At Liv Hospital, we know how important accurate electrocardiogram analysis is. It helps spot serious heart problems. A 12-lead EKG looks at the heart from twelve angles. This gives a full picture of how well the heart is working.
Reading a 12-lead EKG needs a careful method. It helps find heart issues and guide good heart care. We focus on our patients and use the latest medical standards for every EKG.
Learning about EKGs helps doctors make better choices. They can help in urgent situations or regular check-ups. This leads to top-notch healthcare with full support.
Key Takeaways
- Accurate electrocardiogram analysis is key for finding heart problems.
- A careful way to read 12-lead EKGs is vital for reliable heart care.
- Liv Hospital is dedicated to patient care and using the latest EKG standards.
- Understanding EKGs helps doctors make smart choices in emergencies and regular visits.
- Thorough EKG analysis helps provide excellent healthcare.
Understanding the Basics of Electrocardiography
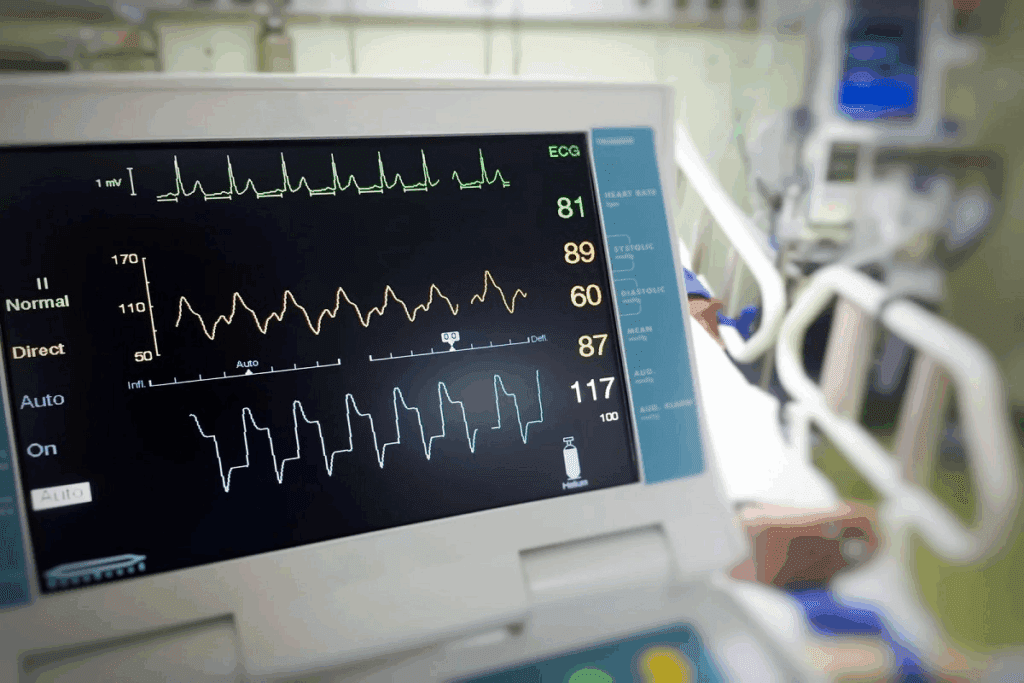
To understand a 12-lead EKG, you need to know the basics of electrocardiography. This tool records the heart’s electrical activity over time. It uses electrodes on the skin to do this. Learn how to read a 12 lead EKG, identify heart rhythm issues, and interpret results accurately.
What is an Electrocardiogram?
An electrocardiogram, or ECG or EKG, measures the heart’s electrical activity. It shows the heart’s rhythm and helps find heart problems.
ECG vs. EKG: Understanding the Terminology
ECG and EKG are often used the same way, but they come from different roots. ECG comes from “cardio” (heart) and “gram” (record) in Greek. EKG comes from the German “Elektrokardiogramm.” Both are the same test.
The Importance of Cardiac Electrical Activity Recording
Recording the heart’s electrical activity is key to understanding it. An electrocardiogram study helps spot arrhythmias and ischemia. It also checks the heart’s electrical health.
| Aspect | Description | Clinical Significance |
| Heart Rhythm | The pattern of electrical activity | Diagnosing arrhythmias |
| Electrical Conduction | The pathway of electrical impulses | Identifying conduction disorders |
| Ischemia Detection | Changes in ST segments and T waves | Diagnosing coronary artery disease |
Knowing these basics is key for doctors to read EKGs well. It helps them make better decisions for patients.
The Anatomy of a 12 Lead EKG
Knowing how a 12-lead EKG works is key to understanding it well. A standard 12-lead ECG system uses 10 electrodes. These electrodes capture the heart’s electrical activity from 12 angles, giving a full view of how the heart works.
The 12 Different Leads and Their Perspectives
The 12-lead EKG has 12 leads, each showing a different view of the heart’s electrical activity. The leads are split into limb leads and precordial leads. Limb leads (I, II, III, aVR, aVL, and aVF) show the heart’s activity from the front. Precordial leads (V1-V6) show it from the side.
Each lead gives a detailed look at the heart’s electrical activity. For example, leads II, III, and aVF are great for spotting heart damage in the lower part of the heart.
Standard Paper and Calibration
ECG recordings are made on special paper with a grid. The paper moves at 25 mm/s, and 1 mV is shown as a 10 mm vertical deflection. This setup helps measure the ECG’s waveforms accurately.
Normal ECG Waveform Components
A normal ECG has several important parts: the P wave, QRS complex, T wave, and sometimes a U wave. The QRS complex represents ventricular depolarization, or when the ventricles get an electrical charge. Knowing these parts is vital for reading a 12-lead EKG.
| Component | Description |
| P wave | Represents atrial depolarization |
| QRS complex | Represents ventricular depolarization |
| T wave | Represents ventricular repolarization |
| U wave | Represents late ventricular repolarization (sometimes present) |
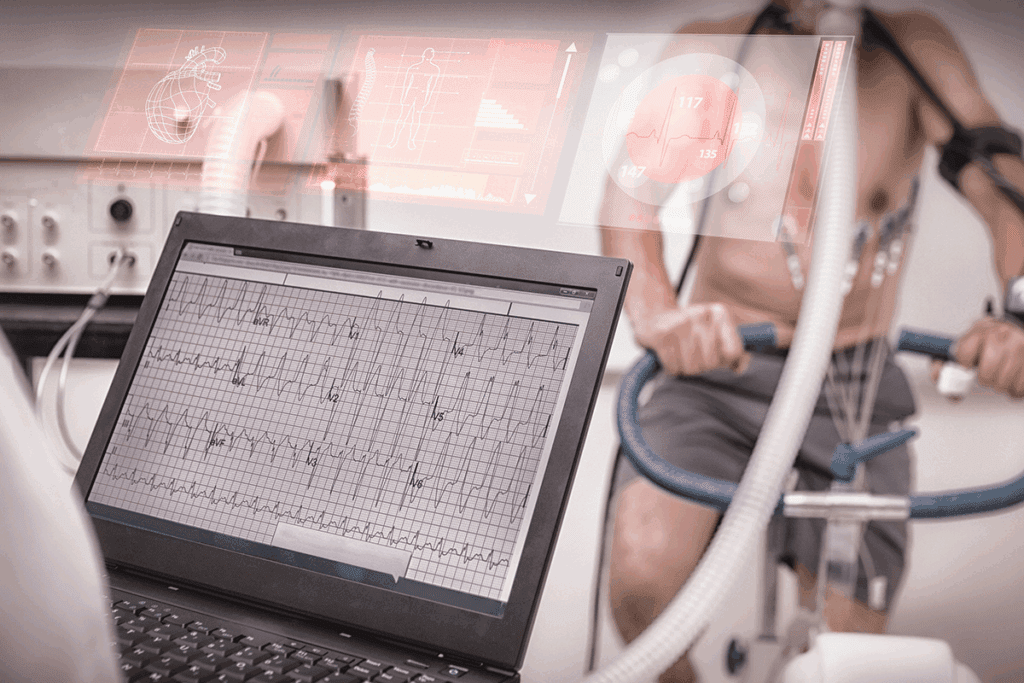
Essential Equipment and Proper Lead Placement
To get a good 12-lead EKG, you need the right tools and how you place the leads matters a lot. Getting the leads right is key for clear ECG readings.
Required Materials for ECG Recording
To do a 12-lead ECG, you’ll need certain things. Here’s what you need:
- ECG machine
- Electrodes (10 electrodes: 4 limb electrodes and 6 precordial electrodes)
- ECG paper or digital recording device
- Patient cable
- Conductive gel or paste (if required)
It’s important that all your gear works well. Also, check that the electrodes are fresh and right for the patient’s skin.
Correct Electrode Placement Technique
Before you start, make sure the skin is dry, hairless, and free of oils. Here’s how to get ready:
- Clean the skin with alcohol or soap and water
- Dry the skin completely
- Remove any hair or oils from the electrode sites
After getting the skin ready, place the electrodes as shown in the 12-lead ECG guide:
- Limb electrodes go on the wrists and ankles.
- Precordial electrodes go on the chest, following specific landmarks.
Common Placement Errors and Artifacts
Even with the right steps, mistakes can happen. Some common problems include:
- Putting electrodes in the wrong spot
- Bad skin prep causing issues
- Patient movement or muscle activity messing with the reading
To avoid these, make sure the patient is comfy and calm. Check the electrode placement often and keep the area quiet to cut down on problems.
By using the right equipment and placing electrodes correctly, we can make sure our 12-lead EKGs are precise and useful. This helps us analyze them better.
Systematic Approach to 12 Lead EKG Interpretation
To accurately diagnose heart conditions, healthcare professionals must use a systematic approach to 12-lead EKG interpretation. This methodical analysis is key to considering all important information. It helps avoid missing critical details.
The Importance of a Methodical Analysis
A systematic approach to EKG interpretation is vital. It minimizes the risk of missing clinically important information. By following a structured method, healthcare providers can ensure their analysis is thorough and reliable. This is critical in high-pressure situations where quick and accurate decisions are needed.
The benefits of a systematic approach include:
- Enhanced accuracy in diagnosis
- Reduced likelihood of overlooking critical EKG findings
- Improved consistency among healthcare providers
- Better patient outcomes due to timely and appropriate interventions
Overview of the 6-Step Interpretation Method
Our systematic approach to 12-lead EKG interpretation involves a 6-step method. This method covers key aspects of ECG analysis. Each step is designed to be followed in sequence for a thorough evaluation.
- Assessing heart rate
- Evaluating heart rhythm
- Analyzing the QRS complex
- Determining the electrical axis
- Measuring key intervals (PR, QT, QTc)
- Interpreting ST segments and T waves
This structured method provides a detailed framework for EKG interpretation. It ensures all critical components are evaluated.
Documentation and Reporting Standards
Accurate documentation and standardized reporting are essential in EKG interpretation. Clear and concise reports help in communication among healthcare providers. They support informed decision-making.
Key elements of effective documentation include:
- Clear description of EKG findings
- Interpretation of the clinical significance of these findings
- Recommendations for further evaluation or treatment as necessary
By following these standards, healthcare providers can ensure their EKG interpretations are communicated effectively. This supports high-quality patient care.
Step 1: Assessing Heart Rate
Understanding heart rate is key to knowing how well the heart works. It tells us if the heart is beating normally or not. This is important for diagnosing health issues.
Methods for Calculating Heart Rate
To figure out heart rate from an EKG, count R-R intervals in six seconds. Then, multiply by 10. This shows the heart rate in beats per minute (bpm).
For example, if there are 8 R-R intervals in six seconds, the heart rate is 80 bpm.
Normal vs. Abnormal Heart Rates
For adults, a normal heart rate is between 60 to 100 bpm. Rates under 60 bpm are called bradycardia. Rates over 100 bpm are called tachycardia.
Knowing if the heart rate is normal or not is very important. It helps doctors figure out what’s going on with the heart.
| Heart Rate Category | BPM Range | Clinical Significance |
| Bradycardia | < 60 bpm | May indicate good physical condition or a heart block |
| Normal | 60-100 bpm | Typical for a healthy adult at rest |
| Tachycardia | > 100 bpm | Could signify stress, anxiety, or cardiac issues |
Clinical Significance of Rate Abnormalities
Abnormal heart rates can mean a lot. Bradycardia might show a person is very fit or could point to heart problems. Tachycardia can be due to stress, fever, or anemia. But it can also mean serious heart issues like arrhythmias or cardiac ischemia.
It’s very important to correctly identify and understand abnormal heart rates. This helps doctors manage and treat patients properly.
Step 2: Evaluating Heart Rhythm
The second step in our systematic approach to 12-lead EKG interpretation is evaluating heart rhythm. This step is key. It helps us spot various cardiac arrhythmias and grasp the heart’s function.
Identifying Regular vs. Irregular Rhythms
First, we check if the heart rhythm is regular or irregular. A regular rhythm means the heartbeats are evenly spaced. An irregular rhythm shows changes in these intervals. Atrial fibrillation has an irregularly irregular rhythm, with no clear pattern.
Common Arrhythmias and Their Patterns
Many arrhythmias show unique patterns on an EKG. For example, atrial flutter looks like a “sawtooth” in the inferior leads. Ventricular tachycardia shows a wide QRS complex tachycardia. Knowing these patterns is key for correct diagnosis.
- Atrial fibrillation: Irregularly irregular rhythm
- Atrial flutter: Sawtooth pattern in inferior leads
- Ventricular tachycardia: Wide QRS complex tachycardia
Determining the Origin of Rhythm Disturbances
To find where rhythm disturbances start, we look at the EKG tracing. This tells us if the problem is in the atria, ventricles, or AV node. For instance, atrial fibrillation starts in the atria, while ventricular tachycardia starts in the ventricles.
By carefully checking the heart rhythm and knowing the signs of different arrhythmias, we can make accurate diagnoses. This helps guide the right treatment.
Step 3: Analyzing the QRS Complex
Looking at the QRS complex is key in reading a 12-lead EKG. It shows how the heart’s ventricles get ready to contract. This is important for pumping blood around the body.
Understanding Ventricular Depolarization
Ventricular depolarization is when the ventricles get ready to contract. This is seen on an EKG as the QRS complex. Knowing about ventricular depolarization helps us see if the heart is working right.
The QRS complex has three parts: the Q wave, the R wave, and the S wave. The Q wave goes down first, then the R wave goes up. After that, the S wave goes down again. These parts show how fast the ventricles depolarize.
Normal QRS Morphology and Duration
A normal QRS complex looks and lasts a certain way. It usually lasts between 0.08 and 0.10 seconds. If it lasts this long, it means the ventricles are depolarizing normally. The shape of the QRS can change a bit from lead to lead, but it should be pretty consistent.
When we check the QRS complex, we look for patterns and make sure it lasts the right amount of time. If it doesn’t, it could mean there’s a heart problem.
Identifying Abnormal QRS Patterns
Abnormal QRS patterns can mean different heart problems. For example, if the QRS lasts too long, it might mean a block or arrhythmia. Finding these problems is key to treating heart issues.
Some common abnormal QRS patterns include:
- Prolonged QRS duration (>0.10 seconds)
- Abnormal QRS morphology, such as notched or fragmented QRS complexes
- Presence of Q waves indicative of previous myocardial infarction
Spotting these patterns takes knowing what a normal QRS looks like and being able to spot when it’s different.
Step 4: Determining the Electrical Axis
Understanding the heart’s electrical axis is key for correct EKG readings. The electrical axis shows the heart’s electrical activity direction. It gives insights into how well the heart is working.
Finding the electrical axis is important because it can show heart problems. We use the hexaxial reference system to figure it out. This method looks at the QRS complex in different leads.
Methods for Calculating the Heart’s Electrical Axis
To find the electrical axis, we mainly use the hexaxial reference system. We look at the QRS complex in leads I, II, and III. We also check the augmented limb leads (aVR, aVL, aVF).
- Identify the QRS complex in leads I and aVF.
- Determine if the QRS is positive or negative in these leads.
- Use the hexaxial reference system to plot the QRS axis.
The hexaxial system helps us know if the axis is normal, left, or right. A normal axis is between -30° and +90°. Left axis deviation is -30° to -90°. Right axis deviation is beyond +90° or between +180° and -90°.
Normal Axis vs. Axis Deviation
A normal electrical axis means the heart’s electrical activity is directed downward and to the left. This is typical in a healthy heart. Axis deviation can mean there’s a heart problem.
Left axis deviation might show left ventricular hypertrophy or left anterior fascicular block. Right axis deviation could mean right ventricular hypertrophy or pulmonary embolism.
Clinical Significance of Axis Abnormalities
Axis deviation can mean a lot for a patient’s health. Left axis deviation might show structural heart disease or conduction problems. Right axis deviation could point to right ventricular issues or other right heart problems.
It’s important to understand what axis deviation means. This helps doctors make the right treatment plans. They need to look at EKG results, symptoms, and other tests for a full picture.
By knowing the electrical axis and its meaning, doctors can make better choices for patient care. This can lead to better health outcomes.
Step 5: Measuring Key Intervals (PR, QT, QTc)
Understanding the PR, QT, and QTc intervals is key for a full EKG analysis. These intervals give us important info about the heart’s electrical activity. They help spot different heart conditions when measured right.
PR Interval: Measurement and Interpretation
The PR interval starts with the P wave and ends with the QRS complex start. It shows how long it takes for the electrical signal to move from the atria to the ventricles.
- A normal PR interval is between 120 to 200 milliseconds.
- A long PR interval might mean first-degree atrioventricular (AV) block.
- A short PR interval is seen in Wolff-Parkinson-White syndrome.
QT and QTc Intervals: Calculation and Significance
The QT interval goes from the QRS complex start to the T wave end. It shows ventricular depolarization and repolarization. The QTc interval is the QT interval adjusted for heart rate.
- The QTc interval is key because a long QTc can lead to dangerous arrhythmias, like Torsades de Pointes.
- The normal QTc interval changes with gender and age. It’s usually under 440 milliseconds for men and 460 milliseconds for women.
Interval Abnormalities and Their Clinical Implications
Abnormalities in the PR, QT, and QTc intervals mean a lot clinically.
- Prolonged PR Interval: May show AV nodal disease or the effect of some meds.
- Short PR Interval: Linked to pre-excitation syndromes.
- Prolonged QTc Interval: Raises the risk of ventricular arrhythmias.
- Short QTc Interval: Though rare, it also raises arrhythmia risk.
In conclusion, accurately measuring and understanding the PR, QT, and QTc intervals is critical for diagnosing and managing heart conditions. These intervals offer valuable insights into the heart’s electrical activity. They help guide clinical decisions.
Step 6: Interpreting ST Segments and T Waves
The sixth step in our systematic approach involves a detailed examination of ST segments and T waves. These elements are key in diagnosing cardiac conditions.
Normal ST Segment and T Wave Morphology
Normal ST segments are usually flat or slightly up. They smoothly connect with the T wave. The T wave points in the same direction as the QRS complex, showing normal ventricular repolarization.
Normal ST Segment Characteristics: Isoelectric or slightly elevated, smooth transition to T wave.
Normal T Wave Characteristics: Generally upright in leads I, II, and V4-V6, following the QRS direction.
ST Elevation and Depression Patterns
ST elevation and depression are key signs of myocardial ischemia or infarction. ST elevation myocardial infarction (STEMI) is diagnosed by specific ST elevation criteria.
| Condition | ST Segment Change | Clinical Significance |
| STEMI | ST Elevation > 1 mm in 2 contiguous leads | Myocardial Infarction |
| Ischemia | ST Depression > 0.5 mm | Myocardial Ischemia |
T Wave Abnormalities and Their Significance
T wave abnormalities can signal various cardiac issues. These include ischemia, ventricular hypertrophy, and bundle branch blocks.
“T wave inversion can be a sign of myocardial ischemia, specially when paired with ST segment depression or other ECG abnormalities.”
T Wave Abnormality Examples:
- Inverted T waves in leads where they are normally upright.
- Peaked T waves, which can indicate hyperkalemia.
- Flattened T waves, which may suggest hypokalemia or ischemia.
Correctly interpreting ST segments and T waves is vital for diagnosing and managing cardiac conditions effectively.
Clinical Indications for Electrocardiogram Analysis
Electrocardiogram analysis is key in many medical situations. We use ECGs to check the heart’s function, find problems, and watch over patients with heart issues.
Chest Pain and Suspected Cardiac Ischemia
Chest pain is a big reason we use ECGs. Cardiac ischemia happens when the heart muscle doesn’t get enough oxygen. This is often due to blocked arteries. An ECG can spot signs of ischemia, like ST-segment changes, helping us decide what to do next.
Here are the main ECG signs of cardiac ischemia:
- ST-segment depression or elevation
- T-wave inversion or flattening
- Q waves showing past heart attacks
Palpitations and Syncope
ECG analysis is also vital for those with palpitations or syncope. Palpitations feel like an irregular heartbeat, and syncope is a sudden loss of consciousness. An ECG can find arrhythmias or heart problems that cause these symptoms.
Common ECG findings for palpitations or syncope include:
- Arrhythmias, such as atrial fibrillation or ventricular tachycardia
- Conduction problems, like AV block
- Pre-excitation syndromes, like Wolff-Parkinson-White syndrome
Pre-operative Assessment
Before surgery, we check the heart with ECGs to see if it’s safe. This is very important for big surgeries or for those with heart disease. The ECG helps find heart issues that could affect surgery results.
Important things to look for in pre-operative ECGs include:
- Significant arrhythmias or conduction problems
- Signs of past heart attacks or ischemia
- Overall heart function and risk factors
Monitoring of Cardiac Medications
ECG analysis is key for watching how cardiac medications work. Drugs like antiarrhythmics can change the heart’s electrical activity. An ECG checks if they’re working right and if there are side effects.
Important ECG monitoring points for cardiac medications include:
- QT interval prolongation, which can lead to dangerous heart rhythms
- Changes in heart rate or rhythm
- Signs of medication toxicity or bad effects
Conclusion: Mastering 12 Lead EKG Interpretation
Learning to read 12-lead EKGs takes practice and a clear plan. Healthcare workers can get better at spotting problems and making decisions by following a step-by-step guide.
Using a systematic way to read ECGs helps doctors find small issues and make smart choices for patients. It’s key to keep practicing and getting better at EKG reading to give the best care.
Reading 12 lead EKGs means looking at heart rate, rhythm, QRS complex, electrical axis, and ST segments. Getting good at these parts helps doctors diagnose and treat heart problems better.
We urge healthcare pros to keep working on their EKG skills. It’s a vital tool for top-notch patient care. With regular practice and a clear plan, anyone can master ECG reading, leading to better health outcomes.
FAQ
What does ECG stand for?
ECG stands for electrocardiogram. It’s a test that measures the heart’s electrical activity.
What is the difference between ECG and EKG?
ECG and EKG are the same test. ECG is used more in Europe, while EKG is common in the U.S.
What is a 12-lead EKG?
A 12-lead EKG records the heart’s electrical activity from 12 angles. It gives a full view of the heart’s function.
What is the QRS complex in an EKG?
The QRS complex shows when the heart’s ventricles contract. It’s a key part of the EKG.
How do you calculate heart rate from an EKG?
To find heart rate, count R waves in 6 seconds. Then, multiply by 10.
What is the normal heart rate range?
Normal heart rate is between 60-100 beats per minute (bpm).
What is the significance of ST segment elevation?
ST segment elevation can mean a heart attack or other heart issues. It needs quick medical help.
What are the clinical indications for electrocardiogram analysis?
ECG analysis is used for chest pain, palpitations, and syncope. It’s also for pre-operative checks and monitoring heart meds.
How is the electrical axis of the heart determined?
The heart’s electrical axis is found by looking at the QRS complex in leads I, II, and III.
What is the importance of proper electrode placement in EKG recording?
Correct electrode placement is key for a good EKG. Wrong placement can cause errors.
What is the abbreviation for electrocardiogram?
ECG is the abbreviation for electrocardiogram.
What does the PR interval represent?
The PR interval shows the time from atrial to ventricular depolarization.
What is the clinical significance of QT interval abnormalities?
QT interval issues can signal a risk of arrhythmias, like Torsades de Pointes.
References:
National Center for Biotechnology Information. (2025). How to Interpret a 12 Lead EKG StepbyStep. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK549803/









