Last Updated on October 31, 2025 by Saadet Demir

If you’re among the millions suffering from obstructive sleep apnea, you might find relief in sleep apnea surgery. It offers a variety of effective solutions.
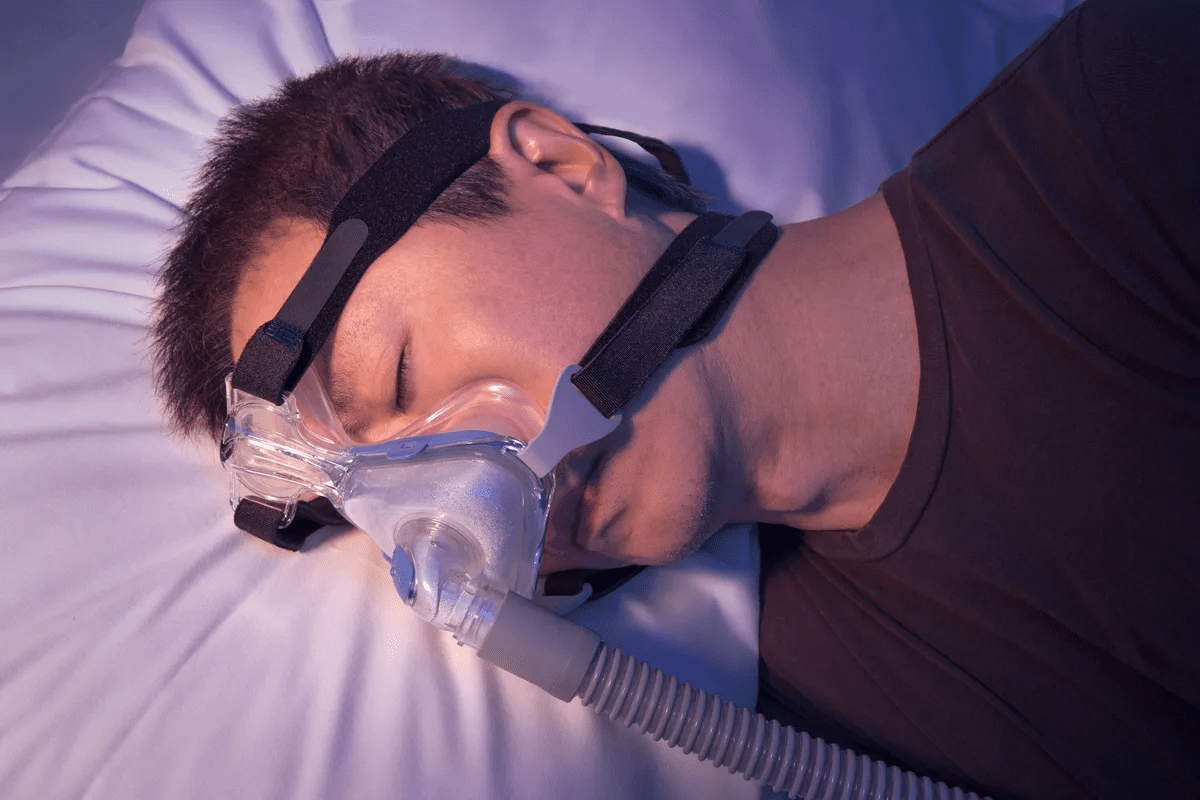
Sleep apnea is a disorder that causes breathing to stop during sleep. Symptoms include snoring, morning headaches, and feeling tired during the day. If CPAP therapy doesn’t work or is too hard to use, surgical interventions can help.
We know that sleep apnea surgery includes many procedures for treating obstructive sleep apnea. It’s important to understand these options if you’re looking for relief from this condition.
What are your OSA surgery options for Obstructive Sleep Apnea, ranging from UPPP to Maxillomandibular Advancement.
Obstructive sleep apnea (OSA) is a common condition that can be serious if not treated. It happens when breathing stops and starts during sleep because of a blocked airway. This can happen many times a night, making sleep poor and affecting health.
OSA happens when throat muscles relax, blocking the airway. This can cause breathing to slow down or stop. The body then tries to breathe again, making loud noises like snoring.
The severity of OSA is measured by how often breathing stops during sleep. This is called the Apnea-Hypopnea Index (AHI). A higher AHI score means more severe sleep apnea.
Sleep apnea is a big health issue, affecting about 30 to 40 million adults in the U.S. Worldwide, it affects around 936 million people. Many cases go undiagnosed because people don’t know about it or mistake its symptoms.
Not treating sleep apnea can lead to serious health problems. These include a higher risk of stroke, heart attack, and high blood pressure. The lack of oxygen and sleep can harm the heart and blood vessels.
“Untreated sleep apnea can have devastating consequences on an individual’s health, stressing the need for early diagnosis and treatment.”
— American Academy of Sleep Medicine
The health effects of OSA show why it’s important to get checked if symptoms last. Early treatment can improve life quality and lower the risk of other health problems.
Surgery for obstructive sleep apnea (OSA) is an option when other treatments don’t work. First, doctors try treatments like CPAP therapy or oral devices. But if these don’t help, surgery might be the next step.
CPAP therapy is often the first treatment for OSA. But some people find it uncomfortable. For them, surgery could be a better choice. CPAP intolerance can be due to mask discomfort, trouble exhaling, or feeling trapped.
A study in the Journal of Clinical Sleep Medicine showed about 50% of CPAP users had trouble with it. For these patients, surgery could offer relief.
Some people keep having OSA symptoms even with treatment. Surgery can help by fixing the underlying problems. Surgical procedures like removing tissue, moving the jaw, or using nerve stimulation can help manage OSA.
“Surgical intervention for OSA is not a one-size-fits-all solution; it requires careful evaluation and personalized planning to address the unique anatomical and physiological characteristics of each patient.”
Some body features might mean a person needs surgery for OSA. These include nasal blockage, a narrow throat, a big tongue, or a jaw that’s too far back. Surgery can be customized to fix these issues.
Anatomical Factor | Surgical Option | Potential Benefit |
Nasal Obstruction | Septoplasty or Turbinate Reduction | Improved Nasal Breathing |
Narrow Oropharynx | Uvulopalatopharyngoplasty (UPPP) | Enlarged Airway |
Enlarged Tongue | Tongue Reduction Surgery | Reduced Obstruction |
Recessed Lower Jaw | Maxillomandibular Advancement (MMA) | Advanced Lower Jaw Position |
Understanding the body’s features that cause OSA helps doctors suggest the right surgery. This can lead to better results for patients.
The first step to fight sleep apnea with surgery is a detailed consultation. This step is key to finding the right surgery for you.
It’s important to find a sleep apnea surgery expert. Look for a surgeon who is board-certified and has lots of experience with OSA. A skilled specialist can handle tough cases and give you the care you need.
When looking for a specialist, think about their reputation, patient feedback, and methods. Making a smart choice can greatly improve your surgery’s success.
At your consultation, ask important questions to understand the surgery. Some key ones are:
Asking these questions helps you make a well-informed choice and know what to expect.
It’s important to have realistic hopes for surgery. Surgery can greatly help sleep apnea, but it’s not a sure fix. How well it works depends on your OSA level, body shape, and health.
Your surgeon will look at your case and talk about what surgery can do. Knowing what’s possible and what’s not helps you get ready for what’s next.
To see if you’re a good candidate for sleep apnea surgery, we need to check your condition closely. This step is key to figuring out if surgery is the best choice for you.
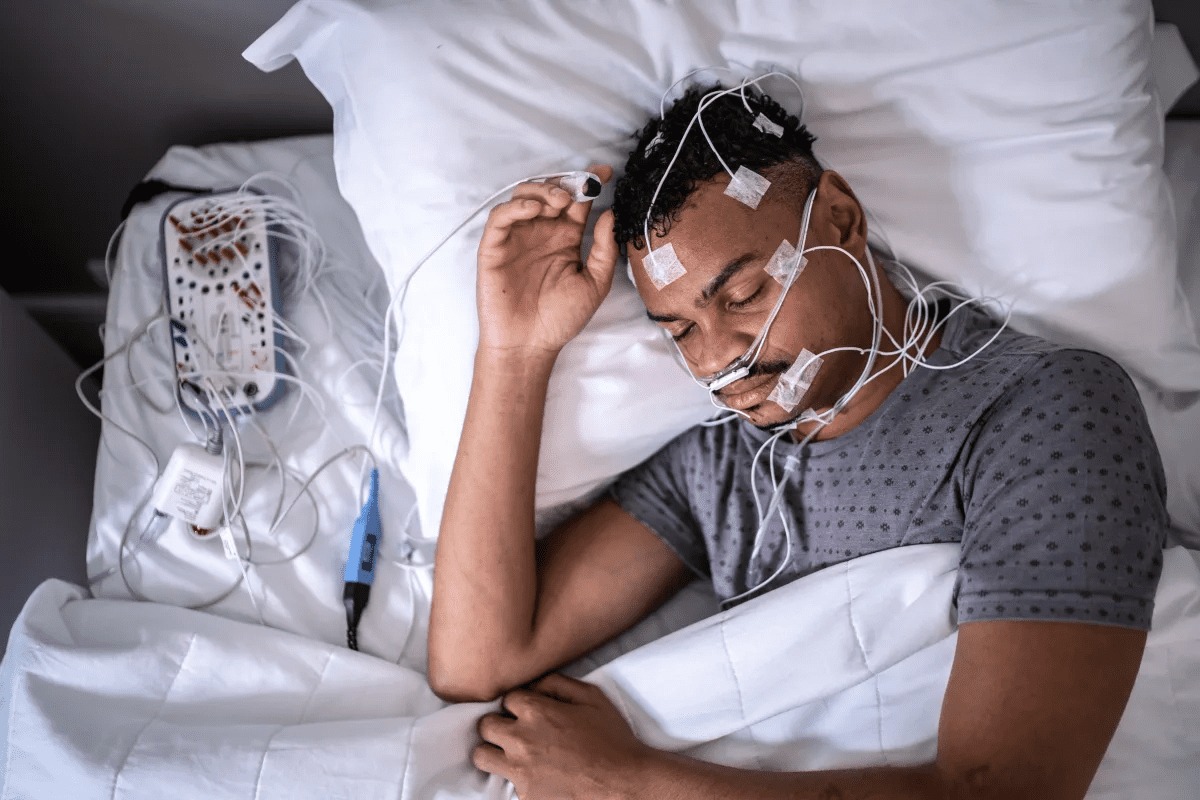
We do several tests and evaluations to see if you’re a good fit for surgery. These might include a nasopharyngoscopy or a sleep endoscopy. These tests let us see your upper airway and find any problems that might be causing your sleep apnea.
Diagnostic tests are very important for planning your surgery. They show us how bad your sleep apnea is and what parts of your airway need fixing during surgery.
Several things decide if you can have sleep apnea surgery. These include how bad your sleep apnea is, your overall health, and if you’ve tried other treatments before.
Factor | Description | Importance |
Severity of Sleep Apnea | Measured by the Apnea-Hypopnea Index (AHI) | High |
Overall Health | Presence of comorbidities like hypertension or diabetes | High |
Previous Treatments | Failure or intolerance to CPAP or other conservative treatments | Medium |
Sleep studies are very important for planning your surgery. They give us detailed info about your sleep patterns. This helps us customize the surgery to fit your needs.
By looking at sleep study data, we can figure out the best surgery plan. This way, we make sure we’re making the right choices for you.
When thinking about surgery for obstructive sleep apnea (OSA), it’s key to know your options. These surgeries aim to fix the physical blockages that disrupt sleep.
There are several ways to treat OSA through surgery. These include reducing tissue, moving the jaw, and using nerve stimulation. Each method targets different parts of the airway to stop blockages during sleep.
Tissue reduction surgeries, like uvulopalatopharyngoplasty (UPPP), remove or shrink throat tissue that blocks the airway. Jaw repositioning surgeries, such as maxillomandibular advancement (MMA), move the jaw forward to keep the airway open. Nerve stimulation therapies, like hypoglossal nerve stimulation, use a device to control the tongue and other muscles to prevent blockages.
OSA surgeries can be single-level or multi-level. Single-level surgeries focus on one area, while multi-level surgeries tackle several spots in the airway.
A study in the Sleep Medicine Reviews journal shows the importance of knowing where the blockage is. It points out that multi-level surgery is now seen as a good option for some patients.
“The concept of multilevel surgery is based on the understanding that OSA is often a multifactorial problem, requiring a complete treatment plan.”
Sleep Medicine Reviews
Choosing the right surgery for OSA means looking at the patient’s anatomy, how severe their OSA is, and their overall health. A tailored approach makes sure the surgery fits the patient’s specific needs.
Surgical Procedure | Target Area | Benefits |
Uvulopalatopharyngoplasty (UPPP) | Throat tissue | Reduces tissue obstruction |
Maxillomandibular Advancement (MMA) | Jaw | Significantly enlarges airway |
Hypoglossal Nerve Stimulation | Tongue and upper airway muscles | Prevents tongue obstruction during sleep |
Understanding the different surgeries and matching them to each patient’s needs helps healthcare providers treat OSA effectively. This improves patients’ lives and outcomes.
Sleep apnea can be managed with nasal surgeries. These surgeries fix problems in the nose that cause sleep issues. Fixing these problems can help reduce sleep apnea symptoms.
Septoplasty fixes a deviated nasal septum, a common cause of blocked nose. Turbinate reduction makes the turbinate bones smaller. Both help air flow better through the nose.
Benefits: Better airflow, less nasal resistance, and possibly better sleep.
Nasal valve surgery fixes the nasal valve area. This area is key for airflow. Problems here can lead to breathing issues and sleep problems.
Procedure: The surgery strengthens or rebuilds the nasal valve area for better airflow.
Research is ongoing on nasal surgeries for OSA treatment. Some studies show they can help, but others have mixed results.
Surgical Procedure | Potential Benefits | Effectiveness for OSA |
Septoplasty | Improved nasal airflow | Variable |
Turbinate Reduction | Reduced nasal resistance | Moderate |
Nasal Valve Surgery | Enhanced nasal valve function | Promising |
Nasal surgeries might help manage sleep apnea by fixing nose problems. But, talk to a doctor before deciding on surgery.
Palatal and throat procedures are common treatments for sleep apnea. They aim to remove the blockage that causes sleep apnea. This improves sleep quality and overall health.
UPPP is the most common surgery for sleep apnea. It removes or shrinks parts of the tonsils, uvula, and soft palate. This widens the airway, reducing sleep apnea symptoms.
Key aspects of UPPP include:
Palatal advancement is a surgical technique for sleep apnea. It moves the palate forward to enlarge the airway. This prevents the airway from collapsing during sleep, reducing apneic events.
The benefits of palatal advancement include:
Tonsillectomy and adenoidectomy remove the tonsils and adenoids. These procedures are common in children with sleep apnea. They widen the airway, reducing sleep apnea obstruction.
Recovery from these surgeries varies by surgery and patient health. Patients may experience discomfort, swelling, and throat pain. Success rates are high, with many seeing a big drop in sleep apnea symptoms.
Success rates are influenced by:
Choosing surgery is a big decision. It’s important to talk to a healthcare professional to find the best treatment for you.
When the tongue blocks the airway, surgery can help. These surgeries target the tongue area. They are used when the tongue blocks the airway during sleep.
Genioglossus advancement moves the genioglossus muscle forward. This stops the tongue from blocking the airway at night. It’s a good option for some patients with OSA.
Tongue reduction surgery makes the tongue smaller. This reduces airway blockage. Techniques include radiofrequency ablation and surgery. Tongue reduction helps when the tongue blocks the airway.
Hyoid suspension moves the hyoid bone to widen the airway. It helps by keeping the tongue and other structures from blocking the airway. This makes breathing easier during sleep.
These surgeries are for those with OSA caused by tongue blockage. Tests like sleep studies and imaging find the right candidates. A detailed check is key to choose the best surgery.
Surgical Procedure | Description | Benefits |
Genioglossus Advancement | Advancing the genioglossus muscle to prevent tongue obstruction | Reduces OSA severity by preventing tongue fallback |
Tongue Reduction | Reducing tongue size to minimize airway obstruction | Effective for patients with a large tongue contributing to OSA |
Hyoid Suspension | Repositioning the hyoid bone to expand the airway | Improves airway patency by stabilizing the hyoid bone |
A leading sleep specialist says,
“Tongue-based surgical interventions offer a valuable treatment option for patients with OSA who have not responded to other therapies.”
Knowing about these surgeries helps patients and doctors choose the best treatment for OSA.
New surgical methods, like hypoglossal nerve stimulation, offer hope for those with OSA. This treatment involves a device that stimulates the hypoglossal nerve. It helps control the tongue and keeps the airway open during sleep.
The device works with the patient’s breathing. It senses when the patient is about to breathe in. Then, it sends a signal to the hypoglossal nerve, moving the tongue forward to prevent airway blockage.
This method is great for those who can’t use CPAP therapy or have tongue base obstruction.
The procedure starts with general anesthesia. Then, incisions are made to place the device. This includes a nerve stimulator, a sensing lead, and a breathing sensor.
The surgery is usually done on an outpatient basis. Patients are watched for a few hours before going home.
Studies show hypoglossal nerve stimulation works for over 80% of patients. They see a big drop in sleep apnea symptoms and better sleep quality. This improves their overall life quality.
Outcome Measure | Pre-Implantation | Post-Implantation |
Apnea-Hypopnea Index (AHI) | 30.4 ± 15.6 | 9.2 ± 6.4 |
Oxygen Desaturation Index (ODI) | 25.8 ± 14.2 | 7.4 ± 5.6 |
Patient Satisfaction Score | 2.1 ± 1.1 | 4.5 ± 0.8 |
After the implant, the device is fine-tuned for the best results. This means adjusting the stimulation to control the airway without discomfort.
Regular check-ups are key to adjusting the device. They help monitor how the patient is doing and watch for any side effects.
Skeletal surgeries, like maxillomandibular advancement, are a good option for those with severe sleep apnea. Maxillomandibular advancement (MMA) moves the upper and lower jaws forward. This makes the airway bigger, helping to lessen sleep apnea symptoms.
The MMA procedure widens the airway by moving the jaws forward. It helps reduce sleep apnea by removing blockages. It also can improve facial structure in some cases. The main benefit of MMA is its ability to greatly reduce OSA in selected patients.
We look at several things when deciding if MMA is right for a patient. These include how severe their OSA is, their overall health, and any treatments they’ve tried before.
Recovery from MMA surgery varies, but it usually takes a few weeks. During this time, patients might feel swollen, uncomfortable, and need to stick to a liquid diet. Following post-operative instructions carefully is key to avoiding complications and ensuring a smooth recovery.
Recovery Stage | Timeline | Expectations |
Immediate Post-Surgery | 1-2 weeks | Swelling, discomfort, liquid diet |
Early Recovery | 2-6 weeks | Gradual return to normal diet, reduced swelling |
Late Recovery | 6-12 weeks | Return to normal activities, continued improvement in symptoms |
Research shows MMA can greatly improve severe OSA symptoms. Many patients see a big drop in apnea-hypopnea index (AHI) scores. The success of MMA over time depends on following post-operative care and attending follow-up appointments.
It’s important to know the risks of OSA surgery before deciding. Surgery can greatly improve life for those with obstructive sleep apnea. But, it’s key to understand the possible complications.
Patients may face swelling, pain, and throat discomfort after surgery. Some might notice voice changes or trouble swallowing.
Talking to your surgeon about these side effects can help you know what to expect.
Though rare, serious issues can happen. These include infections, bleeding, or bad reactions to anesthesia. Sometimes, surgery might not solve the sleep apnea problem, leading to ongoing symptoms.
Knowing these risks and discussing them with your doctor is vital.
To lower surgery risks, follow your surgeon’s advice carefully. This means going to follow-up visits and telling your doctor about any odd symptoms.
Also, staying healthy with a good diet and exercise helps your recovery.
Recovering from OSA surgery can be tough. You might need to change your daily life and face pain or discomfort.
Knowing these challenges can help you prepare and make recovery easier.
Complication | Description | Prevention/ Management |
Infection | Bacterial or viral infection at the surgical site | Antibiotics, proper wound care |
Bleeding | Excessive bleeding during or after surgery | Monitoring, surgical intervention if necessary |
Adverse Reaction to Anesthesia | Reaction to the anesthesia used during surgery | Careful patient screening, alternative anesthesia options |
Sleep apnea surgery is a good option for many with obstructive sleep apnea (OSA). There are different sleep apnea surgery options to consider. It’s important to know what each procedure does.
Choosing the right procedure for sleep apnea or operation for sleep apnea depends on your symptoms. These can differ a lot from person to person. So, talking to a healthcare professional is key.
We suggest patients have detailed talks with their doctors. This helps find the best treatment for them. This way, they can decide if sleep apnea surgery is right. It can greatly improve their life and lower the risks of not treating OSA.
Knowing about the surgery options and what they can do helps. It’s a step towards managing your condition well.
Sleep apnea surgery is a treatment for obstructive sleep apnea (OSA) when other methods don’t work. We offer different surgeries based on what each person needs.
Yes, there are many surgeries for sleep apnea. These include nasal, palatal, throat, tongue, and skeletal surgeries.
Sleep apnea surgery is a way to treat OSA. It fixes problems that block the airway.
You might need OSA surgery if CPAP therapy doesn’t work for you. Or if you have symptoms that won’t go away. Or if your body needs a specific surgery.
Tests for sleep apnea surgery include sleep studies and imaging. They help find out how bad OSA is and what surgery is best.
Common surgeries for OSA include nasal surgeries and throat procedures. Tongue-based surgeries are also used.
Hypoglossal nerve stimulation is a new surgery. It uses a device to keep the airway open during sleep.
Maxillomandibular advancement is a surgery. It moves the upper and lower jaws to make the airway bigger.
OSA surgery can have risks like swelling and pain. Serious problems like bleeding and infection can also happen. We try to avoid these.
To get ready for surgery, find a good specialist. Ask questions and know what to expect. A full check-up before surgery is important.
Recovery after OSA surgery depends on the surgery. We help you deal with side effects and challenges during recovery.
We look at each case to see if you can have surgery. We consider your health and other conditions.
Surgery for sleep apnea works differently for everyone. We talk about how well each surgery works.
Yes, some surgeries like nasal and nerve stimulation are less invasive.
Sleep studies are key for diagnosing OSA and planning surgery. They help us tailor treatment to you.
Yes, if CPAP therapy doesn’t work for you, we can check if surgery is right for you.
National Center for Biotechnology Information. (2025). What Are Your Options for Sleep Apnea Surgery. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11476387/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us