inflammation of the heart muscle, often caused by viruses, is a known risk factor. This inflammation can cause scarring and heart dilation.
“Myocarditis is a significant cause of DCM, mainly in younger people. Early diagnosis and treatment are key to avoiding long-term heart damage.”
Dr. Jane Smith, Cardiologist
Bacterial infections and other pathogens can also cause DCM, with different mechanisms involved.
Metabolic and Nutritional Factors
Metabolic and nutritional issues can also contribute to DCM. For example, thiamine deficiency (beriberi) can lead to heart failure and DCM, often in those with poor diets or alcohol abuse.
Other metabolic factors, like obesity and diabetes, increase the risk of heart problems, including DCM. It’s important to manage these conditions through lifestyle changes and medical treatment.
Understanding the acquired causes of Dilated Cardiomyopathy is key to better prevention and treatment. By tackling these factors, healthcare providers can improve patient outcomes and quality of life.
Key Fact #4: Recognizing Symptoms of an Enlarged Heart
It’s important to know the signs of an enlarged heart to catch Dilated Cardiomyopathy early. We’ll cover the symptoms of DCM, from the first signs to serious heart failure signs.
Early Warning Signs
The early stages of DCM might show small symptoms that are easy to miss. Fatigue and dizziness are common signs, as the heart has trouble pumping blood. People might also feel short of breath when they’re active or lying down.
Swelling in the legs and feet, or edema, can happen because of fluid buildup.
Progressive Symptoms of Heart Failure
As DCM gets worse, symptoms get more serious. Shortness of breath can get worse, even when you’re not active. You might also cough or wheeze because of fluid in your lungs, called pulmonary congestion.
Fluid in the belly, or ascites, can also happen. This makes the belly swell.
Other signs include rapid or irregular heartbeats, or arrhythmias. These can be scary and need doctor’s help. You might also find it harder to do everyday things because of fatigue and weakness.
Emergency Warning Signs
Some symptoms mean you need to get help right away. Severe chest pain or discomfort could mean a heart attack. Severe shortness of breath or coughing up pink, frothy mucus is a sign of acute pulmonary edema and is a medical emergency.
Other urgent signs include fainting or near-fainting episodes. These happen when the brain doesn’t get enough blood. Rapid or irregular heartbeats that are severe or make you dizzy or faint also need quick doctor’s care.
Knowing these symptoms and when to get help is key to managing DCM well. If you or someone you know has any of these emergency signs, get medical help right away.
Key Fact #5: Diagnostic Journey for Dilated Cardiomyopathy
The journey to diagnose DCM is complex. It involves many medical steps to find out if you have it and how severe it is. Doctors use a mix of clinical checks, imaging, and lab tests to make a diagnosis.
Physical Examination Findings
Starting with a detailed physical check is key. Doctors look for signs of heart trouble like edema, jugular venous distension, or abnormal heart sounds. These signs might lead to more tests.
Imaging Technologies
Imaging is vital for spotting DCM. Echocardiography is often first, as it shows the heart’s shape and how well it pumps. Cardiac MRI might also be used for more detailed views of the heart.
Laboratory and Genetic Testing
Lab tests help find what might be causing DCM and check the heart’s health. Tests include blood tests for heart failure signs, infections, or genetic markers. Genetic tests might be suggested if there’s a family history of DCM.
Differential Diagnosis Considerations
Doctors must think of other conditions that could look like DCM. This includes other heart diseases, coronary artery disease, or valvular heart disease. They look at your medical history, physical check, and test results to make a correct diagnosis.
Diagnostic Criteria and Challenges
To diagnose DCM, doctors use specific criteria. They look for heart size and function issues without other causes like coronary disease. Even with new tech, it’s hard to tell DCM from other heart problems or find the cause.
| Diagnostic Tool | Purpose | Key Findings in DCM |
| Echocardiography | Assess heart structure and function | Dilated heart chambers, reduced ejection fraction |
| Cardiac MRI | Detailed assessment of heart anatomy and function | Detailed visualization of heart structure, fibrosis |
| Blood Tests | Identify signs of heart failure, infections, or genetic markers | Elevated BNP, abnormal electrolyte levels |
| Genetic Testing | Identify genetic mutations associated with DCM | Specific genetic mutations linked to DCM |
Key Fact #6: Treatment Approaches for Congestive Cardiomyopathy
Managing congestive cardiomyopathy needs a mix of treatments. We’ll look at the different ways to help patients with DCM.
Medication Strategies
Medicines are key in treating congestive cardiomyopathy. ACE inhibitors and beta-blockers help the heart work better. Diuretics also help by reducing fluid buildup.
ARNI (angiotensin receptor-neprilysin inhibitors) are used in some cases to boost heart function. The right medicine and dose depend on the patient’s needs.
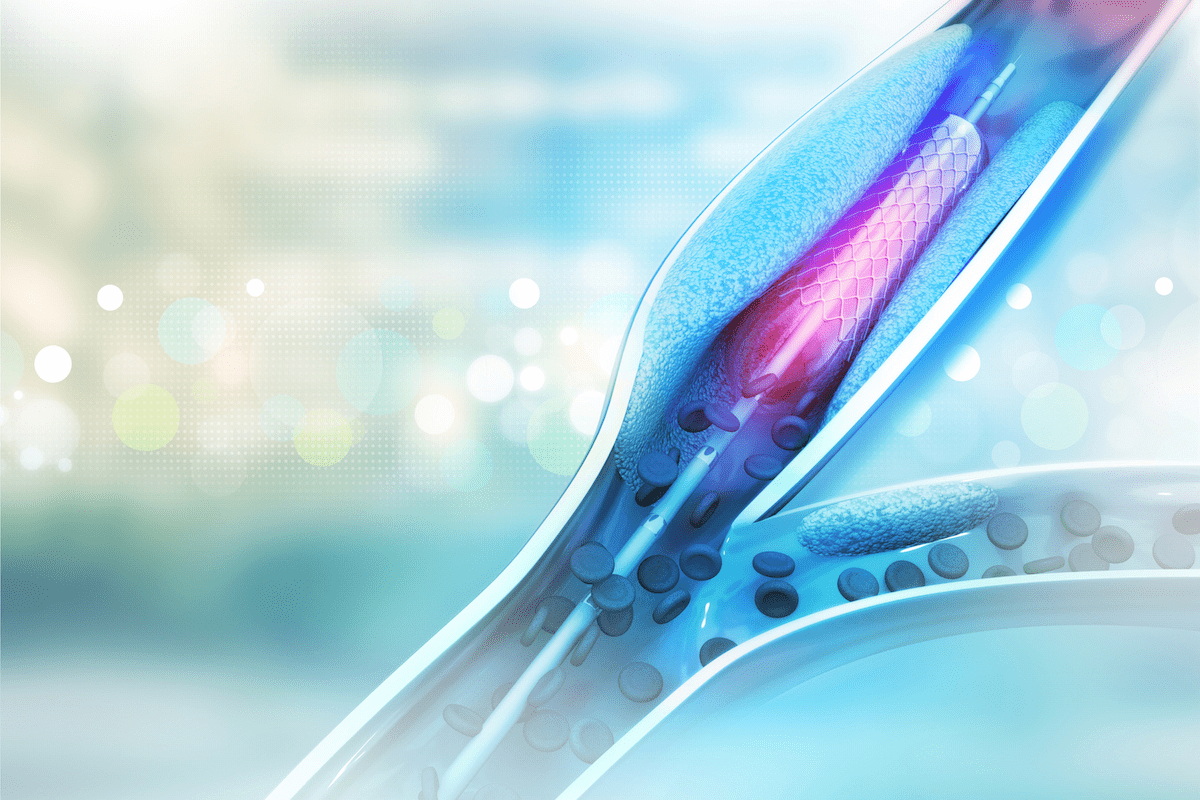
Device-Based Interventions
Some patients need devices to help their heart. Pacemakers and implantable cardioverter-defibrillators (ICDs) keep the heart rhythm steady. Cardiac resynchronization therapy (CRT) makes the heart pump better.
These devices help patients with heart failure feel better and live better lives.
Surgical Options
In severe cases, surgery might be needed. Heart transplantation is a lifesaver for those with failing hearts. Left ventricular assist devices (LVADs) are used as a temporary fix or long-term solution.
Surgery is for those who haven’t gotten better with medicine and devices.
Key Fact #7: Prognosis and Long-term Outlook with DCM Disease
The long-term outlook for DCM patients depends on several key factors. It’s important for both patients and healthcare providers to understand these factors. This knowledge helps in making informed decisions about treatment and management.
Factors Influencing Survival Rates
Several factors affect the survival rates of DCM patients. These include:
- The underlying cause of DCM, whether it’s genetic, infectious, or toxic
- The severity of the disease at diagnosis, including the extent of cardiac dysfunction
- The patient’s response to initial treatment and their ability to tolerate medications
- The presence of comorbidities, such as diabetes or hypertension
- The patient’s adherence to recommended lifestyle modifications and treatment plans
Early diagnosis and appropriate management can significantly improve survival rates. Modern treatments have shown that many DCM patients can see improved cardiac function and overall survival.
Quality of Life Considerations
While survival rates are important, quality of life is equally significant. Factors influencing quality of life include:
- Symptom severity and frequency
- Ability to perform daily activities and maintain independence
- Emotional and psychological well-being
- Social support systems and relationships
Healthcare providers work closely with patients to develop management plans. These plans aim to improve survival and enhance overall quality of life.
Monitoring Disease Progression
Regular monitoring is key in managing DCM effectively. This includes:
- Regular check-ups with healthcare providers
- Periodic echocardiograms and other imaging tests
- Monitoring for signs of worsening heart failure
- Adjusting treatment plans as necessary
By closely monitoring disease progression, healthcare providers can make timely interventions. This helps improve patient outcomes and quality of life.
Living with Dilated Cardiomyopathy: Daily Management
For those with DCM, daily life needs careful planning. This helps manage symptoms and improve life quality. Managing DCM involves several daily strategies.
Lifestyle Modifications
Changing your lifestyle is key in managing DCM. This includes eating right, exercising regularly, and managing stress. Eating a diet full of fruits, veggies, and whole grains can help manage symptoms.
- Reduce sodium intake to minimize fluid retention.
- Limit alcohol consumption, as it can exacerbate DCM symptoms.
- Maintain a healthy weight to reduce the heart’s workload.
It’s also important to exercise regularly. But, always talk to a doctor first to make sure it’s safe. Stress management, like meditation or yoga, can also help.
Emotional and Psychological Support
Living with DCM can affect your emotions and mind. Having a support system is vital. This can be family, friends, or a support group.
“Support groups can provide a sense of community and understanding that is invaluable for individuals living with DCM.”
— Dr. Jane Smith, Cardiologist
Also, seeing a mental health professional can help with anxiety and depression. These are common in people with chronic heart conditions. Staying positive and connected with loved ones can greatly improve your life.
| Support Strategy | Description | Benefits |
| Support Groups | Joining a group of individuals with DCM to share experiences. | Reduces feelings of isolation, provides emotional support. |
| Mental Health Professionals | Working with a therapist to manage anxiety and depression. | Improves mental health, enhances coping strategies. |
| Family and Friends | Maintaining strong relationships with loved ones. | Provides emotional support, practical help. |
Special Considerations: DCM in Specific Populations
Dilated Cardiomyopathy (DCM) affects different people in different ways. We need to tailor care for children, pregnant women, and the elderly. Each group faces unique challenges and needs special management.
Pediatric Dilated Cardiomyopathy
DCM in kids is different from adult cases. It can progress quickly. Treatment must match the child’s age and size.
Early diagnosis and treatment are key for kids with DCM. Genetic causes are common in children, so we must consider these when planning treatment.
Pregnancy and DCM
Pregnancy is risky for women with DCM. Pregnancy can make symptoms worse. Close monitoring is essential during and after pregnancy.
Women with DCM thinking about pregnancy should get preconception counseling. A team of doctors is needed to manage the condition during pregnancy.
Elderly Patients with Dilated Heart
Elderly patients with DCM often have other health issues. Age and other conditions make treatment more complex.
Medications for DCM can interact with other conditions common in the elderly. Device therapy and other advanced treatments must be adjusted for older patients.
Understanding DCM in these groups helps us give better care. This improves their health outcomes.
Global Perspectives on Cardiomiopatia Dilatativa
Looking at DCM worldwide shows how important international terms and treatment methods are. Dilated Cardiomyopathy, known differently around the world, makes diagnosis and treatment tricky.
International Terminology and Understanding
Different places call DCM by different names. For example, in some areas, it’s called “cardiomiopatia dilatativa,” while others just say “Dilated Cardiomyopathy.” This can cause confusion, like in international studies or when patients travel for care.
It’s key for doctors to know these differences. This way, patients get the right care, no matter where they are.
Regional Differences in Treatment Approaches
How DCM is treated also changes from place to place. It depends on local health policies, technology, and culture. For instance, some places focus more on medicines, while others use devices like ICDs.
- In Europe, doctors often follow strict treatment guidelines.
- In the United States, there’s a big use of advanced devices like ICDs and CRT.
- In developing countries, the goal is to make basic, affordable treatments available to more people.
These differences show we need to tailor DCM care to each area’s needs and resources.
By grasping global views on DCM, doctors can better care for patients from all over. This helps improve health outcomes for people with this condition everywhere.
Future Horizons: Research and Emerging Therapies
The treatment for Dilated Cardiomyopathy (DCM) is on the verge of a big change. New research and therapies are leading the way. These advancements will likely make treating DCM much better for patients.
Gene Therapy and Precision Medicine
Gene therapy is a major breakthrough in DCM treatment. It aims to fix the genetic problems that cause heart issues. Precision medicine is key here, as it tailors treatments to each person’s genes.
This mix of gene therapy and precision medicine is very promising. It could lead to more effective treatments with fewer side effects. This is because treatments are made just for each person.
Stem Cell and Regenerative Approaches
Stem cell therapy and regenerative medicine are also being explored for DCM. They aim to fix or replace damaged heart cells. Stem cell therapies have shown promise in early studies, suggesting they could be a future treatment.
These regenerative methods use stem cells to help the heart heal. While they’re not yet proven, they offer hope for DCM patients.
Novel Pharmacological Treatments
New medicines are also being developed for DCM. These drugs target specific parts of the disease process. They aim to be more effective and safer than current treatments.
Research on these new medicines is ongoing. Several are in clinical trials, showing promise. These emerging treatments could give patients and doctors more options.
Conclusion
Dilated cardiomyopathy (DCM) is a major cause of heart failure and heart transplants globally. Knowing the 7 key facts about DCM is vital for raising awareness and finding effective ways to manage it.
We’ve looked into what DCM is, how common it is, its causes, symptoms, how it’s diagnosed, and how it’s treated. Recognizing the need for early diagnosis and proper care can greatly improve the lives of those with DCM.
As we move forward in cardiology, staying updated on new research and treatments for DCM is key. This way, we can offer the best care and support to those dealing with DCM.
FAQ
What is dilated cardiomyopathy (DCM)?
Dilated cardiomyopathy is a heart condition. The heart muscle weakens, and the chambers get bigger. This makes it hard for the heart to pump blood well.
What are the symptoms of DCM?
Early signs of DCM include feeling very tired and short of breath. As the disease gets worse, you might notice swelling in your legs and ankles. Emergency signs are chest pain and trouble breathing.
How is DCM diagnosed?
Doctors use several steps to diagnose DCM. They look at physical signs, use imaging like echocardiography, and do lab and genetic tests. They also consider other possible conditions.
What are the treatment options for DCM?
Treatments for DCM include medicines to help manage symptoms and slow the disease. Doctors might also suggest devices like pacemakers. In some cases, a heart transplant is needed.
Can DCM be inherited?
Yes, DCM can run in families. Knowing about genetic links is important. It helps identify people at risk. Families with a history of DCM should get screened.
How can I manage DCM on a daily basis?
Managing DCM daily means making healthy choices. Eat well, exercise regularly, and get emotional support. These steps help cope with the condition.
Are there any new treatments on the horizon for DCM?
Yes, researchers are exploring new treatments. They’re looking into gene therapy, stem cells, and new medicines. These could offer better ways to manage DCM in the future.
How does DCM affect different populations?
DCM affects people differently, depending on their age or health status. Children, pregnant women, and older adults need special care. Their treatment plans must consider their unique needs.
What is the prognosis for someone with DCM?
The outlook for DCM varies. It depends on several factors, including survival rates and quality of life. Personalized care is key to managing the disease effectively.
Is DCM the same as heart failure?
No, DCM and heart failure are not the same. DCM is a condition where the heart muscle weakens. It can lead to heart failure, but they are distinct.
Can lifestyle changes help manage DCM?
Yes, making healthy lifestyle choices is important. It can help slow the disease and improve your quality of life.
References
- O’Rourke, M. F. (2018). Structure and function of systemic arteries: reflections on the vascular wall and blood flow. Vascular Medicine, 23(4), 316-323. https://pubmed.ncbi.nlm.nih.gov/30016416/