Acute cystitis is a common bacterial infection of the urinary bladder. It affects millions of people worldwide. This condition is caused by inflammation of the bladder, often due to Escherichia coli (E. coli) bacteria. It can cause a lot of discomfort and affect your daily life.What is acute UTI with cystitis? Learn how an acute urinary tract infection leads to inflammation and irritation of the bladder lining.
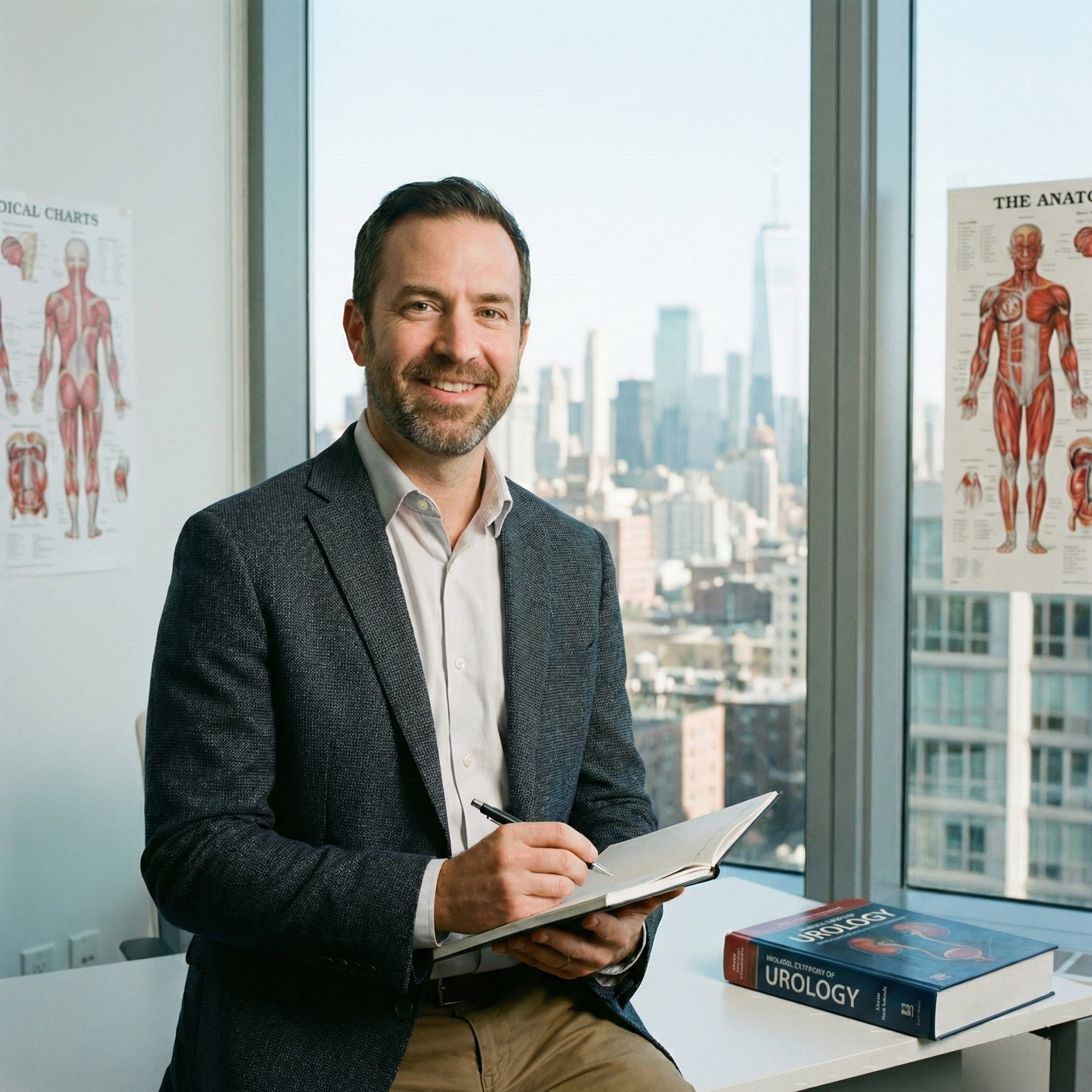
Bladder infection happens when bacteria get into the urinary tract. This leads to inflammation and uncomfortable symptoms. At Liv Hospital, we use the latest medical knowledge and care to treat urinary tract infections with top international standards.
Key Takeaways
- Acute cystitis is a bacterial infection of the urinary bladder.
- It is a common condition affecting millions worldwide.
- E. coli bacteria are a common cause of bladder infections.
- Symptoms can be uncomfortable and disrupt daily life.
- Liv Hospital provides complete care for urinary tract infections.
Understanding Acute Cystitis

Acute cystitis is a common condition that affects the bladder. It’s mainly caused by bacteria, with Escherichia coli being the top offender.
Definition and Basic Concepts
Acute cystitis is a sudden inflammation of the bladder, often due to infection. It can lead to pain while urinating and needing to go more often. Knowing what acute cystitis definition is key to treating it right.
The bladder’s job is to hold urine. But infections or inflammation can mess with this. We’ll dive into the reasons behind cystitis soon.
Prevalence and Global Impact
Acute cystitis is a big deal worldwide, hitting millions each year. Urinary Tract Infections (UTIs), which include cystitis, are among the top bacterial infections globally.
| Region | Estimated Annual Cases of UTIs | Percentage of Population Affected |
| North America | 150 million | 40% |
| Europe | 120 million | 35% |
| Asia | 200 million | 30% |
The global impact of UTI is huge, with big costs to healthcare and the economy. Knowing about acute cystitis is key to fighting it.
Looking into cystitis causes helps us tackle this global health problem better.
The Anatomy of the Urinary System
Knowing how the urinary system works is key to understanding cystitis. This system is responsible for making, storing, and getting rid of urine. It’s also known as the renal system.
The urinary system has several important parts. These include the kidneys, ureters, bladder, and urethra. We’ll look at each part, focusing on the bladder, to understand how it all works together.
Structure of the Bladder
The bladder is a muscular, hollow organ. It’s in the pelvis, behind the pubic bone. It connects to the kidneys through the ureters. Its shape changes to hold more or less urine.
The bladder has layers like the mucosa and muscularis. The mucosa touches urine. The muscularis layer, made of smooth muscle, helps push urine out when you pee.
How the Urinary System Functions
The main job of the urinary system is to get rid of waste and extra fluids. It starts in the kidneys, where filtration happens, making urine.
Urine then goes through the ureters to the bladder. There, it waits until it’s time to leave the body through the urethra. The muscles and nerves work together to control when you pee.
| Organ | Function |
| Kidneys | Filter waste and excess fluids from the blood to produce urine |
| Ureters | Transport urine from the kidneys to the bladder |
| Bladder | Stores urine until it is expelled from the body |
| Urethra | Provides the pathway for urine to exit the body |
In summary, the urinary system is designed to make, store, and get rid of urine. Knowing how the bladder and other parts work is key to understanding cystitis and its effects on the body.
Causes of Acute UTI with Cystitis
It’s important to know why acute UTI with cystitis happens. This condition is often caused by a bacterial infection. It leads to inflammation in the bladder.
Bacterial Pathogens
Bacteria are the main cause of acute UTIs with cystitis. E. coli is the biggest offender, causing 80-90% of UTIs. Other bacteria like Klebsiella, Proteus, and Staphylococcus saprophyticus can also lead to infections.
| Bacterial Pathogen | Prevalence in UTIs (%) | Characteristics |
| E. coli | 80-90 | Most common cause of uncomplicated UTIs |
| Klebsiella | 4-6 | Often associated with complicated UTIs |
| Proteus | 2-4 | More common in patients with urinary tract abnormalities |
| Staphylococcus saprophyticus | 2-4 | Common in young, sexually active women |
Risk Factors for Infection
There are several factors that increase the risk of getting a UTI with cystitis. These include:
- Female anatomy: Women are more prone to UTIs due to their shorter urethra.
- Sexual activity: Intercourse can introduce bacteria into the urinary tract.
- Certain contraceptive methods: Use of diaphragms or spermicides can increase UTI risk.
- Urinary tract abnormalities: Conditions like vesicoureteral reflux can predispose to UTIs.
Knowing about these risk factors and the role of bacteria is key. It helps in preventing and managing acute UTI with cystitis. By tackling these issues, we can lower UTI rates and better care for patients.
Gender Differences in Cystitis Occurrence
Women are more likely to get urinary tract infections than men. This is because of differences in their bodies.
Why Women Are More Susceptible
Women’s shorter urethras make it easier for bacteria to reach the bladder. Anatomical factors are a big reason for this. Hormonal changes during menstruation and menopause also play a part.
A study found that women are more likely to get UTIs. This is because of things like sex and birth control.
“The shorter urethra in women significantly increases the risk of bacterial entry into the bladder, leading to cystitis.”
Cystitis in Men
Men can get cystitis too, though it’s less common. It often happens in men with big prostates or other urinary issues. These problems can block urine flow, raising the risk of infection.
Men with cystitis usually have worse symptoms. They might also face serious problems like prostatitis or epididymitis. This shows why they need quick medical help.
It’s important to understand these differences. This way, doctors can give better care for cystitis in both men and women.
The Pathophysiology of Bladder Infections
Bladder infections happen when bacteria invade and the body’s immune system reacts. Knowing how this works helps us understand cystitis and how to treat it.
How Bacteria Invade the Bladder
Bacteria can get into the bladder through the urethra. Escherichia coli (E. coli), from the gut, is the main culprit. They stick to the bladder lining and start an infection.
Several things can make it easier for bacteria to get in:
- Sexual activity can spread bacteria to the urethra.
- Urinary tract problems like blockages let bacteria stay longer.
- Catheter use can bring bacteria straight into the urinary system.
Inflammatory Response in Cystitis
When bacteria get into the bladder, they set off an immune reaction. This reaction causes symptoms like dysuria (painful urination), frequency, and urgency.
The immune response includes:
- Immune cells go to fight the infection.
- Pro-inflammatory substances make symptoms worse.
- Local immune actions try to get rid of the infection.
Understanding how bladder infections work is key to finding good treatments. We need to target the bacteria and the immune response.
Common Symptoms of Acute Cystitis
Knowing the symptoms of acute cystitis is key for quick diagnosis and treatment. This condition, an inflammation of the bladder, often caused by infection, shows various symptoms. These can range from mild to severe.
Urinary Symptoms
The most common symptoms of acute cystitis are related to urination. These include:
- Dysuria: Painful or burning sensation while urinating, which can range from mild to severe.
- Frequency: Frequent need to urinate, even when the bladder is not full.
- Urgency: Sudden, intense need to urinate.
- Hematuria: Presence of blood in the urine, which can be visible to the naked eye or detected through laboratory tests.
Systemic Symptoms
Some people may also have systemic symptoms, including:
- Fever: Elevated body temperature, often indicating an infectious process.
- Malaise: General feeling of being unwell or tired.
- Pelvic discomfort: Pain or discomfort in the pelvic region.
When Symptoms Indicate Complications
While many cases of acute cystitis are uncomplicated, certain symptoms may indicate a more serious condition or complication, such as a kidney infection (pyelonephritis). These include:
- Severe flank pain: Pain in the side or back, below the ribs.
- High fever: Fever above 101.5°F (38.6°C).
- Nausea and vomiting: Symptoms that can lead to dehydration.
- Blood in the urine: Visible hematuria, which can be a sign of a more severe infection.
If you experience any of these severe symptoms, it is essential to seek medical attention promptly. This is to prevent complications and ensure appropriate treatment.
Diagnosing Acute Bladder Infections
To find out if you have an acute bladder infection, doctors use several steps. They start with a detailed check-up, then do lab tests, and sometimes use imaging. This way, they can tell if you have an infection and how bad it is.
Clinical Evaluation
The first step is a detailed check-up. Doctors look at your medical history and do a physical exam. They check for symptoms like pain when you pee, needing to pee a lot, and feeling pain in your belly.
Key parts of the check-up are:
- Looking at your medical history for risk factors and symptoms
- Doing a physical exam to check for belly pain
- Checking how long you’ve had your symptoms
Laboratory Tests
Lab tests are key to confirming an acute bladder infection. The main test is urinalysis, which includes:
- A urine dipstick test to find leukocyte esterase and nitrites
- A microscopic look at urine to see white blood cells and bacteria
- A urine culture to find the cause and what antibiotic to use
Urine culture is the best way to confirm a UTI. It shows for sure if you have an infection and what antibiotic to take.
| Laboratory Test | Purpose | Significance in Diagnosing Acute Cystitis |
| Urine Dipstick Test | Detects leukocyte esterase and nitrites | Shows bacteria and inflammation |
| Microscopic Examination | Sees white blood cells and bacteria | Confirms infection |
| Urine Culture | Finds the cause and antibiotic sensitivity | Helps choose the right antibiotic |
Imaging Studies
Imaging is not usually needed for simple bladder infections. But, if you have recurring infections or other issues, imaging might be needed. Common tests include:
- Ultrasound to check for blockages or abscesses
- Computed Tomography (CT) scan for upper urinary tract problems
As noted by
“Imaging studies should be reserved for patients with complicated or recurrent UTIs, as they provide valuable information on the urinary tract anatomy and possible complications.”
In summary, finding out if you have a bladder infection involves a detailed check-up, lab tests, and sometimes imaging. This method helps doctors make an accurate diagnosis and treat you right to ease your symptoms and prevent future problems.
Treatment Approaches for Acute Cystitis
Dealing with acute cystitis needs a mix of treatments. The main goal is to get rid of the infection. We’ll cover the key steps to make sure patients get the best care.
Antibiotic Therapy
Antibiotics are key in treating acute bacterial cystitis. The right antibiotic depends on several things. These include the likely cause of the infection, local resistance, and the patient’s health.
Here are some common antibiotics for acute cystitis:
- Nitrofurantoin
- Fosfomycin
- Trimethoprim/sulfamethoxazole
- Ciprofloxacin
| Antibiotic | Typical Dosage | Duration |
| Nitrofurantoin | 100 mg twice daily | 5-7 days |
| Fosfomycin | 3 g single dose | 1 day |
| Trimethoprim/sulfamethoxazole | 160/800 mg twice daily | 3 days |
Pain Management
Managing pain is important in treating acute cystitis. It affects how well a patient can live. We suggest using over-the-counter pain relievers like ibuprofen or acetaminophen.
In some cases, phenazopyridine may be given to ease urinary pain and burning. But remember, it doesn’t cure the infection.
Hydration and Supportive Care
Drinking enough water is key in treating acute cystitis. It helps flush out bacteria and aids in healing.
We tell patients to drink 8-10 glasses of water a day. Also, avoiding caffeine, alcohol, and spicy foods can help with discomfort while recovering.
Recurrent and Chronic Cystitis
Understanding recurrent and chronic cystitis is key to managing it. Recurrent cystitis means having repeated urinary tract infections (UTIs). These can really affect a person’s life.
Defining Recurrent Infections
Recurrent cystitis happens when you get UTIs often. This is more than twice in six months or three times in a year. It’s important to know the difference between relapse and reinfection to treat it right.
A relapse is when the same bacteria cause another infection soon after. This might mean the treatment didn’t work well or there’s another issue. Reinfection is when a new bacteria causes the infection. This is more about how likely you are to get it again.
Risk Factors for Recurrence
Many things can make cystitis come back. These include physical issues, how you behave, and health problems. Physical problems like vesicoureteral reflux or blockages in the urinary tract can make you more likely to get infections.
How you live your life can also play a part. This includes how often you have sex, what birth control you use, and how clean you stay. Health issues like diabetes, being immunosuppressed, and using catheters can also raise your risk.
Management Strategies
Managing recurrent cystitis means taking steps to prevent it and sometimes using antibiotics. Changing your lifestyle is very important. This includes drinking enough water, staying clean, and avoiding things that might irritate your bladder.
For some, using antibiotics as a preventive measure is suggested. This might be after sex or during times when you’re more at risk. Other strategies include using cranberry products, D-mannose, and probiotics. But, the proof for these is not always strong.
“The key to managing recurrent cystitis lies in understanding the individual’s specific risk factors and tailoring the management strategy according.”
By taking a full approach to managing recurrent and chronic cystitis, you can cut down on how often it happens. This can greatly improve your life.
Complications of Untreated Cystitis
Untreated cystitis can cause serious problems, not just in the bladder but throughout the urinary system. It’s key to know these risks to see why treatment is so important.
Ascending Infections
One big risk of untreated cystitis is ascending infections. Bacteria can move up from the bladder to the kidneys, causing pyelonephritis. This is a serious kidney infection.
Pyelonephritis brings symptoms like flank pain, fever, and nausea. If it gets worse, it can harm the kidneys or even cause sepsis, a deadly condition.
“Pyelonephritis is a serious infection that requires prompt medical attention. Untreated, it can lead to significant morbidity and potentially life-threatening complications.”
Chronic Bladder Changes
Recurring or ongoing cystitis can change the bladder for the worse. These changes can make urination symptoms and discomfort last a long time.
| Chronic Bladder Change | Description |
| Bladder Wall Thickening | The bladder wall gets thicker due to long-term inflammation, possibly shrinking its size. |
| Bladder Instability | The bladder muscle gets too active, causing frequent and urgent need to urinate. |
Systemic Complications
In rare but serious cases, untreated cystitis can cause systemic problems. Bacteria from the urinary tract can get into the blood, leading to sepsis. This is a condition that can be deadly if not treated quickly.
Knowing these possible complications shows why it’s vital to get medical help if cystitis symptoms don’t go away or get worse. Early treatment can stop these problems and help patients recover better.
Prevention Strategies
Preventing cystitis involves good hygiene, diet, and lifestyle changes. By following these steps, you can lower your risk of getting cystitis.
Hygiene Practices
Keeping clean is key to avoiding cystitis. Always wipe from front to back to stop bacteria from getting into your urethra. Keeping your genital area clean and dry also helps prevent bacteria growth.
Stay away from harsh soaps or douches, as they can irritate your urethra. Use gentle, fragrance-free products for better genital hygiene. This helps keep your natural balance and lowers cystitis risk.
Dietary Considerations
Your diet affects cystitis prevention. Drinking lots of water helps flush out bacteria from your urinary tract. Cranberry products may also help prevent bacteria from sticking to your bladder walls.
Try to avoid caffeine, alcohol, and spicy foods, as they can irritate your bladder. Eating foods high in antioxidants and fiber supports your urinary health.
| Dietary Element | Benefit |
| Adequate Hydration | Flushes out bacteria from the urinary tract |
| Cranberry Products | May prevent bacterial adhesion to bladder walls |
| Avoiding Irritants | Reduces bladder irritation and risk of cystitis |
Lifestyle Modifications
Making lifestyle changes can help prevent cystitis. Urinating after sex helps flush out bacteria. Also, avoid holding your urine for too long to prevent bacterial growth.
Wear breathable cotton underwear and choose loose-fitting clothes. These simple steps can greatly help in preventing cystitis.
Conclusion: Managing and Living with Acute Cystitis
Managing acute cystitis means knowing a lot about it. You need to understand its causes, symptoms, and how to treat it. This knowledge helps you make smart choices about your health.
To live well with cystitis, you must be proactive. Practice good hygiene, drink plenty of water, and know what increases your risk of infection. These actions help prevent more episodes and lessen the condition’s impact on your life.
There are many ways to treat cystitis, like antibiotics and pain relief. Working with your doctor, you can create a plan that fits your needs. This approach helps you get the best results.
Living with cystitis means you have to keep caring for yourself. Stay informed and take steps to manage your condition. This way, you can enjoy a better life and avoid serious problems related to UTIs.
FAQ
qWhat is acute cystitis?
Acute cystitis is a urinary tract infection (UTI) that affects the bladder. It causes inflammation and uncomfortable symptoms.
What causes acute cystitis?
Bacteria, like E. coli, usually cause acute cystitis. They invade the bladder and lead to infection.
Why are women more susceptible to cystitis?
Women are more likely to get cystitis because of their shorter urethra. This makes it easier for bacteria to reach the bladder. Hormonal and anatomical factors also play a role.
What are the symptoms of acute cystitis?
Symptoms include painful urination, frequent urination, and a strong need to urinate. Fever and abdominal pain can also occur.
How is acute cystitis diagnosed?
Doctors use a clinical evaluation and urine culture to diagnose it. Imaging studies may also be used to confirm the infection and check for complications.
What is the treatment for acute cystitis?
Treatment involves antibiotics to kill the infection. Pain management and staying hydrated also help alleviate symptoms.
Can cystitis lead to complications if left untreated?
Yes, untreated cystitis can cause kidney infections, chronic bladder changes, and other systemic complications.
How can I prevent cystitis?
To prevent cystitis, practice good hygiene, stay hydrated, and urinate after sex. Cranberry products may also help.
What is recurrent cystitis?
Recurrent cystitis means having repeated episodes of cystitis. It often stems from anatomical or behavioral factors.
How is recurrent cystitis managed?
Managing recurrent cystitis involves addressing risk factors, making lifestyle changes, and sometimes using preventive antibiotics.
Is cystitis in men less common?
Yes, men get cystitis less often. But when they do, it’s often linked to health issues like an enlarged prostate or urinary tract abnormalities.
Can acute cystitis become chronic?
Yes, if not treated or if risk factors are not managed, acute cystitis can become chronic. This leads to ongoing or recurring infections.
What is the role of antibiotic therapy in treating cystitis?
Antibiotics are the main treatment for acute cystitis. They aim to eliminate the bacterial infection causing the symptoms.
Are there any lifestyle changes that can help prevent UTIs?
Yes, staying hydrated, practicing good hygiene, and urinating after sex can help prevent UTIs.
References
National Center for Biotechnology Information. What Is Acute Cystitis and How Does It. https://www.ncbi.nlm.nih.gov/books/NBK482435/