Interstitial cystitis (IC), also known as bladder pain syndrome (BPS), is a chronic condition. It causes bladder and pelvic pain, along with urinary urgency and frequency. There’s a growing interest in how IC/BPS might link to bladder cancer.Understand the difference between chronic cystitis versus bladder neoplasm. Learn whether interstitial cystitis increases your risk of cancer.
Recent studies have looked at big groups of patients. They found a link between IC/BPS and a higher risk of bladder cancer. But, doctors are not all agreed on what this means.
We’re going to dive into the latest research. We’ll look at what we know about IC/BPS and bladder cancer. Knowing the truth about this link is key for the right diagnosis and treatment.
Key Takeaways
- Interstitial cystitis (IC) is associated with an increased risk of bladder cancer.
- The clinical significance and causation of this association are not yet clear.
- It’s important to evaluate patients thoroughly for accurate diagnosis.
- Using advanced tests is needed for good treatment plans.
- Understanding the link between IC/BPS and bladder cancer is important for patients.
Understanding Interstitial Cystitis and Bladder Pain Syndrome
It’s important to know about interstitial cystitis (IC) and bladder pain syndrome (BPS). These terms describe a long-term condition that causes bladder pain and pressure. They also lead to urgent need to urinate.
Definition and Diagnostic Criteria
Interstitial cystitis/bladder pain syndrome (IC/BPS) is a condition marked by chronic pelvic pain. It also includes bladder pressure or discomfort. Symptoms like frequent and urgent need to urinate are common. Doctors diagnose IC/BPS based on patient history and symptoms, as there’s no specific test.
The criteria for diagnosis are:
Chronic pelvic pain, pressure, or discomfort
Symptoms linked to the bladder
Urinary frequency and urgency
No other known causes for symptoms
Common Symptoms and Presentation
People with IC/BPS may have several symptoms. These include:
- Chronic pain in the bladder or pelvic area
Urinary urgency and frequency
Painful urination
Pressure or discomfort in the bladder area
These symptoms can be severe and affect daily life. They can also cause emotional distress and lower quality of life.
Prevalence and Gender Distribution
The number of people with BPS/IC varies, from 0.45% to 12.6%. Women are more likely to have IC/BPS than men. This gender difference is key in diagnosis and treatment.
Healthcare providers need to understand IC/BPS well. This helps them give better care. It also helps patients manage their condition better.
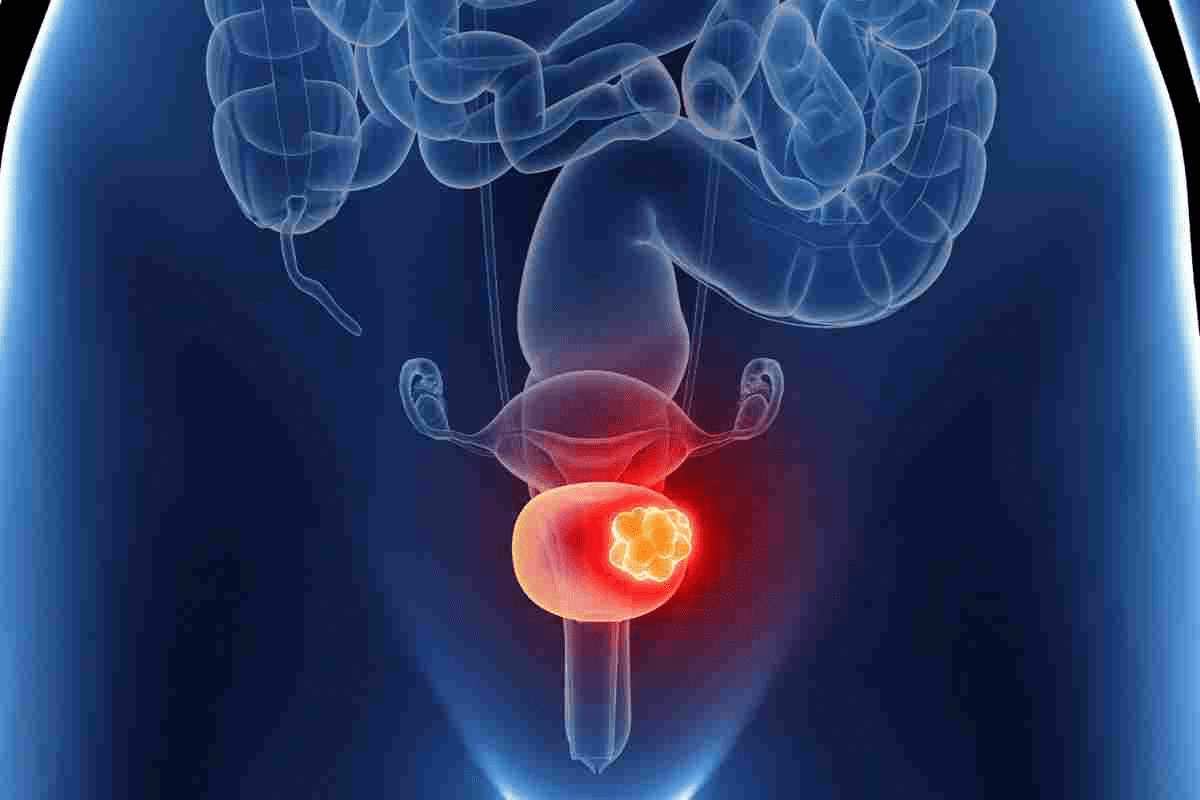
Bladder Cancer: Essential Facts and Risk Factors
To understand the link between interstitial cystitis and bladder cancer, we need to know the basics of bladder cancer.
Types and Staging of Bladder Cancer
Bladder cancer comes in three main types: urothelial carcinoma, squamous cell carcinoma, and adenocarcinoma. Urothelial carcinoma, or transitional cell carcinoma, makes up about 90% of cases. The staging of bladder cancer is key for treatment and prognosis.
It uses the TNM system to assess the tumor size, lymph node involvement, and metastasis. Knowing the stage is critical for choosing the right treatment. Stages range from 0, where cancer is in the bladder lining, to IV, where it has spread.
Established Risk Factors
Several factors increase the risk of bladder cancer. Smoking is the biggest risk, causing half of all cases. Chemical exposure in industries like dye and paint also raises the risk. Chronic bladder issues, parasitic infections, and genetics play a role too.
Smoking
Exposure to certain industrial chemicals
Chronic bladder irritation or infection
Genetic predisposition
Warning Signs and Early Detection
Spotting bladder cancer early is key to successful treatment. The main symptom is hematuria, or blood in the urine. Other signs include painful urination, frequent need to urinate, and urgency.
It’s important to notice these signs and see a doctor quickly. Tests like cystoscopy and urine cytology help find cancer early.
Chronic Cystitis Versus Bladder Neoplasm: Key Differences
It’s important for doctors to know the differences between chronic cystitis and bladder neoplasm. Both can have similar symptoms, making it hard to diagnose.
Symptom Comparison and Overlap
Chronic cystitis and bladder neoplasm both cause pelvic pain, frequent urination, and blood in the urine. But, the reasons and effects of these symptoms are different.
Let’s look at the symptoms and what they mean for each condition:
Symptom | Chronic Cystitis | Bladder Neoplasm |
Pelvic Pain | Common, often chronic | Less common, may be absent |
Urinary Frequency | Frequent, often with urgency | Variable, may be present |
Hematuria | Occasional, usually microscopic | Common, may be gross |
Diagnostic Challenges for Clinicians
Doctors find it hard to tell chronic cystitis apart from bladder neoplasm because of similar symptoms. They need to do a detailed check to find out what’s causing the symptoms.
Key diagnostic challenges include:
- Distinguishing between chronic and malignant conditions based on symptom presentation
- Interpreting diagnostic test results, such as cystoscopy and biopsy findings
- Considering the patient’s medical history and risk factors for bladder cancer
Differential Diagnosis Approaches
To solve these problems, doctors use different ways to diagnose. These include:
Comprehensive patient history: Getting all the details about the patient’s symptoms, medical history, and risk factors.
Diagnostic imaging: Using scans like ultrasound or CT to see the bladder and find any problems.
By using these methods, doctors can accurately diagnose and plan the best treatment.
The Scientific Evidence: Research on IC and Cancer Risk
Scientists have been studying the connection between IC and bladder cancer. Research from Taiwan has been key in this area. It has shed light on how IC/BPS might affect bladder cancer risk.
Taiwan Population-Based Cohort Studies
A big study in Taiwan looked at over 10,000 BPS/IC patients. It found that bladder cancer risk went up, mainly in the first year after diagnosis. This shows a possible link between IC/BPS and bladder cancer, but we don’t know why yet. The study’s large size and design make its findings reliable.
The study showed that the risk of bladder cancer was highest right after diagnosis. This makes us wonder if it’s really a higher risk or just a matter of finding more cases.
Propensity Score Matching Research Findings
Researchers used a method called propensity score matching (PSM) to control for other factors. PSM helps make the groups being compared more alike, making the study more valid. Even with this adjustment, the link between IC/BPS and bladder cancer stayed strong.
Using PSM made the evidence stronger. But we’re not yet clear on how IC/BPS and bladder cancer are connected.
Methodological Limitations and Research Gaps
Despite the valuable insights, there are some limitations to these studies. These include possible biases in who gets chosen for the study, differences in how IC/BPS is diagnosed, and the use of administrative data. We also don’t know the exact biological reasons behind this link.
“Further research is needed to clarify the relationship between IC/BPS and bladder cancer, including studies that explore the biological mechanisms underlying this association.”
It’s important to fill these gaps to fully understand the connection between IC/BPS and bladder cancer risk.
Inflammation and Cancer: Possible Biological Mechanisms
Inflammation is a complex response that can cause tissue damage. It may also lead to cancer, including bladder cancer. Chronic inflammation, with its long-lasting inflammatory cells and mediators, is seen in many conditions. This includes IC/BPS.
Chronic Inflammation as a Cancer Trigger
Chronic inflammation can start cancer through several ways. It produces harmful substances that damage DNA. If this damage isn’t fixed, it can cause genetic changes that lead to cancer.
It also boosts the release of substances that help cells grow and live longer. This creates a perfect environment for tumors to grow. The inflammation also weakens the body’s immune system, helping tumors spread.
Key factors in chronic inflammation that contribute to cancer development:
DNA damage due to ROS and RNS
Enhanced cell proliferation and survival
Suppression of anti-tumor immune responses
Angiogenesis and metastasis promotion
Cellular and Tissue Changes in Long-term IC
In long-term IC/BPS, the bladder changes a lot. The lining of the bladder, called the urothelium, gets damaged. The tissue underneath also changes, becoming more fibrous and vascular.
These changes create a long-lasting inflammation. This inflammation can lead to the release of substances that help cells grow. This can increase the risk of bladder cancer.
Comparing IC to Other Inflammatory Conditions Linked to Cancer
IC/BPS is similar to other inflammatory conditions that raise cancer risk. For example, chronic pancreatitis increases the risk of pancreatic cancer. Inflammatory bowel disease (IBD) raises the risk of colorectal cancer.
In all these conditions, long-lasting inflammation plays a big role. It creates an environment that can lead to cancer. Studying how chronic inflammation leads to cancer in these conditions can help us understand the link between IC/BPS and bladder cancer.
Common features of inflammatory conditions linked to cancer:
Persistent inflammatory response
Tissue damage and repair cycles
Release of pro-inflammatory cytokines and growth factors
Potential for DNA damage and genetic instability
Detection Bias in IC and Bladder Cancer Research
It’s key to grasp the role of detection bias in studies on interstitial cystitis (IC) and bladder cancer. Detection bias happens when how we diagnose a disease affects the numbers of cases. This can make us think there are more or fewer cases than there really are.
Understanding Detection and Surveillance Bias
Detection bias and surveillance bias are linked and can change what research shows. Surveillance bias means we find more cases because we’re watching more closely. For IC and bladder cancer, people with IC might get checked more often. This could mean we find more bladder cancer than before.
First-Year Diagnosis Patterns After IC Diagnosis
Studies show bladder cancer rates jump in the first year after IC diagnosis. This might be because we’re checking these patients more. This could mean we find cancers that were there but not showing symptoms.
A study found the highest risk of bladder cancer right after IC diagnosis. This suggests that how we find these cancers might skew our results.
Critical Evaluation of Current Research Findings
To really understand IC and bladder cancer, we need to look at research carefully. We must think about how we diagnose and how often we check. Also, we should look at when IC and bladder cancer are found.
By tackling detection bias, we can see the real connection between IC and bladder cancer. This helps us improve care for patients.
Blood in Urine: IC-Related Hematuria Versus Cancer Signs
Blood in the urine, or hematuria, can be a sign of both Interstitial Cystitis and bladder cancer. It’s important for patients and doctors to know the reasons for hematuria in IC patients. They need to tell the difference between harmless and serious bleeding.
Causes of Hematuria in IC Patients
Hematuria in IC patients can come from several sources. These include chronic bladder inflammation, Hunner’s ulcers, or other IC complications. Chronic inflammation is a key feature of IC, making the bladder tissue fragile and prone to bleeding.
Other reasons for hematuria in IC patients might include bladder stones, infections, or side effects from some medications. Finding the cause of hematuria is key to proper treatment.
Distinguishing Between Benign and Concerning Bleeding
Telling if hematuria is from IC or something more serious, like bladder cancer, can be hard. Important factors include other symptoms, how long the bleeding lasts, and any changes in urination habits.
IC patients should keep in close touch with their doctors. Regular check-ups and tests are vital for catching any problems early.
“The presence of hematuria in IC patients necessitates a thorough evaluation to rule out other causes, including malignancy.”
When to Seek Immediate Medical Attention
Even though hematuria can be harmless in IC patients, there are times when it’s urgent. Severe hematuria or bleeding with other serious symptoms like pain, trouble urinating, or fever needs quick attention.
Patients should get help right away if they see big changes in their symptoms or if they have hematuria for the first time. Quick action can stop complications and check for conditions like bladder cancer.
Diagnostic Procedures: Ruling Out Bladder Cancer in IC Patients
We use many tests to tell IC from bladder cancer. It’s hard to tell because their symptoms are similar. So, we need to check everything carefully.
Cystoscopy and Biopsy Considerations
Cystoscopy lets us see inside the bladder. A doctor can spot problems like ulcers or tumors. If they find something odd, they might take a biopsy to check for cancer.
Cystoscopy considerations include: how comfortable the patient is, if they use anesthesia, and how well they look around.
Urine Cytology and Biomarker Testing
Urine cytology checks for cancer cells in urine. It’s helpful but not perfect. Biomarker testing looks for special proteins or genes linked to bladder cancer.
Biomarkers can make diagnosis better when used with cystoscopy and cytology.
Imaging Studies and Their Interpretation
CT scans or MRI can spot tumors or other issues in the bladder. Radiologists look at these images for signs of cancer.
Diagnostic Procedure | Purpose | Key Considerations |
Cystoscopy | Visualize inside the bladder | Patient comfort, use of anesthesia |
Biopsy | Examine tissue for cancer cells | Accuracy of sampling, pathology analysis |
Urine Cytology | Detect cancer cells in urine | Sensitivity and specificity of the test |
Biomarker Testing | Identify specific proteins or genetic markers | Interpretation of results, correlation with other diagnostic findings |
Imaging Studies (CT, MRI) | Visualize tumors or abnormalities | Radiologist expertise, image resolution |
Monitoring Recommendations and Risk Management
Regular monitoring and risk management are key for those with Interstitial Cystitis (IC). It’s not just about treating symptoms. It’s also about keeping an eye on how the patient is doing.
Current Clinical Guidelines for IC Patients
Guidelines suggest regular checks for IC patients. This includes cystoscopy and urine tests to watch for complications or worsening of the disease. We stick to these guidelines to give our patients the best care.
Key monitoring recommendations include:
Regular cystoscopic examinations to assess bladder health
- Urine testing to detect any abnormalities or signs of infection
- Symptom tracking to monitor the effectiveness of treatment plans
Personalized Risk Assessment Approaches
Every patient is different, needing a personalized approach to risk assessment. We look at the severity of symptoms, medical history, and lifestyle when making a monitoring plan.
This way, we can spot problems early and act fast.
Communication Strategies with Healthcare Providers
Good communication with healthcare providers is vital for managing IC. We stress the need for open talks between patients and their healthcare team. This way, concerns get addressed quickly.
Strategies for effective communication include:
- Keeping a symptom journal to track changes and patterns
- Asking questions during appointments to clarify any concerns
- Sharing information about any new symptoms or changes in condition
By working together, we can create a care plan that meets each patient’s needs. This helps ensure the best health outcomes.
Conclusion: Balancing Concern with Current Evidence
Understanding the link between interstitial cystitis/bladder pain syndrome (IC/BPS) and bladder cancer is complex. Research shows a possible connection between IC/BPS and a higher risk of bladder cancer. Yet, the exact cause and how significant this risk is are not fully understood.
Our review of the latest studies emphasizes the need for more research. Chronic inflammation is a known cancer risk factor. But, its exact role in IC/BPS and bladder cancer needs more study.
In summary, people with IC/BPS should know about the possible risks. They should talk openly with their doctors. By grasping the current research and its boundaries, we can improve care and outcomes for patients.
FAQ
Can interstitial cystitis lead to bladder cancer?
We are studying if interstitial cystitis might lead to bladder cancer. Some studies hint at a link, but more research is needed. We want to understand this relationship better.
What are the common symptoms of interstitial cystitis?
Symptoms of interstitial cystitis include pelvic pain and frequent urination. You might also feel discomfort while urinating. These symptoms can affect your daily life.
How is bladder cancer diagnosed?
Doctors use imaging studies, cystoscopy, and biopsy to diagnose bladder cancer. They might also use urine cytology and biomarker testing.
Can chronic cystitis be mistaken for bladder cancer?
Yes, chronic cystitis and bladder cancer can have similar symptoms. Doctors must carefully look at symptoms, medical history, and test results. This helps them tell the two apart.
Does interstitial cystitis cause blood in the urine?
Interstitial cystitis can cause blood in the urine, but it’s not always a sign of bladder cancer. We’ll talk about why this happens and when to see a doctor.
How is the risk of bladder cancer assessed in IC patients?
Doctors use personalized risk assessments for IC patients. They look at medical history, symptoms, and test results to evaluate the risk.
What are the current clinical guidelines for IC patients regarding bladder cancer risk?
Guidelines suggest regular monitoring for IC patients to manage bladder cancer risk. We’ll discuss these guidelines and strategies for managing risk.
Can detection bias influence the reported link between IC and bladder cancer?
Yes, detection bias can affect the reported link between IC and bladder cancer. We’ll look into how detection and surveillance bias impact research.
What are the possible biological mechanisms linking IC to bladder cancer?
Chronic inflammation might link IC to bladder cancer. We’ll explore how long-term IC changes cells and tissues. We’ll also compare IC to other inflammatory conditions linked to cancer.
How can IC patients distinguish between benign and concerning bleeding?
IC patients should know the causes of bleeding and when to seek medical help. We’ll guide you on how to tell if bleeding is a concern.
Are there any specific diagnostic procedures used to rule out bladder cancer in IC patients?
Yes, tests like cystoscopy, biopsy, and urine cytology are used to rule out bladder cancer in IC patients. We’ll discuss these tests and how to interpret them.
References
- Kok, D. J. (2016). Timelines of the “free-particle” and “fixed-particle” models of renal stone formation. World Journal of Nephrology, 5(6), 213–219. https://pmc.ncbi.nlm.nih.gov/articles/PMC5250668/