Last Updated on November 6, 2025 by Bilal Hasdemir
At Liv Hospital, we know finding the right prostate cancer treatment can be tough. But androgen deprivation therapy has changed the game for many men. We focus on you, using the latest medical methods and care to meet your needs.Complete guide to ADT therapy for prostate cancer: how it works and outcomes.
Hormone therapy, or androgen deprivation therapy, is key for advanced prostate cancer. It cuts down on testosterone and other male hormones that help cancer grow. This way, we can slow cancer’s spread and help patients do better.
Prostate cancer is linked to androgens like testosterone. Studies show that Androgen Deprivation Therapy (ADT) helps patients live longer. ADT works by stopping testosterone from reaching cancer cells, making them die or grow slower.
This shows how important hormones are in prostate cancer growth.
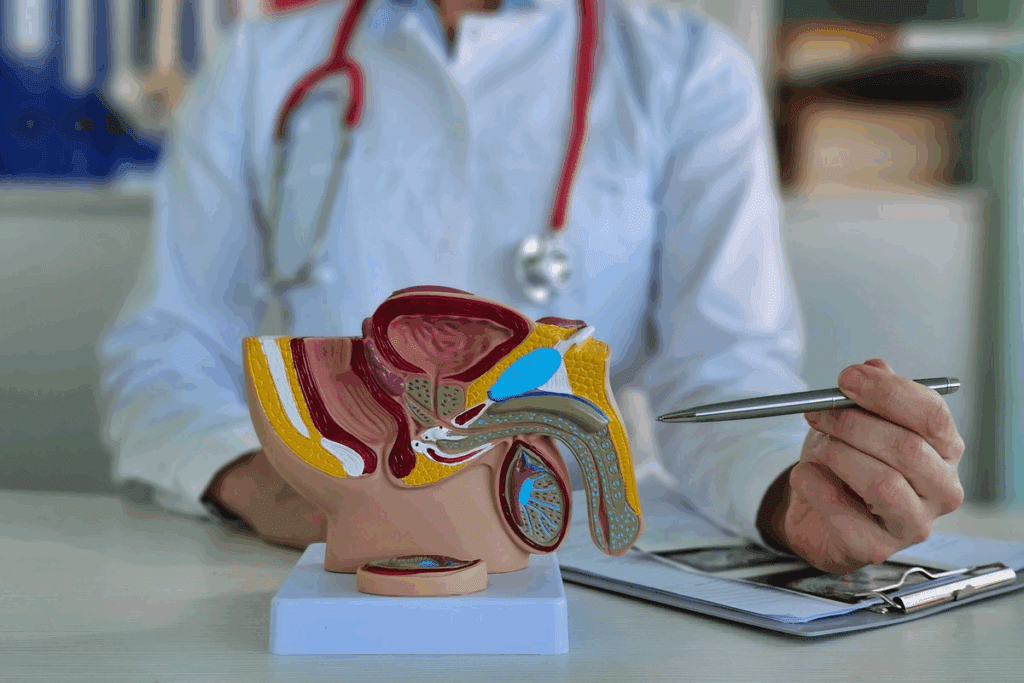
Male hormones, like testosterone, help prostate cancer cells grow. The androgen receptor on these cells makes them divide and multiply.
Testosterone’s role in prostate cancer growth is key. Knowing this helps doctors find better treatments.
Prostate cancer cells need androgens to grow and survive. This is why ADT is effective.
| Characteristics | Androgen-Dependent Cells | Androgen-Independent Cells |
| Growth Stimulation | Stimulated by androgens | Not dependent on androgens |
| Response to ADT | Responsive to ADT | Less responsive or resistant to ADT |
The table shows the difference between androgen-dependent and independent cells. It highlights the role of androgen dependency in treatment.
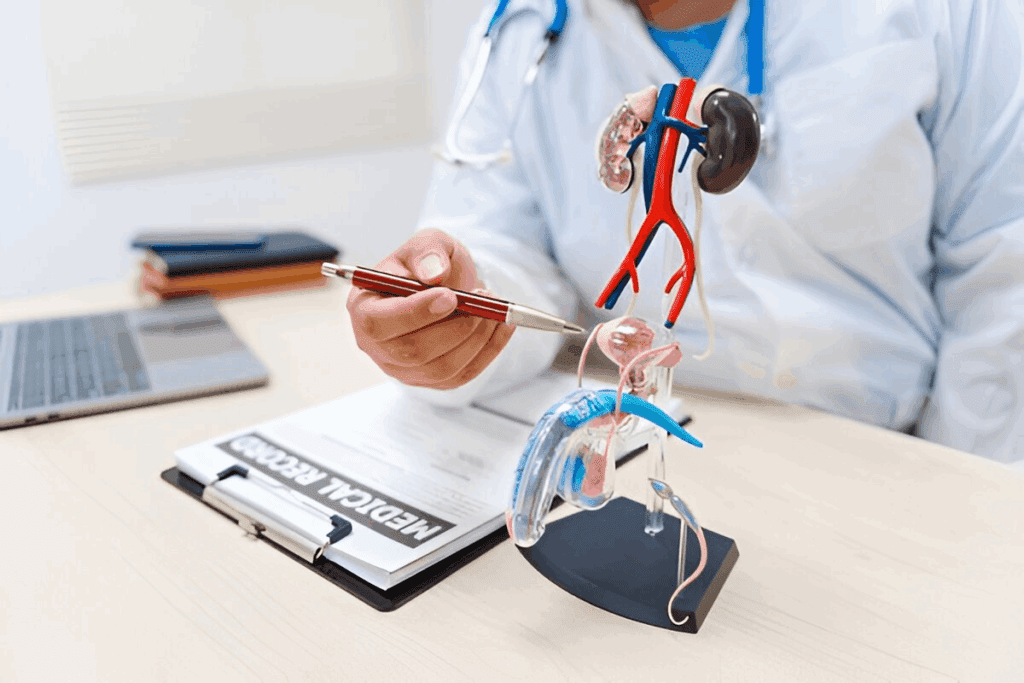
ADT therapy is key in treating prostate cancer. It lowers androgen levels, which slows cancer growth. Androgen deprivation therapy (ADT) works by reducing male hormones. These hormones help prostate cancer cells grow.
Androgen deprivation therapy is a treatment that deprives prostate cancer cells of the androgens they need to grow. Its main goal is to lower androgen levels. This stops androgens from acting on prostate cancer cells, slowing or stopping cancer growth.
This therapy helps manage the disease. It also improves quality of life and can increase survival rates for prostate cancer patients.
ADT works in several ways. It can reduce androgen production or block their action on prostate cancer cells. Medications like LHRH agonists (e.g., leuprolide, goserelin) and antagonists (e.g., degarelix) are used. Anti-androgens (e.g., bicalutamide, flutamide) are also used. These can be used alone or together for better results.
These therapies can greatly impact prostate cancer growth and spread. They offer a valuable treatment option for patients.
ADT therapy for prostate cancer uses different medications and surgeries to lower androgen levels. These treatments help control prostate cancer by cutting off the hormones cancer cells need to grow.
LHRH agonists first increase testosterone production. But, with ongoing use, they reduce LHRH receptors in the pituitary gland. This leads to lower testosterone levels. Examples are leuprolide, goserelin, and triptorelin. They are given via injections, usually monthly, every 3 months, or every 6 months.
LHRH antagonists, like degarelix, block LHRH on the pituitary gland. This immediately lowers luteinizing hormone and testosterone production. They don’t cause an initial testosterone surge, which can help prevent disease flare-ups.
Anti-androgens block androgens at the androgen receptor, stopping them from promoting prostate cancer cell growth. Examples are bicalutamide and flutamide. They are often used with LHRH agonists or antagonists for a stronger androgen block.
Orchiectomy, or removing the testes, is a way to lower testosterone levels. It’s a surgical option instead of medical treatments. Orchiectomy is considered for long-term ADT or for those who find injections hard to follow.
Studies show combining ADT with radiation therapy can greatly improve prostate cancer treatment outcomes. For example, one study found a 10-year survival rate increase. The choice of ADT medication or surgery depends on cancer stage, aggressiveness, patient preference, and health.
ADT therapy uses different methods and protocols for each patient. This makes sure each person gets the best treatment for their needs.
ADT therapy often involves injections, given monthly or every six months. The choice depends on the medication and how well the patient responds. For example, some LHRH agonists are given monthly, while others are given every three or six months.
Flexible injection schedules help doctors adjust treatment plans as needed. This is key in managing side effects and keeping patients on track with their treatment.
Keeping an eye on testosterone levels is a big part of ADT therapy. The goal is to keep levels below 20 ng/dL, which is considered castrate level. Blood tests are done regularly to check levels and adjust treatment if needed.
Effective monitoring lets doctors make quick changes to ADT therapy. This keeps testosterone levels in the right range, making treatment more effective.
Sticking to the treatment plan is key for ADT therapy success. Patients must follow their treatment closely and go to regular check-ups. These visits help doctors track how well the treatment is working, manage side effects, and make any needed changes.
By focusing on treatment adherence and regular check-ups, doctors can make ADT therapy work better. This improves patient outcomes.
Recent studies have shown ADT’s key role in treating prostate cancer. It helps slow down the disease and improves life quality. The evidence backing its effectiveness is strong.
Clinical studies have found ADT boosts survival rates in prostate cancer patients. A major study showed combining ADT with radiation therapy greatly increased survival rates. This combination is now a common treatment for many.
Another study found ADT’s role in lowering testosterone is key to slowing cancer growth. This improves patient results. The data shows ADT is vital in managing prostate cancer.
ADT helps slow prostate cancer progression, giving patients more time. This delay is key to a better quality of life. It means fewer symptoms and less discomfort for patients.
ADT also leads to better patient-reported outcomes, like symptom management and overall well-being. By reducing testosterone, ADT slows cancer cell growth. This delays severe symptoms.
“The use of ADT in prostate cancer treatment has revolutionized the management of this disease, improving survival rates and quality of life.”
Combining ADT with radiation therapy is changing how we treat prostate cancer. This mix of treatments offers a more complete way to fight prostate cancer.
ADT and radiation therapy together create a synergistic effect. This makes cancer cells more vulnerable to radiation. This combo has been shown to greatly improve treatment results.
“The mix of ADT and radiation therapy is a big step forward in prostate cancer treatment,” says Medical Expert, a top oncologist. “Together, we can better control the cancer and boost survival rates.”
The timing of ADT with radiation therapy is key. There are three main ways: neoadjuvant, concurrent, and adjuvant. Neoadjuvant ADT is given before to shrink the tumor. Concurrent ADT is during to make radiation more effective. Adjuvant ADT is after to kill any leftover cancer cells.
The length of ADT with radiation therapy varies. It depends on the patient’s risk and the treatment plan. Research shows this combo can raise 10-year survival rates for prostate cancer patients.
Healthcare providers plan the timing and length of ADT and radiation therapy carefully. This helps get the most benefits while reducing side effects.
In recent years, we’ve seen big changes in treating prostate cancer. New therapies are being added to ADT, making treatments better. This shift is bringing new hope to patients.
Enzalutamide is a big step forward in ADT treatment. It blocks androgens, stopping prostate cancer cells from growing. Studies show it makes treatments more effective, helping patients live longer and fight cancer better.
Abiraterone and other CYP17 inhibitors are also making a difference. They stop the body from making androgens, which cancer cells need to grow. When used with ADT, they help patients with advanced prostate cancer live longer.
It’s important to look at how well these new treatments work together. Clinical trials show that adding enzalutamide or abiraterone to ADT improves results. But, the right choice depends on the patient’s health and the cancer’s specifics.
We’re entering a new era in prostate cancer treatment. Advanced combinations are giving patients new hope. As research keeps improving, we’ll see even better treatments and outcomes.
To get the most from ADT, finding the right treatment length is key. The time spent on Androgen Deprivation Therapy (ADT) for prostate cancer is very important. It greatly affects how well a patient does.
Knowing a patient’s risk level is vital for setting ADT’s length. Doctors sort patients into groups based on PSA levels, Gleason score, and stage. High-risk patients usually need longer ADT to control cancer well.
Tools help doctors decide how long ADT should last. For example, high-risk patients might need ADT for 2-3 years or more. But, those with lower-risk cancer might not need it as long.
Choosing between intermittent and continuous ADT is important. Intermittent ADT means taking breaks from treatment to lessen side effects and improve life quality. Continuous ADT keeps hormone levels low all the time.
Studies suggest intermittent ADT works for some, like those with less aggressive cancer. But, for high-risk or advanced cancer, continuous ADT is the usual choice. The right choice depends on the patient’s health and how they handle treatment side effects.
Adjusting ADT length based on how a patient responds is getting more attention. We watch PSA levels and other signs to see how treatment is working. Changing treatment length based on response can improve results and avoid too much treatment.
By looking at how a patient reacts and their risk, we can tailor ADT to fit their needs. This approach balances treatment benefits with side effects. It helps patients live better and feel better.
ADT is a key treatment for prostate cancer but comes with side effects. These can really affect how well a patient lives. It’s important to manage these side effects well.
Hot flashes are a big problem for up to 80% of patients. Hot flashes can be very bad and mess up daily life. Patients also often gain weight and lose muscle.
To deal with these changes, making lifestyle changes helps. Eating less and more protein can help with muscle loss. Also, exercising, like weight training, can help a lot.
ADT can make bones weaker, raising the risk of osteoporosis and fractures. It’s smart to get regular bone scans. To prevent bone loss, taking bisphosphonates or denosumab is helpful.
It’s also key to get enough calcium and vitamin D. Regular exercise and not smoking or drinking too much alcohol also helps bones.
| Preventive Measure | Description |
| Bisphosphonates | Medications that help strengthen bones by reducing bone resorption |
| Denosumab | A monoclonal antibody that targets the RANKL protein, involved in bone resorption |
| Calcium and Vitamin D Supplements | Essential nutrients for maintaining bone health |
ADT can increase the risk of heart disease and metabolic syndrome. It’s important to check blood work regularly. This includes looking at cholesterol, blood pressure, and sugar levels.
To lower heart risk, diet and exercise are key. Doctors might also prescribe medicine to control blood pressure and cholesterol. A study found that heart risks for men on ADT are high. So, managing these risks is very important.
Source: A relevant medical journal
ADT can also affect the mind, causing depression, anxiety, and memory loss. It’s vital to watch for these signs and act quickly.
Helping patients with counseling and memory training can be very helpful. Some might need medicine for depression or anxiety.
In summary, while ADT is a good treatment for prostate cancer, its side effects need careful handling. By understanding and tackling these issues, doctors can improve patients’ lives a lot.
Choosing the right patients for Androgen Deprivation Therapy (ADT) is key in treating prostate cancer well. ADT is mainly for those with high-risk localized or advanced prostate cancer. We look at several important factors when deciding.
ADT is considered for patients with high-risk localized or metastatic prostate cancer. The risk level depends on PSA level, Gleason score, and clinical stage. Those with high-risk features see big benefits from ADT, as it lowers cancer recurrence risk and boosts survival chances.
| Risk Category | PSA Level | Gleason Score | Clinical Stage |
| Low | <10 ng/mL | 6 or less | T1-T2a |
| Intermediate | 10-20 ng/mL | 7 | T2b-T2c |
| High | >20 ng/mL | 8 or higher | T3-T4 |
Age and health conditions are big factors in choosing ADT. Older patients or those with serious health issues need careful thought. We look at their overall health, life expectancy, and how ADT might affect their quality of life.
“The decision to start ADT should be based on a detailed look at the patient’s cancer, health, and personal wishes.”
ADT is good for many, but there are times when it’s not right. Patients with conditions like osteoporosis or heart disease might need other treatments. For those with lower-risk disease, we might suggest active surveillance or other local treatments.
In summary, picking patients for ADT is complex. We consider cancer stage, risk, age, health, and individual factors. This careful approach helps us use ADT effectively and improve outcomes for prostate cancer patients.
Androgen Deprivation Therapy (ADT) is key in treating prostate cancer. It uses hormone therapy to stop male hormones that help cancer grow. This therapy is very important in managing the disease.
ADT is getting better thanks to new research and treatments. Now, doctors use LHRH agonists and antagonists, anti-androgens, and combinations. These changes have made treatments better and improved patients’ lives.
As we move forward, we’ll see even more improvements in ADT. We might see treatments that last longer and new ways to mix therapies. By keeping up with these changes, doctors can give patients the best care possible. This will make treating prostate cancer even more effective.
ADT (Androgen Deprivation Therapy) is a treatment for prostate cancer. It lowers male hormones like testosterone that help cancer grow.
ADT blocks hormones that prostate cancer cells need. This slows or stops cancer cell growth.
There are several ADT medications. These include LHRH agonists, LHRH antagonists, anti-androgens, and surgical options like orchiectomy.
ADT therapy is given through injections. These are given monthly or every six months. It’s important to check testosterone levels to keep them low.
Combining ADT with radiation therapy kills more cancer cells. This improves treatment results. The timing and length of this treatment are key to success.
Side effects of ADT include hot flashes, weight gain, and muscle loss. It can also affect bone health, heart health, and mental health.
The best length of ADT treatment depends on several factors. These include the patient’s risk, response, and whether to use it continuously or intermittently.
ADT is usually recommended for certain cancer stages and risk levels. It considers the patient’s age, health, and other factors. It also looks at what treatments to avoid or use instead.
Androgen receptor pathway inhibitors, like enzalutamide, are used in advanced ADT treatments. They offer more options for treating prostate cancer.
ADT can affect quality of life due to its side effects. But, managing these side effects well and choosing the right patients can reduce its negative effects.
Intermittent ADT stops and starts treatment based on how the patient responds. Continuous therapy keeps treatment going without breaks. The choice depends on the patient’s situation.
Yes, ADT therapy is always evolving. New medications and combination treatments are being developed. These changes are improving prostate cancer care.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us