At Liv Hospital, we know how hard congestive heart failure (CHF) can be. CHF acute exacerbations happen when the body can’t keep up, leading to worse symptoms and more hospital visits. We’re dedicated to top-notch healthcare, helping patients from around the world with the latest treatments and support. Learn about chf acute exacerbation, its pathophysiology, etiology, and key clinical presentation facts.
We want to teach you about exacerbations of heart failure. We’ll look at how CHF works, why it happens, and how it shows up in patients. Our goal is to help you understand and manage this condition better.
Key Takeaways
- Understanding the pathophysiology of CHF is key to managing it well.
- Knowing what causes exacerbations helps prevent them.
- Spotting the signs of CHF exacerbations is important for quick action.
- Liv Hospital is all about quality care for CHF patients.
- We offer advanced treatments and support for patients from abroad.
Understanding CHF and Its Global Impact
Congestive heart failure (CHF) is a serious condition where the heart can’t pump blood well. This leads to many problems in the body. It happens when the heart is damaged or doesn’t work right.
Definition and Significance of CHF
CHF, or heart failure, means the heart can’t pump enough blood. This causes tiredness, swelling, and trouble breathing. It really affects a person’s life quality.
CHF is a big problem because it’s common, causes a lot of illness, and can be deadly. It’s a major health issue.
The definition of CHF covers many symptoms and causes. Knowing about CHF helps doctors find better ways to treat it and help patients.
Rising Incidence of Congestive Heart Failure
More and more people are getting CHF all over the world. This is because more people are living longer, and more are at risk because of things like high blood pressure and diabetes. It’s a big challenge for health care.
As more people get older, CHF will keep getting more common. This means health care will need to do more to help.
Impact of Population Aging on CHF Prevalence
Older people are more likely to get CHF. As people get older, their hearts change and they get more risk factors. So, CHF is becoming a bigger problem.
It’s important to understand how aging affects CHF. This helps health care plan better and use resources wisely.
Pathophysiology of CHF Acute Exacerbation
To understand CHF acute exacerbation, we must look at how the heart tries to keep up and fails. CHF happens when the heart can’t pump enough blood for the body’s needs.
Compensatory Mechanisms in Heart Failure
The body tries to keep the heart working by activating certain systems. The sympathetic nervous system makes the heart beat faster and stronger. The renin-angiotensin-aldosterone system (RAAS) helps keep fluid in and blood pressure up. But, these efforts can harm the heart over time, making heart failure worse.
Neurohumoral Activation and Its Consequences
Neurohumoral activation is key in CHF. It causes blood vessels to narrow, holds onto sodium, and makes the heart work harder. This can lead to the heart changing shape and function, making it less effective. Knowing this helps doctors find better ways to treat heart failure.
Transition from Compensated to Decompensated Heart Failure
When the heart’s backup systems fail, symptoms get worse quickly. This can happen due to not taking medicine, eating the wrong foods, or getting sick. Spotting these signs early is vital for quick action and stopping things from getting worse.
Common Etiologies of Heart Failure
Understanding the causes of congestive heart failure (CHF) is key to managing it well. CHF happens when the heart can’t pump blood properly. This is due to many reasons that harm the heart’s function.
Heart failure comes from several sources, like heart diseases and other health issues. Ischemic heart disease, hypertensive heart disease, valvular heart disease, and cardiomyopathies are the main culprits.
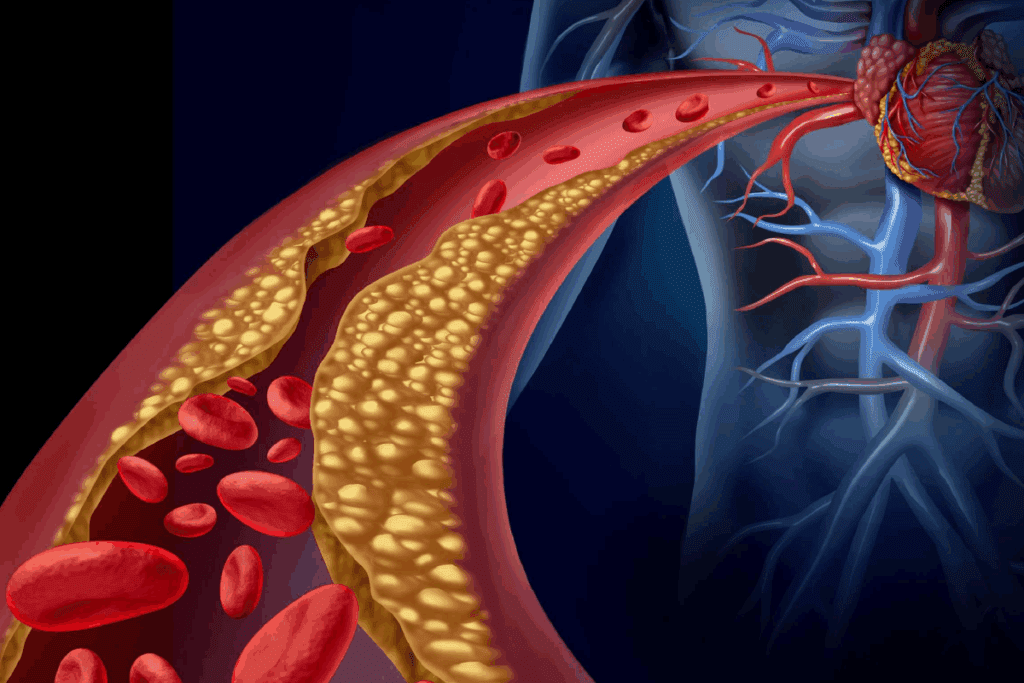
Ischemic Heart Disease
Ischemic heart disease, mainly from coronary artery disease, is the top cause of heart failure. It happens when blood flow to the heart muscle drops. This can cause a heart attack and lead to heart failure.
Hypertensive Heart Disease
Hypertensive heart disease comes from long-term high blood pressure. It makes the heart work too hard, leading to thickening of the left ventricle. This can cause heart failure.
Valvular Heart Disease
Valvular heart disease affects the heart valves. It can make the heart pump blood poorly, leading to heart failure.
Cardiomyopathies and Other Causes
Cardiomyopathies, like dilated, hypertrophic, and restrictive types, directly harm the heart muscle. This can lead to heart failure. Other causes include diabetes, obesity, and infections.
| Etiology | Pathophysiology | Clinical Impact |
| Ischemic Heart Disease | Reduced blood flow to the heart muscle | Myocardial infarction, heart failure |
| Hypertensive Heart Disease | Left ventricular hypertrophy due to high blood pressure | Heart failure, cardiac arrhythmias |
| Valvular Heart Disease | Impaired valve function | Heart failure, valve replacement needed |
| Cardiomyopathies | Disease of the heart muscle | Heart failure, arrhythmias |
Triggers of CHF Acute Exacerbation
Knowing what causes CHF acute exacerbation is key to better care. We must find and handle these causes to avoid hospital stays and better patient results.
Medication Non-Adherence and Dietary Indiscretion
Not taking medicine as told and eating too much salt are big problems. Not taking medicines like diuretics and ACE inhibitors can hurt the heart fast. Eating too much salt can also make fluid build up and make symptoms worse.
We need to teach patients how important it is to take their medicines and eat right. They should eat less than 2 grams of salt a day and drink less water.
Arrhythmias and Acute Coronary Syndromes
Arrhythmias like atrial fibrillation and heart attacks can make CHF worse. Arrhythmias can lower how well the heart pumps, and heart attacks can damage the heart more.
We must spot and treat these problems quickly. We suggest keeping an eye on the heart of patients at risk and acting fast when arrhythmias or heart attacks happen.
Infections and Inflammatory Conditions
Infections and inflammatory diseases can also make CHF worse. Infections like pneumonia can make the body work harder and put more stress on the heart.
We should try to stop infections with vaccines and treat them early. We also need to manage inflammatory diseases well to lower the chance of CHF getting worse.
Other Precipitating Factors
Other things that can make CHF worse include high blood pressure, blood clots in the lungs, and low blood count. High blood pressure can make the heart work too hard, while blood clots and low blood count can make it hard for tissues to get enough oxygen.
We must watch blood pressure closely, treat blood clots fast, and fix low blood count to stop CHF from getting worse.
Clinical Presentation of CHF Acute Exacerbation
It’s key to know how CHF acute exacerbation shows up to catch it early and treat it right. The signs and symptoms can differ a lot from person to person. So, doctors need to be ready for all kinds of symptoms.
Pulmonary Symptoms and Signs
Pulmonary symptoms are a big deal in CHF acute exacerbation. People often have dyspnea, which can be mild or very severe. They might also cough up frothy or pink sputum and hear wheezing.
Doctors might hear crackles or rales when listening to the lungs. This means there’s fluid in the lungs. In bad cases, patients might use extra muscles to breathe and not get enough oxygen.
Systemic Manifestations
CHF acute exacerbation also shows up in other ways. Fatigue and weakness are common because the heart isn’t pumping well. Many people also get swelling in their legs and feet.
Other signs include jugular venous distension and hepatojugular reflux. These show the heart is not working right. Some people might not want to eat or feel pain in their belly because of liver problems.
Variations in Presentation Based on Heart Failure Type
The way CHF shows up can change based on the heart failure type. For example, left-sided heart failure often means more lung problems. Right-sided failure might show up as more swelling and jugular venous distension.
Also, the cause of CHF can affect how it presents. Ischemic cardiomyopathy might cause chest pain. Valvular heart disease might have specific heart sounds.
Knowing these differences helps doctors give better care. By understanding all the ways CHF acute exacerbation can show up, doctors can treat each patient more effectively.
Diagnostic Criteria and Evaluation
Diagnosing CHF involves clinical evaluation, biomarker analysis, and imaging studies. These methods give a full picture of the condition.
Clinical Assessment and Physical Examination
Diagnosing CHF starts with a detailed clinical assessment. We look at the patient’s medical history for signs of heart failure. This includes symptoms like jugular venous distension, pulmonary rales, and peripheral edema.
The physical exam can show these signs. They are key indicators of CHF.
Laboratory Biomarkers
B-type natriuretic peptide (BNP) and N-terminal pro b-type natriuretic peptide (NT-proBNP) are important biomarkers. High levels of these biomarkers suggest heart failure. They help tell if symptoms come from the heart or not.
Imaging Studies
Imaging studies like echocardiography and chest radiography are vital. They help check the heart’s structure and function. Echocardiography shows how well the left ventricle works and if there are any problems with the valves.
Chest radiography can spot signs of lung congestion and an enlarged heart.
NIH and Evidence-Based Diagnostic Criteria
The National Institutes of Health (NIH) and other groups have set guidelines for diagnosing CHF. These guidelines stress the need for a thorough approach. This includes clinical assessment, biomarker analysis, and imaging studies.
Following these guidelines helps ensure accurate diagnosis and proper treatment of CHF.
By using these diagnostic tools together, we can accurately diagnose CHF. Then, we can create a treatment plan that meets each patient’s needs.
Management Strategies for CHF Acute Exacerbation
Managing CHF acute exacerbation is vital to reduce illness and death. We will look at how to manage this condition. This includes initial steps, medicines, and advanced treatments for hard cases.
Initial Stabilization Approaches
The first step in managing CHF acute exacerbation is to stabilize the patient. This means using oxygen therapy, diuretics, and vasodilators. These help ease symptoms and improve heart function.
Using non-invasive ventilation is also key. It helps avoid the need for a ventilator.
| Therapy | Purpose | Benefits |
| Oxygen Therapy | Improve oxygenation | Reduces hypoxemia, alleviates dyspnea |
| Diuretic Administration | Reduce fluid overload | Decreases pulmonary congestion, improves symptoms |
| Vasodilator Therapy | Reduce ventricular preload and afterload | Improves cardiac output, reduces myocardial oxygen demand |
Pharmacological Interventions
Medicines play a big role in treating CHF acute exacerbation. We start with loop diuretics to reduce fluid. We also use ACE inhibitors or ARBs to fight neurohumoral activation.
In severe cases, inotropic agents might be needed for patients with low blood pressure or shock.
Advanced Therapies for Refractory Cases
For those not helped by initial treatments, we consider advanced options. This includes mechanical circulatory support like pumps or assist devices. We also use ultrafiltration to remove extra fluid.
In some cases, heart transplantation is an option for those with severe heart failure.
Prevention of Recurrent CHF Acute Exacerbation
Stopping CHF acute attacks is key in managing chronic heart failure. It needs a full plan. This includes better management of heart failure, teaching patients, and using self-care. Also, working with a team of healthcare experts is important.
Optimizing Chronic Heart Failure Management
Managing chronic heart failure well is the first step to avoid acute attacks. Here are some important steps:
- Medication Adherence: It’s vital for patients to take their medicines as told. This includes ACE inhibitors, beta-blockers, and diuretics.
- Regular Monitoring: Keeping up with regular check-ups and watching how patients do helps spot problems early.
- Lifestyle Modifications: Helping patients change their diet and get more exercise can really help manage CHF.
By focusing on these areas, doctors can lower the chance of acute attacks and help patients do better.
Patient Education and Self-Care Strategies
Teaching patients about their heart failure is very important. When patients know how to manage their condition, they can catch problems early. Key things to teach include:
- Why taking medicines as directed is so important
- How to spot when heart failure is getting worse
- How to manage diet and fluids
By teaching patients, we can help them manage their heart failure better.
Role of Multidisciplinary Care Teams
Using a team of healthcare experts is key for caring for CHF patients. This team might include cardiologists, primary care doctors, nurses, dietitians, and more. The benefits are:
- Getting care that covers all health needs
- Better communication among doctors
- More support and education for patients
Together, these teams can stop CHF attacks from coming back and improve care for patients.
Conclusion: Future Directions in CHF Management
We are making progress in understanding and treating congestive heart failure (CHF). It’s key to know the different causes and how we diagnose and treat it.
Our approach to managing CHF is changing. This is thanks to new research and better treatment options. The latest studies on congestive heart failure statpearls are helping us a lot.
We aim to provide top-notch healthcare to everyone, including international patients. Our goal is to make CHF management both new and focused on the patient.
By improving how we manage CHF, teaching patients, and working together as a team, we can make a big difference. This will help patients and reduce the impact of CHF.
Looking ahead, we need to keep finding new ways to treat CHF. We must also support patients at every step of their care.
FAQ
What is CHF acute exacerbation?
CHF acute exacerbation is when heart failure symptoms get worse suddenly. It often means the patient needs to go to the hospital right away.
What are the common etiologies of heart failure?
Heart failure can be caused by several things. These include heart disease from blocked arteries, high blood pressure, problems with heart valves, and muscle diseases of the heart.
What triggers CHF acute exacerbation?
Several things can make heart failure symptoms worse. These include not taking medicine as told, eating too much salt, irregular heartbeats, heart attacks, infections, and inflammation.
How is CHF acute exacerbation diagnosed?
Doctors use several ways to figure out if someone has a heart failure crisis. They look at symptoms, blood tests, images of the heart, and follow guidelines from the National Institutes of Health.
What are the management strategies for CHF acute exacerbation?
To manage heart failure crises, doctors first try to stabilize the patient. Then, they use medicines and advanced treatments for severe cases.
How can recurrent CHF acute exacerbation be prevented?
To stop heart failure crises from happening again, it’s important to manage heart failure well. This includes educating patients, teaching them how to take care of themselves, and working with a team of healthcare professionals.
What is the pathophysiology of CHF?
Heart failure happens when the heart can’t keep up with the body’s needs. This leads to changes in the heart and body, making it harder to breathe and pump blood.
What is the impact of population aging on CHF prevalence?
As more people get older, heart failure becomes more common. This puts a big strain on healthcare systems around the world.
What are the clinical presentations of CHF acute exacerbation?
Symptoms of a heart failure crisis include trouble breathing and signs of fluid buildup. They can also vary based on the type of heart failure.
References
National Center for Biotechnology Information. (2025). 7 Key Facts About CHF Acute Exacerbation Pathophysiology. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2646079/







