Last Updated on October 31, 2025 by Batuhan Temel
Learn angina definition, symptoms, and key facts about angina pectoris.
At Liv Hospital, we take heart health seriously. Stable angina is a condition where chest pain happens because of less blood to the heart. This usually comes from blocked arteries.
This chest pain can last up to five minutes. It often happens when you’re active or stressed. Knowing about angina pectoris is key to getting the right care.
We’ll cover the main points about stable angina. This includes its symptoms and important facts. We aim to help you understand your heart better.
Angina pectoris, or angina, is a condition that causes chest pain or discomfort. It happens when the heart doesn’t get enough oxygen-rich blood. This usually occurs during physical activity or stress.
There are different types of angina, with stable angina being the most common. Stable angina happens when you exert yourself or feel stressed. Other types include:
Chest pain from angina is mainly due to a temporary drop in blood flow to the heart. This drop can be caused by:
Knowing the causes of angina is key to managing and treating it. By understanding the triggers and types, people can control their condition better. This improves their quality of life.
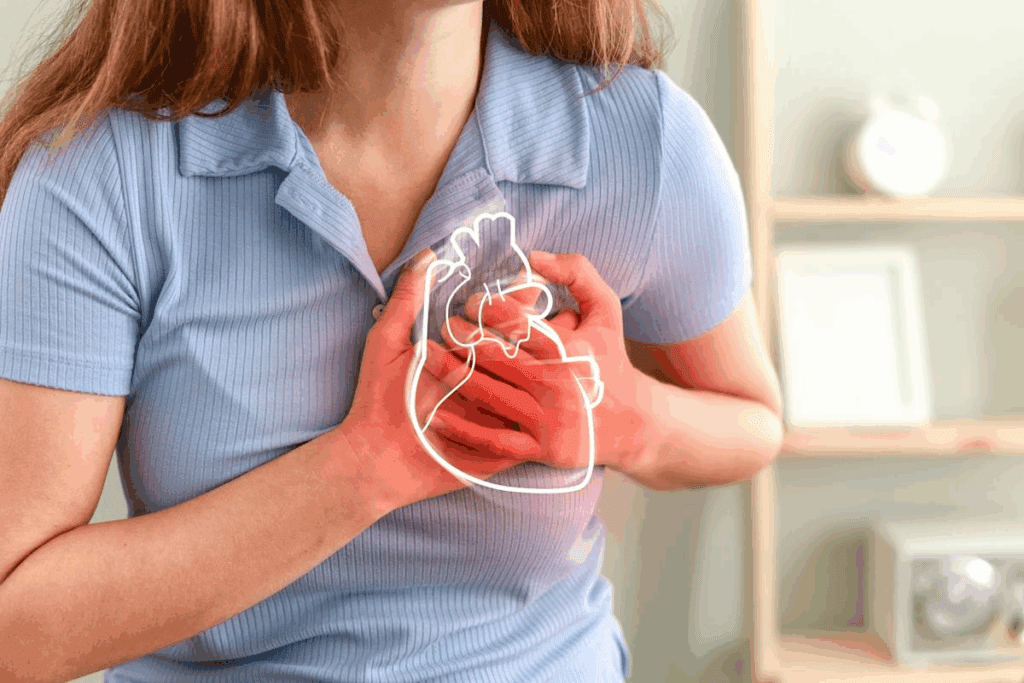
To understand angina, we need to look at its medical definition and how it’s diagnosed. Angina, or angina pectoris, is chest pain or discomfort. It happens when the heart muscle doesn’t get enough oxygen-rich blood, often because of blocked arteries.
Angina is chest pain or discomfort when the heart muscle doesn’t get enough oxygen. This pain feels like squeezing or pressure in the chest. It can also spread to the arms, back, neck, jaw, or stomach.
This pain usually happens when you’re active or stressed. It goes away when you rest or take medicine.
The clinical definition links angina to heart muscle not getting enough oxygen. This is usually because of blocked arteries. The pain is often predictable but can change in how bad it is and how often it happens.
The term “angina pectoris” was first used by William Heberden in 1768. He described chest pain that happens when you exert yourself. Back then, doctors diagnosed angina based on symptoms and what the patient said.
Now, we know more about angina thanks to new medical tools and tests. Doctors use ECGs, stress tests, and coronary angiography to check for artery blockages.
Looking at the history of diagnosing angina shows how far we’ve come. It shows the need for ongoing research and new ways to treat this condition.
Stable angina is a type of chest pain that happens when you exert yourself or feel stressed. It’s caused by blocked arteries in the heart. Knowing about stable angina helps us understand its unique traits and how it’s different from other chest pains.
Stable angina is known for its consistent chest pain. This pain usually shows up when you’re active or stressed. The main signs of stable angina are:
Doctors say stable angina is a sign of heart disease. It means the heart’s blood flow is temporarily cut off. This highlights the need to control heart disease risk factors.
Stable angina has a clear pattern, unlike unstable angina. People with stable angina can usually tell when pain will strike. For example, they might feel pain when climbing hills or during stressful times. This predictability helps them manage their condition better.
Knowing the pattern of stable angina is key to managing it. By identifying triggers and taking steps, people can lessen the pain’s frequency and intensity.
“The predictability of stable angina symptoms allows for better management and treatment planning.”
We stress the importance of sticking to treatment plans and making lifestyle changes. This helps manage stable angina well.
It’s key to know the signs of stable angina to manage it well. Stable angina causes chest pain or discomfort. This happens when the heart doesn’t get enough blood and oxygen, often during activity or stress.
The signs of stable angina include:
These symptoms usually happen when you’re active or stressed.
The time symptoms last can vary but often lasts 5 to 15 minutes. They’re often caused by:
Rest or taking medication like nitroglycerin can help ease these symptoms.
| Symptom | Characteristics | Triggers | Relief |
| Chest Pain/Discomfort | Pressure, squeezing, heaviness | Physical exertion, emotional stress | Rest, nitroglycerin |
| Shortness of Breath | Feeling winded | Physical exertion | Rest |
| Nausea/Exhaustion | Feeling tired, nauseous | Emotional stress, physical exertion | Rest |
Knowing these symptoms and what causes them helps manage the condition better. It also helps know when to see a doctor.
It’s key for doctors to tell stable angina apart from unstable angina and heart attacks. This helps patients know what they have and what treatment they need.
Stable angina causes chest pain when the heart needs more oxygen. This usually happens when you’re active or stressed. The pain goes away when you rest or take medicine.
Unstable angina is more serious. It causes chest pain without warning, even when you’re not active. This pain doesn’t go away with rest or medicine.
Unstable angina means a heart attack could happen soon. Here’s a table showing the main differences:
| Characteristics | Stable Angina | Unstable Angina |
| Pattern of Pain | Predictable, related to exertion | Unpredictable, may occur at rest |
| Duration of Pain | Typically short, relieved by rest or medication | May be prolonged, not relieved by rest or medication |
| Severity of Pain | Usually consistent | May increase in severity |
Angina is a sign of reduced blood flow to the heart. But a heart attack happens when blood flow is blocked long enough to damage heart muscle. Angina warns of a problem but isn’t a heart attack.
The main differences are:
Knowing these differences is vital for getting the right care quickly.
Knowing what causes stable angina is key to managing it well. Stable angina mainly comes from coronary artery disease. This disease narrows or blocks the coronary arteries because of plaque buildup.
Coronary artery disease (CAD) is the top reason for stable angina. CAD happens when the heart’s blood supply gets cut off. This is because the coronary arteries get narrowed or blocked by plaque.
Many lifestyle choices can raise the risk of stable angina. These include:
Some medical conditions also increase the risk of stable angina. These include:
| Medical Condition | Description | Impact on Stable Angina |
| Diabetes | High blood sugar damages blood vessels and nerves. | Raises the risk of CAD and angina. |
| High Blood Pressure | High blood pressure strains the heart and damages arteries. | Speeds up atherosclerosis and CAD. |
| High LDL Cholesterol | Too much “bad” cholesterol leads to plaque buildup. | Helps narrow and block coronary arteries. |
By knowing these causes and risk factors, people can take steps to manage their condition. This can help reduce how often they have angina episodes.
To find out if someone has stable angina, doctors use many steps. They look at the person’s health history and do physical checks. They also use special tests to see if it’s stable angina or something else.
First, doctors do a detailed check-up. They look for signs of heart problems. They check blood pressure and listen to the heart.
Tests are key to figuring out stable angina. Here are some:
Doctors also think about other possible causes of symptoms. They look at things like unstable angina or heart attacks. This helps make sure they get the right diagnosis.
By using what they find from the check-ups, tests, and ruling out other causes, doctors can accurately diagnose stable angina. Then, they can start treatment.
Stable angina needs a mix of treatments. This includes medicines, lifestyle changes, and sometimes surgery. We’ll cover the different ways to manage it.
There are several medicines for stable angina. These include:
These drugs help control symptoms and improve life quality.
Changing your lifestyle is key in managing stable angina. We suggest:
These lifestyle changes can greatly lessen angina episodes.
Sometimes, surgery is needed. This can include:
These surgeries help improve blood flow to the heart, reducing symptoms.
We can prevent and manage stable angina by understanding its causes and symptoms. We also need to take the right steps to prevent it. This includes medical treatment, lifestyle changes, and regular check-ups.
Primary prevention is key to avoiding stable angina. It involves controlling blood pressure, managing diabetes, and lowering cholesterol. It also means keeping a healthy weight and not smoking.
Key Primary Prevention Strategies:
| Prevention Strategy | Benefits |
| Hypertension Management | Reduces heart strain, lowers heart attack risk |
| Diabetes Control | Prevents heart problems, lowers heart disease risk |
| Cholesterol Reduction | Reduces plaque buildup, lowers heart attack risk |
Living with stable angina means constant management and lifestyle changes. Understanding the condition and its triggers helps manage symptoms. This improves life quality.
Tips for Managing Stable Angina:
Understanding stable angina is key to better management and a better life. We’ve looked into what it is, its symptoms, and important facts. It shows that with the right treatment and lifestyle changes, it’s a condition that can be managed.
Stable angina is a sign of coronary artery disease. It causes chest pain or discomfort, often when you’re active or stressed. Knowing the symptoms and causes helps people take action to manage their condition.
Managing stable angina means using medicine, making lifestyle changes, and sometimes surgery. A healthy lifestyle, following medication, and informed care choices help people with stable angina live fully.
We aim to give people the knowledge and tools to manage their condition well. This way, we can improve health and well-being for those with stable angina and angina pectoris.
Stable angina is chest pain or discomfort caused by less blood flow to the heart. It usually happens because of blocked arteries.
Symptoms include chest pain or discomfort. They often start with physical activity or stress. Rest or medicine can help relieve it.
Stable angina has a pattern and is usually triggered by activity or stress. Unstable angina is unpredictable and can happen at rest.
The main cause is coronary artery disease. This disease reduces blood flow to the heart muscle.
Doctors use a physical exam and tests to diagnose stable angina. They also rule out other conditions.
Treatments include medicines and lifestyle changes. For severe cases, surgery might be needed.
Preventing it involves managing risk factors like high blood pressure and cholesterol. A healthy lifestyle is also key.
Yes, it can be managed by controlling risk factors and living a healthy lifestyle. Following treatment plans is also important.
Angina pectoris is chest pain from reduced blood flow. A heart attack is when blood flow is blocked, damaging the heart muscle.
Risk factors include smoking, being inactive, and eating poorly. Medical conditions like high blood pressure and diabetes also increase risk.
National Center for Biotechnology Information. (2025). What Is Stable Angina Definition Symptoms and Key. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559016/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us