
Acute coronary syndrome (ACS) is a serious heart condition that needs quick action. At Liv Hospital, we know how vital it is to act fast to save lives.Learn acs symptoms and risk factors you need to know for diagnosis and prevention of complications.
ACS is a medical emergency where blood flow to the heart drops suddenly. This usually happens when a coronary artery gets blocked. Signs include chest pain, trouble breathing, and feeling dizzy.
Knowing the risk factors and warning signs is key to getting help fast. We think knowing the facts is the first step to caring for your heart.
Key Takeaways
- ACS is a medical emergency requiring immediate attention.
- Common signs include chest pain, shortness of breath, and dizziness.
- Understanding risk factors is vital for timely action.
- Spotting warning signs can save lives.
- Being informed is the first step to heart health.
Understanding Acute Coronary Syndrome: A Life-Threatening Cardiac Emergency
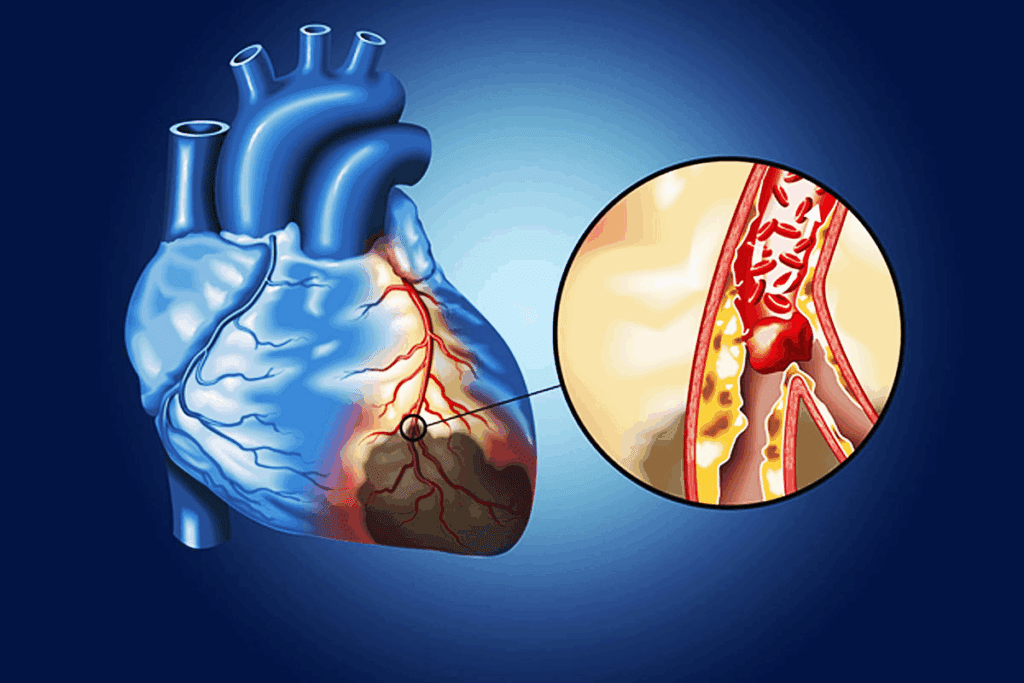
Acute coronary syndrome (ACS) is a serious heart emergency that needs quick medical help. It happens when blood flow to the heart muscle suddenly stops. This can lead to life-threatening conditions like heart attacks and unstable angina.
The Spectrum of ACS Conditions
ACS covers a range of heart emergencies, from unstable angina to heart attacks. Unstable angina means the heart doesn’t get enough blood and oxygen, which can lead to a heart attack. A heart attack, or myocardial infarction, happens when a blockage cuts off blood flow to the heart for too long, damaging or killing heart muscle.
Key ACS Conditions:
- Unstable Angina
- Non-ST-Elevation Myocardial Infarction (NSTEMI)
- ST-Elevation Myocardial Infarction (STEMI)
How ACS Affects Heart Blood Flow
The heart needs a steady supply of oxygen and nutrients to work right. These are delivered through the coronary arteries. ACS happens when these arteries get blocked by a blood clot on top of a plaque. This greatly reduces or stops blood flow to the heart.
Without enough oxygen, the heart muscle can get damaged or die, leading to a heart attack. The severity of ACS on the heart depends on how long and how much the blockage is.
| ACS Condition | Description | Impact on Heart Blood Flow |
| Unstable Angina | Reduced blood flow to the heart | Partial blockage |
| NSTEMI | Partial blockage causing damage | Significant reduction |
| STEMI | Complete blockage causing significant damage | Complete stoppage |
Why Immediate Medical Attention Matters
Getting medical help right away is key in managing ACS. The American Heart Association (AHA) says quick action can save lives and prevent long-term heart damage.
We stress the need to spot ACS symptoms early and get emergency care. The AHA’s ACS management guidelines highlight the importance of fast assessment and treatment. This includes using medicines to dissolve clots and procedures like angioplasty to open blocked arteries.
The 5 Critical ACS Symptoms You Should Never Ignore
Knowing the signs of ACS can save lives. Acute Coronary Syndrome (ACS) is a serious heart issue that needs quick medical help. We’ll cover the main symptoms to watch for, so you can act fast.
Chest Pain (CPx): The Cardinal Warning Sign
Chest pain is often the first sign of ACS. It can feel like pressure, squeezing, or a heavy feeling. Don’t ignore chest pain, as it might mean a heart attack is coming.
Pain Radiation Patterns: Beyond the Chest
Pain from ACS can spread to the arms, back, neck, jaw, or stomach. It might feel like a dull ache or sharp pain. It’s not just chest pain; pain can spread.
Breathing Difficulties and Respiratory Distress
Shortness of breath is a key symptom of ACS. People might find it hard to breathe or feel like they’re suffocating. Act fast if someone has trouble breathing badly.
Gastrointestinal Symptoms: Nausea and Vomiting
Nausea and vomiting can also signal ACS. These stomach issues might seem minor but can be serious if other symptoms are present.
Other signs include sudden heavy sweating, a racing heartbeat, feeling lightheaded or dizzy, and fainting. These need quick medical help, as fast action can save lives.
- Chest pain or discomfort
- Pain radiating to other areas
- Shortness of breath
- Nausea and vomiting
- Sweating, dizziness, or fainting
Knowing these 5 key ACS symptoms can help you get medical help quickly. This could save lives.
How ACS Symptoms Differ Between Men and Women
ACS symptoms can show up differently in men and women. It’s key to know these differences for the best care. While both can have chest pain, women often have atypical symptoms that make it harder to diagnose.
Classic vs. Atypical Presentation Patterns
ACS symptoms fall into two groups: classic and atypical. Classic symptoms, like chest pain that spreads to the arm or jaw, are more common in men. Women, on the other hand, often experience shortness of breath, nausea, and fatigue. Knowing these patterns helps doctors make the right diagnosis.
Women, older adults, and those with diabetes tend to have atypical symptoms. These symptoms can be subtle and might not seem like ACS at first. This can cause delays in getting the right treatment.
Why Women’s Symptoms Are Often Misdiagnosed
Women’s ACS symptoms are often missed or not taken seriously. This is partly because ACS is seen as a male condition. Also, women’s symptoms can be more complex and not fit the usual ACS picture. This shows the need for increased awareness among doctors about these gender differences.
Studies also show women are less likely to get timely and right treatment for ACS. This is partly because their symptoms are not recognized quickly. It’s critical for doctors to get education and training to handle ACS in women well.
Age-Related Variations in Symptom Presentation
Age also plays a big role in how ACS symptoms show up. Older adults, regardless of gender, often have atypical symptoms like confusion, dizziness, and loss of consciousness. These symptoms can make diagnosis harder because they might seem like other conditions.
It’s important to understand how age, gender, and symptoms interact for the best care. Doctors need to be careful and think of ACS when older adults and women have unexplained or atypical symptoms.
By knowing these differences and the various ways ACS can present, we can improve diagnosis and treatment. This leads to better health outcomes for everyone.
Major Risk Factors That Increase Your ACS Danger
ACS risk is shaped by age, lifestyle, and medical history. Knowing these factors helps spot high-risk individuals. It also guides preventive actions.
Age and Gender: Who’s Most Vulnerable
Age is a big risk factor for ACS. The risk grows after 45 for men and 55 for women. Men face higher risks, but women’s risk goes up after menopause.
Hypertension: The Silent Contributor
Hypertension, or high blood pressure, is a major ACS risk. It damages coronary arteries, making them prone to blockage. Controlling blood pressure through lifestyle and medication is key to lowering ACS risk.
Diabetes and Metabolic Disorders
Diabetes is a big risk factor for ACS. People with diabetes are more likely to get atherosclerosis. This condition builds up plaque in arteries, leading to ACS. Managing diabetes and metabolic disorders can reduce this risk.
Family History and Genetic Predisposition
A family history of heart disease raises ACS risk. If a first-degree relative had a heart attack young, you’re at higher risk. Genetic factors can influence high cholesterol and hypertension.
Understanding ACS risk factors helps individuals work with healthcare providers. Together, they can create a plan to lower risk. This might include lifestyle changes, managing health conditions, and preventive medication.
Lifestyle-Related Risk Factors for Acute Coronary Syndrome
Many lifestyle choices can increase the risk of Acute Coronary Syndrome. By changing these habits, we can lower our risk of ACS.
Smoking and Tobacco Use
Smoking is a big risk for ACS. Tobacco use harms the heart and blood vessels. Quitting can greatly lower this risk.
Tobacco smoke damages blood vessel linings, making them more likely to block. Cessation programs and support groups help people quit.
Diet and Cholesterol Levels
Eating too much saturated fat, cholesterol, and sodium raises ACS risk. Eating a balanced diet with fruits, veggies, and whole grains keeps cholesterol healthy.
It’s key to limit cholesterol and keep a healthy weight. Nutritional counseling offers personalized advice for heart-healthy eating.
Physical Inactivity and Obesity
Being inactive and overweight or obese are big risks for ACS. Regular exercise improves heart health.
Doing at least 150 minutes of moderate exercise or 75 minutes of vigorous exercise weekly helps. Exercise programs tailored to you can help you stick with it.
Stress and Psychological Factors
Long-term stress and some mental health issues can lead to ACS. Managing stress with techniques like meditation or deep breathing helps.
It’s also important to deal with mental health issues like depression and anxiety. Mental health support from experts is key for heart health.
American Heart Association (AHA) Guidelines for ACS Management
The American Heart Association (AHA) has set clear guidelines for managing Acute Coronary Syndrome (ACS). These guidelines focus on quick diagnosis and treatment. They are key for healthcare teams to give the best care to ACS patients.
Managing ACS well means spotting it early, using the right tests, and treating it based on evidence. The AHA’s guidelines are essential. They help make sure patients get the top care possible.
Current Diagnostic Protocols
Spotting ACS quickly and right is vital. The AHA says to use a mix of clinical checks, ECGs, and blood tests to diagnose it. High-sensitivity troponin assays are highlighted for catching heart attacks early.
| Diagnostic Tool | Description | Significance in ACS Diagnosis |
| ECG | Electrocardiogram to assess heart rhythm and detect ischemia or infarction. | Critical for identifying STEMI and NSTEMI. |
| Cardiac Biomarkers | Proteins released into the blood when heart muscle is damaged. | Troponin levels are key in diagnosing myocardial infarction. |
| Clinical Assessment | Evaluation of patient symptoms and medical history. | Essential for risk stratification and guiding treatment. |
Evidence-Based Treatment Approaches
Treatment for ACS follows proven methods. These aim to get blood flowing to the heart, lessen ischemia, and stop more heart damage. The AHA suggests early invasive strategies for high-risk patients. For others, the best treatment is medical therapy.
Recent Updates in ACS Care Standards
The AHA keeps updating its guidelines with new research and practices. Recent changes highlight the need for potassium and magnesium management in ACS treatment.
The Critical Timeline for Intervention
Acting fast is key in ACS care. The AHA says STEMI patients should get primary PCI within 90 minutes of first medical contact. For NSTEMI, high-risk patients should get an early invasive strategy.
In summary, the AHA’s ACS management guidelines offer a detailed plan for healthcare teams. By sticking to these guidelines, we can better care for ACS patients and lessen its impact.
Emergency Response: What to Do When ACS Symptoms Strike
When ACS symptoms hit, every second is critical. Knowing how to act can save lives. Acute Coronary Syndrome is a serious medical emergency that needs quick action.
Recognizing the Emergency: When to Call 911
If you or someone with you has ACS symptoms like chest pain, call 911 right away. Don’t try to drive to the hospital yourself. It can make things worse and risk your safety and others.
It’s vital to act fast. Quick medical help is key to managing ACS and protecting the heart.
First Aid Measures While Awaiting Help
While waiting for help, there are steps you can take. Stay calm. If someone is showing symptoms, help them sit or lie down comfortably.
If they’re awake and can, ask them to cough hard and often. But don’t wait to call 911.
The Golden Hour: Why Minutes Matter
The first hour after ACS symptoms start is called the “golden hour.” It’s a critical time. Quick medical care can greatly improve outcomes by reducing heart damage.
Acting fast in this hour can be a matter of life and death. It’s why recognizing symptoms and acting quickly is so important.
What to Tell Emergency Responders
When help arrives, give them all the details you can. Talk about the symptoms, any past health issues, and current medications.
Having this info ready can help responders give the best care right away.
Prevention Strategies for Those at High Risk
For those at high risk of Acute Coronary Syndrome (ACS), prevention is key. It’s not just about managing symptoms. It’s about making lifestyle changes and managing risk factors. Regular screenings are also important.
Lifestyle Modifications That Save Lives
Lifestyle changes are vital for preventing ACS. Start with a heart-healthy diet full of fruits, veggies, whole grains, and lean proteins. Cut down on saturated fats, cholesterol, and sodium.
- Regular physical activity is essential. Aim for 150 minutes of moderate exercise or 75 minutes of vigorous exercise weekly.
- Smoking cessation is critical, as smoking greatly increases ACS risk.
- Maintain a healthy weight to avoid obesity-related issues.
- Stress management is important. Try meditation, yoga, or deep breathing exercises.
Medical Management of Risk Factors
Medical management is often needed for high-risk individuals. It helps control risk factors that lifestyle changes can’t manage alone. This may include:
- Hypertension management through medication and lifestyle adjustments.
- Diabetes management to keep blood glucose levels in check.
- Cholesterol management using statins or other therapies.
| Risk Factor | Lifestyle Intervention | Medical Management |
| Hypertension | Dietary changes, exercise | Antihypertensive medication |
| High Cholesterol | Dietary changes, exercise | Statins, lipid-lowering therapy |
| Diabetes | Dietary changes, exercise | Glucose-lowering medication, insulin therapy |
Screening Recommendations by Age and Risk Level
Screening for cardiovascular risk factors is vital for ACS prevention. Recommendations depend on age and risk level. For example:
- Those with a family history of early heart disease should start screening early.
- People with many risk factors may need more frequent screenings.
Working With Your Healthcare Provider
Working closely with a healthcare provider is essential for high-risk individuals. Regular check-ups and personalized advice help tailor prevention strategies.
By following a complete prevention plan, high-risk individuals can lower their ACS risk. This plan includes lifestyle changes, medical management, and regular screenings.
Conclusion: Empowering Yourself Against ACS
Learning about Acute Coronary Syndrome (ACS) and its causes helps people get help fast. Knowing the signs and risks is key to fighting ACS. This knowledge lets acs patients take steps to lower their risk.
We’ve talked about ACS, why quick medical help is vital, and how lifestyle affects ACS risk. Knowing ACS symptoms and risks helps patients get help on time. This can lead to better health outcomes.
Teaching people about ACS is important. It helps them spot warning signs and get help quickly. Working with doctors and making healthy choices can lower ACS rates. Education is the core of managing ACS well.
FAQ
What is Acute Coronary Syndrome (ACS)?
Acute Coronary Syndrome (ACS) is a condition where blood flow to the heart suddenly drops. It includes heart attacks and unstable angina.
What are the symptoms of ACS?
Symptoms of ACS include chest pain or discomfort. You might also feel pain in your arms, back, neck, jaw, or stomach. Shortness of breath, nausea, or vomiting are other signs.
How do ACS symptoms differ between men and women?
Men often feel chest pain. Women might experience shortness of breath, nausea, or fatigue. These symptoms can delay diagnosis.
What are the major risk factors for developing ACS?
Risk factors for ACS include age and high blood pressure. Diabetes, family history, smoking, and high cholesterol are also important. Being inactive is another risk.
How can lifestyle modifications reduce the risk of ACS?
Quitting smoking and eating healthy can help. Regular exercise and managing stress are also key. These changes can lower your risk of ACS.
What are the American Heart Association guidelines for ACS management?
The American Heart Association stresses quick diagnosis and treatment. This includes using ECGs and troponin levels. Treatments like angioplasty and thrombolysis are recommended.
What should I do if I or someone else is experiencing ACS symptoms?
Call 911 if you or someone else has ACS symptoms. Stay calm while waiting. If the person is not breathing or has no pulse, start CPR if you can.
How can individuals at high risk of ACS prevent it?
High-risk individuals should work with their doctor to manage risk factors. Adopting a healthy lifestyle and following screening guidelines can help prevent ACS.
What is the importance of the “golden hour” in ACS treatment?
The “golden hour” is the first hour after ACS symptoms start. Quick medical help during this time can greatly improve outcomes and lower death rates.
How often should I get screened for risk factors if I have a family history of heart disease?
If you have a family history of heart disease, talk to your doctor about screenings. You may need regular checks for blood pressure, cholesterol, and diabetes.
References:
National Center for Biotechnology Information. (2025). 5 Key ACS Symptoms and Risk Factors You. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11287626



































