Last Updated on October 31, 2025 by Batuhan Temel
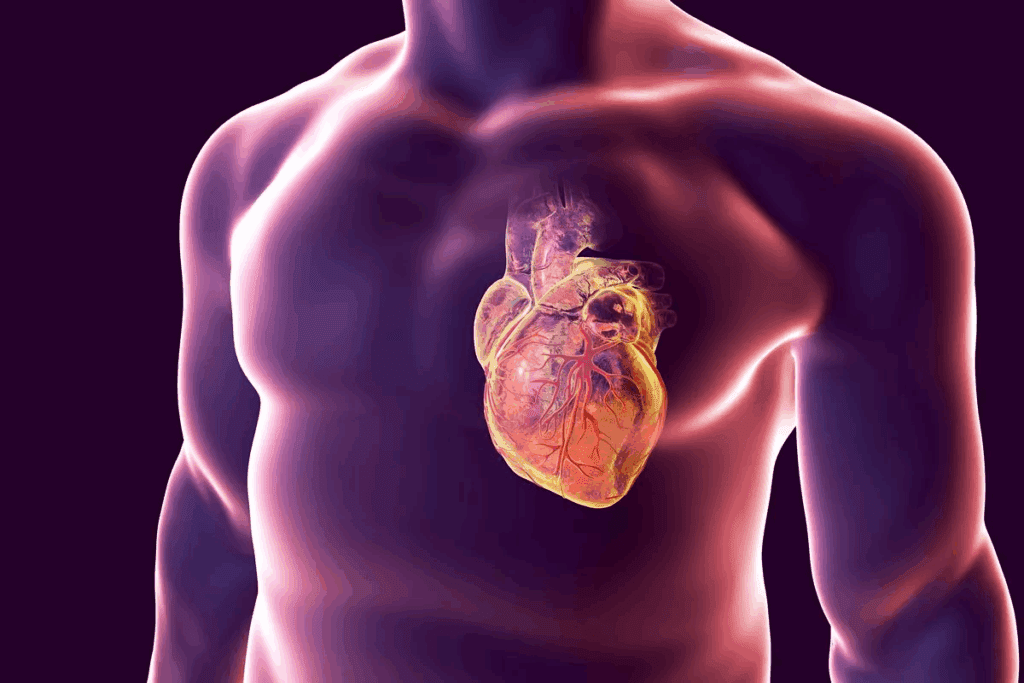
Acute coronary syndrome (ACS) is a serious condition where blood flow to the heart suddenly drops. This can cause chest pain or discomfort. At Liv Hospital, we know how important it is to spot the signs and risk factors of ACS.Explore acs heart signs, risk factors, and what to watch for in patients with acute coronary syndrome.
ACS includes a heart attack and unstable angina, which is chest pain. It’s vital to understand these to get help quickly. We aim to provide top-notch healthcare, supporting international patients with international standards.
Acute Coronary Syndrome (ACS) is a group of heart issues. They can cause serious problems if not treated quickly.
ACS includes heart attacks and unstable angina. These are serious because they block blood flow to the heart. This can damage or kill heart tissue.
Myocardial Infarction (MI), or heart attack, happens when heart blood flow stops. This damages or kills heart muscle. Unstable Angina means the heart doesn’t get enough blood. It causes chest pain but doesn’t kill heart tissue.
“The early diagnosis and treatment of ACS can significantly improve outcomes by restoring blood flow to the affected area of the heart.”
Quickly spotting ACS symptoms is key. Early treatment can greatly help. The sooner you act, the less damage to the heart.
ACS symptoms include chest pain or discomfort. This can feel like pressure or tightness in the chest. It might spread to the arms, back, neck, jaw, or stomach. Other signs are shortness of breath, nausea, vomiting, dizziness, and feeling very tired. The term for chest pain in medical terms is ‘CP’.
Seeing these signs early and getting help fast is critical. Knowing these symptoms and acting quickly can save lives. We stress the need to be aware and act fast.

It’s important to know how acute coronary syndrome works to help patients quickly. ACS happens when the heart muscle doesn’t get enough blood. This usually happens because of a blockage in the coronary arteries.
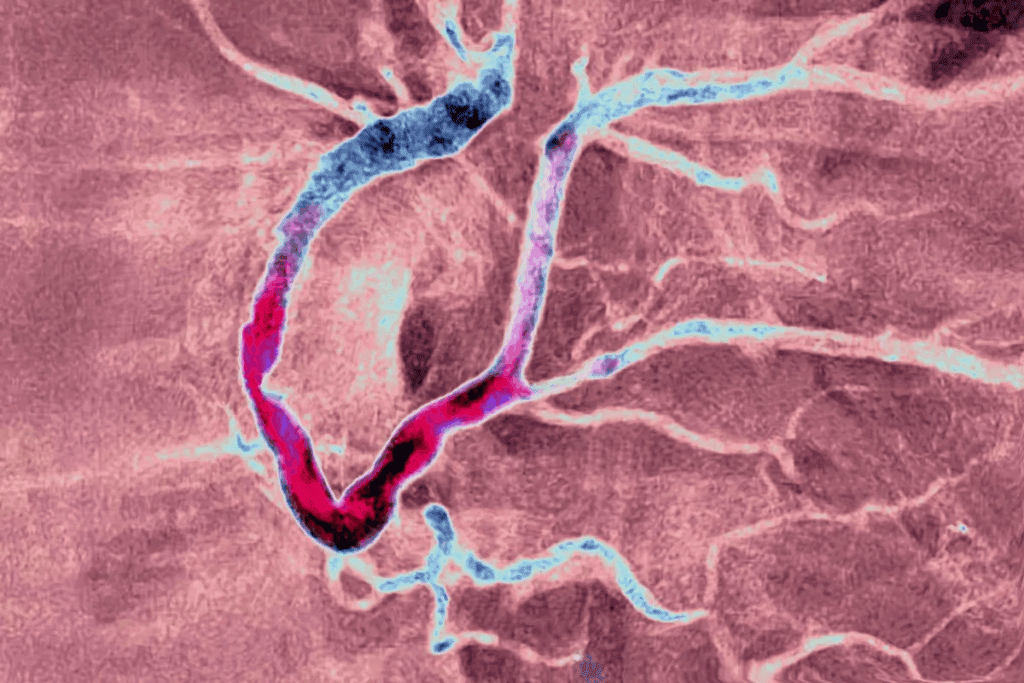
Atherosclerosis plays a big role in ACS. It’s when fatty deposits, or plaques, build up in the heart’s arteries. If a plaque bursts, it can cause a blood clot. This clot might block blood flow to the heart.
Atherosclerosis gets worse over time. It can be caused by high blood pressure, high cholesterol, and smoking.
When a plaque bursts, it exposes blood to a very sticky material. This can start a blood clot in the coronary artery. This clot can block the artery, causing myocardial ischemia or infarction.
The clotting process is complex. It involves platelets getting active, sticking together, and starting the coagulation cascade.
Myocardial ischemia happens when the heart doesn’t get enough blood. This means it can’t get enough oxygen. If this goes on for too long, it can cause a heart attack.
Understanding how ACS works is key to treating it right. Knowing the pathophysiology helps doctors give the best care. This can lead to better outcomes for patients.
Knowing the top 10 signs and symptoms of ACS is key for both doctors and patients. Acute Coronary Syndrome (ACS) is a serious condition where blood flow to the heart suddenly stops. Spotting these symptoms early can greatly improve treatment outcomes.
Chest pain or discomfort is the most common sign of ACS. This pain feels like pressure or tightness in the chest and can spread to other areas. It’s important to remember that chest pain can feel different for everyone.
Pain from ACS can spread to the arms, jaw, or back. This happens because these areas share nerve paths with the heart. People often describe this pain as a dull ache or feeling of heaviness.
Shortness of breath, or dyspnea, is a critical symptom of ACS. It can happen with or without chest pain and often means the heart is not working well. Dyspnea in ACS can be a sign of heart failure or severe ischemia.
Nausea and vomiting are common symptoms of ACS, more so in women and diabetic patients. These symptoms can be mistaken for stomach problems, which can delay getting a diagnosis.
Other symptoms of ACS include:
Symptoms of ACS can differ a lot between people. Women and diabetic patients might have more unusual symptoms, making it harder to diagnose on time.
Spotting these signs and symptoms early is vital for managing ACS well. By knowing how ACS can present differently, both doctors and patients can act quickly. This can save lives.
It’s important to know about atypical ACS symptoms, mainly in women, diabetic patients, and the elderly. Classic symptoms like chest pain are well-known, but atypical symptoms can make diagnosis harder. We need to be aware of these variations to give the best care.
Women with ACS often show different symptoms than men. They might feel short of breath, nauseous, or tired. Unlike men, they are less likely to have chest pain as their main symptom.
This difference can cause delays in getting the right treatment. Doctors need to watch for these atypical symptoms in women. Early action is key to better outcomes.
Diabetic patients often have atypical ACS symptoms. Diabetes can make it hard to feel pain, including ACS pain. This means they might have a “silent” heart attack without any symptoms.
It’s important to keep a close eye on diabetic patients. We should use other tests and markers to find ACS in them.
Elderly patients often have atypical ACS symptoms, making diagnosis tough. They might have cognitive issues, many health problems, and take many medicines. This can make it hard to spot ACS symptoms.
In older patients, symptoms like confusion, dizziness, or weakness are common. A detailed check-up is needed to find ACS in this group.
Knowing about these atypical symptoms helps us diagnose and treat better. Awareness and education are vital to tackle these challenges.
It’s key to know medical abbreviations well, like in ACS cases. Healthcare pros need to grasp the terms fast and right for ACS diagnosis and care.
The term for chest pain is ‘CP.’ It’s a big sign for patients to see a doctor. Knowing this helps doctors spot and treat ACS quickly.
Key aspects of chest pain include:
ACS diagnosis uses many medical terms. Knowing these is key for right diagnosis and treatment.
Some key terms include:
In emergencies, clear talk among healthcare pros is vital. Misunderstanding medical terms can cause delays or mistakes in treatment.
Benefits of clear communication include:
Using standard medical terms helps ensure patients get top care in emergencies.
Knowing the top risk factors for ACS heart is key to better heart health. By understanding these risks, we can prevent and treat heart disease early.
Hypertension, or high blood pressure, is a big risk for ACS. It damages blood vessels, making them more likely to block. We can manage high blood pressure with lifestyle changes and medicine.
High cholesterol or triglycerides in the blood is called hyperlipidemia. It can cause plaque in arteries, raising ACS risk. We can control it with diet, exercise, and sometimes medicine.
Smoking harms blood vessels, making them more likely to block. Quitting smoking greatly lowers heart disease risk.
Diabetes mellitus means high blood sugar. It damages blood vessels and nerves, raising ACS risk. Managing diabetes with lifestyle and medicine is key.
Other important risk factors include family heart disease history, obesity, not being active, older age, and unhealthy diet. Knowing these risks helps us prevent ACS better.
| Risk Factor | Description | Management Strategies |
| Hypertension | High blood pressure damaging blood vessels | Lifestyle changes, medication |
| Hyperlipidemia | High cholesterol or triglycerides | Diet, exercise, medication |
| Smoking | Damages inner lining of blood vessels | Quitting smoking |
| Diabetes Mellitus | High blood sugar damaging blood vessels and nerves | Lifestyle changes, medication |
Table: Major Risk Factors for ACS and Their Management
By managing these risk factors, we can lower ACS risk. It’s important to work with doctors to create a plan for reducing risk.
The American Heart Association (AHA) has set clear guidelines for Acute Coronary Syndrome (ACS). They stress the need for quick diagnosis and treatment. These rules help doctors give the best care to ACS patients.
The AHA’s ACS guidelines have changed a lot over time. They use the newest research and findings to help patients. This shows their dedication to better ACS management.
The guidelines highlight the need for fast diagnosis. They recommend using ECG monitoring and cardiac biomarker testing. These tools are key for accurately diagnosing ACS patients.
| Diagnostic Tool | Purpose |
| ECG Monitoring | To quickly identify signs of ischemia or infarction |
| Cardiac Biomarker Testing | To assess for cardiac damage |
Treatment plans include pharmacological interventions and percutaneous coronary intervention (PCI). The right treatment depends on the patient’s situation and how severe the ACS is.
Recent updates aim to make diagnosis and treatment quicker. These changes are designed to improve patient care by making treatments more timely and effective.
Diagnosing acute coronary syndrome (ACS) needs a detailed approach. This includes clinical checks, ECG monitoring, and cardiac biomarkers. This method helps doctors accurately diagnose and treat ACS, leading to better patient care.
When we first see a patient suspected of ACS, we start by looking at their medical history and symptoms. We also check for risk factors for heart disease. This helps us decide who needs urgent care.
A detailed physical exam is also key. It can show signs of heart problems or other issues that might look like ACS. Based on this, we decide what tests to do next.
ECG monitoring is a big part of diagnosing ACS. We look for specific changes in the ECG, like ST-segment elevation or depression. These changes help us understand the type and severity of ACS.
In the acute setting, continuous ECG monitoring is vital. It lets us catch changes in the heart’s rhythm quickly and respond fast.
Cardiac biomarkers, like troponin, are key in diagnosing ACS. High troponin levels mean heart damage, and how high it is shows how bad the damage is.
We also look at other biomarkers, like CK-MB and myoglobin. But troponin is preferred because it’s very sensitive and specific.
| Cardiac Biomarker | Sensitivity | Specificity |
| Troponin | High | High |
| CK-MB | Moderate | Moderate |
| Myoglobin | High | Low |
Advanced imaging like echocardiography, cardiac CT, or CMR imaging also helps in diagnosing and managing ACS. These tests let us see how well the heart is working and spot any complications.
These tests help us find out who might need more aggressive treatments, like revascularization.
Using ACLS protocols quickly is key for better results in ACS patients. ACLS guidelines help by giving a clear plan for treating ACS. This plan focuses on fast and right actions.
When ACS is thought of, quick actions are vital. These include:
Quick action can greatly help patients by cutting down time to get a diagnosis and treatment.
Medicine is very important in treating ACS. Guidelines suggest using:
As ACLS guidelines say, “medicines should be chosen and given based on the patient’s specific needs and how they react.”
Important choices in ACLS for ACS include:
These choices need a team effort and good communication among team members.
Good team work is key in managing ACS. This means:
“Clear talk, clear roles, and a united effort are vital for the best care.”
Everyone should know their part and work together well. This helps get the best results for ACS patients.
It’s key for doctors to know the many ways to treat ACS. This helps them make better choices and lets patients understand their treatment. ACS treatment uses different methods to manage the condition well.
Medicines are a big part of treating ACS. They include drugs to stop blood clots, prevent more clots, and lower heart work. They also help lower cholesterol. These drugs are very important in the early treatment of ACS and are often used for a long time to stop the condition from coming back.
PCI, like angioplasty and stenting, is a main treatment for ACS, mainly for STEMI. It opens the blocked artery to get blood flowing to the heart again.
CABG is a surgery that bypasses blocked arteries with grafts. It’s for patients with complex heart disease or those who can’t have PCI.
Rehab is a big part of managing ACS. It helps improve physical function, manage risks, and boost overall health. It includes a team of experts, exercise, lifestyle education, and mental support.
| Treatment Strategy | Description | Key Benefits |
| Pharmacological Interventions | Use of medications to manage ACS | Prevents clot formation, reduces myocardial oxygen demand |
| PCI | Angioplasty and stenting to open blocked arteries | Restores blood flow to the heart muscle |
| CABG | Surgical bypass of blocked coronary arteries | Improves blood flow for patients with complex disease |
| Rehabilitation | Multidisciplinary program for recovery | Improves physical function, manages risk factors |
Learning about acute coronary syndrome (ACS) is key to better patient care and outcomes. It’s important for both patients and healthcare providers to understand ACS well. This knowledge helps in managing the condition effectively.
Public awareness campaigns are vital. They teach people about ACS signs and symptoms. They stress the need for quick medical help. These campaigns use many media to reach lots of people, spreading awareness and prevention.
Training programs for healthcare providers are essential. They teach the latest in ACS management. Topics include diagnosis, treatment, and the need for quick action. This ensures providers use the best ACS care methods.
Patient education materials are very important. They help people understand their health and make smart care choices. These include brochures, websites, and videos. They cover everything from recognizing symptoms to post-treatment care.
Community resources and support groups offer ongoing help. They help patients and families deal with ACS challenges. These groups let people share experiences, get advice, and connect with others facing similar health issues.
Using these educational tools can greatly improve ACS management. It leads to better patient care and a more informed, supportive community.
Acute coronary syndrome (ACS) is a serious medical issue that needs quick action. Knowing the signs and symptoms of ACS is key to getting the right treatment fast. This guide has covered the top 10 signs and risk factors, like chest pain and high blood pressure.
Understanding how ACS works is vital for doctors to treat it well. The American Heart Association (AHA) has guidelines for diagnosing and treating ACS. These guidelines stress the need for fast action, including medicines and procedures like PCI.
Knowing the signs and risks of ACS can help people get medical help quickly. This can lower the chance of serious problems and improve treatment results. We stress the need for education and awareness in dealing with ACS, helping both doctors and patients.
Acute Coronary Syndrome (ACS) is a condition where blood flow to the heart suddenly drops. It often causes chest pain or discomfort.
The main symptom of ACS is chest pain. People often describe it as a tight feeling in the chest. This pain can spread to the arms, jaw, or back. Other signs include shortness of breath, nausea, and vomiting.
ACS can show up differently in various groups. Women and the elderly might not have the typical symptoms. Diabetic patients might not even feel pain, known as silent ischemia.
The term for chest pain in medical terms is ‘CP’.
High blood pressure, high cholesterol, smoking, diabetes, and a family history of heart disease are major risks for ACS.
The American Heart Association (AHA) has guidelines for ACS. They cover how to diagnose and treat it. This includes using heart tests, ECGs, and treatments like stents.
Doctors use several methods to diagnose ACS. These include checking the patient’s symptoms, ECGs, heart enzyme tests, and imaging tests like echocardiograms and angiograms.
Advanced Cardiovascular Life Support (ACLS) is key in managing ACS. It involves quick actions, giving medicines, and making important decisions.
Treatments for ACS include medicines, stents, bypass surgery, and rehabilitation plans. These help manage symptoms and improve heart function.
Knowing about ACS is vital for both patients and doctors. It helps recognize symptoms, understand risks, and get timely care.
There are many resources for learning about ACS. These include public campaigns, training for doctors, patient guides, and support groups.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us