At Liv Hospital, we know how important it is to tackle carcinoma in situ (CIS) of the bladder. It’s a serious, flat, noninvasive form of carcinoma that’s a big challenge for doctors. Essential facts on carcinoma in situ bladder (CIS), including its high-grade nature and standard treatment with BCG immunotherapy.
CIS is stage 0 cancer and doesn’t invade the bladder. But, if not treated, it can turn into invasive bladder cancer. We focus on accurate diagnosis and proven treatments, using top urology skills from around the world.
It’s key for both patients and doctors to understand CIS. We’ll look into the main facts about CIS. This includes what it is, why it matters, how to diagnose it, and treatment choices. Our goal is to give a full picture of this condition.
Key Takeaways
- CIS of the bladder is a high-grade, noninvasive urothelial carcinoma.
- It is considered stage 0 cancer but has a high risk of progressing.
- Accurate diagnosis and proven treatments are vital.
- Liv Hospital offers top urology care from around the world.
- Knowing about CIS is important for patients and doctors.
What is Carcinoma in Situ Bladder? Definition and Overview
CIS of the bladder, also known as urothelial carcinoma in situ, is a flat, high-grade lesion. It hasn’t invaded the bladder wall but is a big challenge. It’s seen as a step before invasive urothelial carcinoma, making it key in urology.
CIS is known for its aggressive nature and risk of turning into invasive cancer. Knowing about its definition, clinical implications, and how common it is is vital for managing it well.
Clinical Significance in Urology
CIS is significant because of its high-grade nature and risk of becoming invasive cancer. If not treated, CIS can lead to invasive cancer. It’s also linked to a high chance of coming back and getting worse, making early detection and treatment essential.
Key aspects of CIS that underscore its clinical significance include:
- High-grade cytology without invasion into the bladder wall
- Potential for progression to invasive urothelial carcinoma
- Association with a high risk of recurrence
- Need for prompt and effective treatment to prevent progression
Prevalence and Demographics
CIS makes up less than 3 percent of all urothelial neoplasms. Yet, it’s found alongside or after bladder cancer in 45 percent and 90 percent of cases, respectively. Knowing how common CIS is and who’s at risk is key.
The people most likely to get CIS are similar to those with bladder cancer. Factors that raise the risk include:
| Risk Factor | Description |
| Age | Increased risk with advancing age, typically over 60 years |
| Gender | Males are more commonly affected than females |
| Smoking History | Smoking is a significant risk factor for CIS and bladder cancer |
Understanding CIS’s definition, clinical importance, and how common it is helps healthcare providers manage it better. This improves patient outcomes.
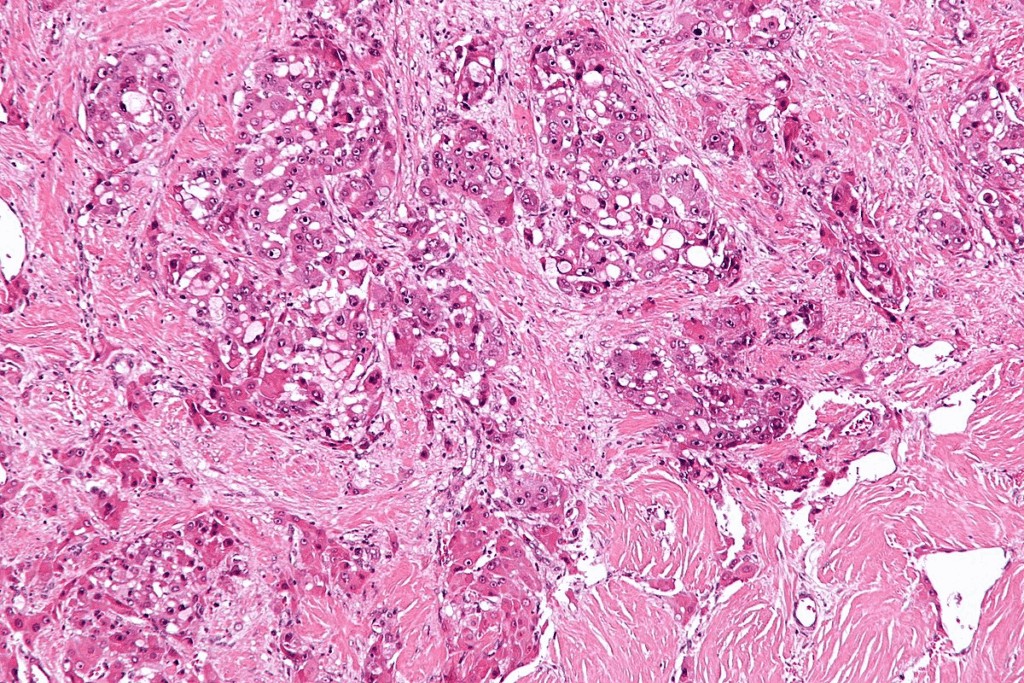
The Pathology of Bladder CIS: Cellular Characteristics
To understand CIS bladder cancer, we must look at its cell features and molecular markers. Carcinoma in situ (CIS) is a serious, non-invasive bladder cancer. It hasn’t broken through the basement membrane yet. Knowing about its pathology helps in early detection and treatment.
Histological Features
The features of CIS are key for its diagnosis. CIS shows marked nuclear enlargement, hyperchromasia, and loss of cellular polarity in the urothelium. These abnormal cells stay in the epithelial layer and haven’t invaded deeper tissues. The urothelium looks disordered or chaotic, with cells showing a lot of pleomorphism.
Looking at the cells under a microscope is vital to tell CIS apart from other bladder issues. The diagnosis of CIS relies on these specific cell features.
Molecular and Genetic Markers
Molecular and genetic markers are also important in diagnosing and predicting CIS. Research has found genetic changes like TP53 mutations and FGFR3 alterations in CIS. These markers help predict if the cancer will grow and guide treatment choices.
Knowing the molecular traits of CIS helps us understand how it might react to treatments. For example, CIS with certain genetic changes might respond better to targeted therapies. Using molecular and genetic info in diagnosing and treating CIS is a big step forward in urology.
Essential Fact #1: Carcinoma in Situ Bladder is a High-Grade Precursor to Invasive Cancer
Carcinoma in situ (CIS) of the bladder is a serious condition. It can turn into invasive cancer if not treated. CIS looks flat and non-invasive, but it can be dangerous.
Progression Risk Without Treatment
People with CIS face a big risk of getting invasive cancer. Research shows many CIS patients will get muscle-invasive bladder cancer. This is a serious condition with a high risk of spreading and death.
Risk Factors for Progression:
- Presence of CIS in multiple locations within the bladder
- Coexistence with other bladder tumors
- Failure to respond to initial treatment
Relationship to Invasive Urothelial Carcinoma
CIS is linked to invasive urothelial carcinoma. It’s seen as a precursor. CIS and invasive urothelial carcinoma share genetic and molecular changes.
| Characteristics | CIS | Invasive Urothelial Carcinoma |
| Growth Pattern | Flat, non-invasive | Invasive, potentially metastatic |
| Grade | High-grade | High-grade |
| Molecular Alterations | Similar to invasive carcinoma | Complex genetic alterations |
It’s key to understand CIS and invasive urothelial carcinoma. Early and effective treatment can stop CIS from getting worse. This can lead to better outcomes.
Essential Fact #2: Classification and Types of CIS
Carcinoma in situ (CIS) of the bladder has different types based on its presentation and association with other bladder cancers. Knowing these classifications is key to finding the best treatment and predicting patient outcomes.
Primary (De Novo) CIS
Primary or de novo CIS happens without a history of bladder cancer. It’s often found during an initial check for symptoms like blood in the urine or trouble with urination. This type of CIS is aggressive and needs quick treatment.
Concurrent and Secondary CIS
Concurrent CIS is found at the same time as another bladder tumor, like a papillary urothelial carcinoma. Secondary CIS develops later, after treatment for a previous bladder cancer. Both types mean a higher risk of the cancer getting worse and need careful management.
Research shows that secondary CIS is more likely to turn into muscle-invasive disease than primary CIS. So, it’s important to watch these patients closely and treat them quickly.
Focal vs. Diffuse CIS
CIS can also be classified by how much of the bladder it affects. Focal CIS is in a small area, while diffuse CIS covers more of the bladder or is in many areas. Knowing if CIS is focal or diffuse is important because diffuse CIS is more likely to get worse and might need stronger treatment.
A study in a top urology journal found that patients with diffuse CIS are at a higher risk of developing muscle-invasive bladder cancer than those with focal CIS. This shows how important it is to accurately stage and classify CIS to plan the best treatment.
| Type of CIS | Description | Risk of Progression |
| Primary (De Novo) CIS | CIS without prior history of bladder cancer | High |
| Concurrent CIS | CIS diagnosed with another bladder tumor | High to Very High |
| Secondary CIS | CIS developing during follow-up for previously treated bladder cancer | Very High |
| Focal CIS | CIS limited to a small area | Moderate to High |
| Diffuse CIS | CIS involving a larger surface area or multiple areas | High to Very High |
A leading urologist says, “The classification of CIS bladder cancer is not just a matter of semantics; it has significant implications for treatment and prognosis.” Understanding CIS types is vital for creating effective treatment plans and improving patient outcomes.
Essential Fact #3: Signs, Symptoms, and Clinical Presentation
CIS bladder cancer shows different signs and symptoms. These signs are important for early detection and treatment. They help doctors find and treat the cancer early.
Common Symptoms
People with CIS bladder cancer might have blood in their urine, painful urination, and need to urinate often. These symptoms can really affect a person’s life. They should see a doctor right away.
Blood in the urine, or hematuria, is a common symptom. It can be seen with the naked eye or only under a microscope.
| Symptom | Description | Prevalence |
| Hematuria | Blood in the urine, can be microscopic or gross | Common |
| Painful Urination | Discomfort or pain while urinating | Frequent |
| Frequent Urination | Need to urinate more often than usual | Frequent |
| Urgent Need to Urinate | Sudden, intense need to urinate | Frequent |
Asymptomatic Presentation
Some people with CIS bladder cancer don’t show symptoms. They might find out about it during tests for other urinary problems or regular check-ups.
When to Seek Medical Attention
If you have symptoms like blood in your urine, painful urination, or need to urinate a lot, see a doctor. Early treatment can make a big difference.
If you notice unusual symptoms or have a history of bladder cancer, see a doctor. Quick action is important for managing CIS.
Essential Fact #4: Diagnostic Approaches for Bladder CIS
Diagnosing bladder CIS uses many methods, from looking directly at the bladder to studying tissue samples. It’s important to use different tools to find and treat bladder CIS correctly.
Cystoscopy and Blue Light Cystoscopy
Cystoscopy lets doctors see inside the bladder. They can spot any problems. Blue light cystoscopy makes cancer cells stand out by using a special dye.
A top urologist says, “Blue light cystoscopy has made finding bladder CIS easier. This means we can diagnose and treat it better.”
“The use of blue light cystoscopy has revolutionized the field of urology, enabling us to identify CIS more effectively.”
Urine Cytology and Urinary Biomarkers
Urine cytology checks urine for abnormal cells. But it’s not very good at finding CIS. Urinary biomarkers help by looking for proteins or genetic changes linked to bladder cancer.
| Diagnostic Method | Sensitivity for CIS | Specificity for CIS |
| Urine Cytology | Moderate | High |
| Urinary Biomarkers | High | Moderate |
Biopsy and Pathological Examination
A biopsy takes a tissue sample from the bladder. It’s the best way to diagnose CIS. The sample is then checked under a microscope for CIS signs.
Pathological examination is key to confirming CIS and figuring out its grade and stage. This info helps plan the best treatment.
Imaging Studies
Imaging like CT scans or MRI isn’t the main way to diagnose CIS. But, it helps see how far the disease has spread.
We mix these methods to accurately find and stage bladder CIS. This helps us create a treatment plan that fits each patient’s needs.
Essential Fact #5: The High Recurrence Rate of CIS Bladder Cancer
Carcinoma in situ (CIS) bladder cancer often comes back, making regular checks very important. The rate at which it comes back can vary a lot. Studies show it can happen from 17% to 89% of the time over five years.
Statistics on Recurrence
Knowing how often CIS bladder cancer comes back is key. It helps set realistic goals and plan for future care. The big difference in rates is because of many factors. These include the type of patients, treatments used, and how long they are followed.
| Study | Recurrence Rate | Follow-Up Period |
| Study A | 17% | 2 years |
| Study B | 50% | 5 years |
| Study C | 89% | 10 years |
Risk Factors for Recurrence
There are several reasons why CIS bladder cancer might come back. These include having cancer in many places, having had bladder cancer before, and not treating it well the first time.
- Multifocal Disease: If cancer is found in many parts of the bladder, it’s more likely to come back.
- Prior History: Having had bladder cancer before makes it more likely to come back.
- Inadequate Initial Treatment: If the first treatment didn’t work well, the cancer might come back more often.
Surveillance Protocols
Because CIS bladder cancer often comes back, it’s very important to keep checking on it. This usually means doing cystoscopy, urine tests, and imaging studies.
Good surveillance plans help catch when it comes back early. This means doctors can act fast and possibly improve treatment results.
Treatment Options for CIS of the Bladder
There are many ways to treat bladder CIS, from using medicines inside the bladder to surgery. The right treatment depends on how far the disease has spread, the patient’s health, and what treatments they’ve had before.
Intravesical BCG Therapy
Intravesical BCG (Bacillus Calmette-Guérin) therapy is a common treatment for CIS of the bladder. BCG is a weakened form of Mycobacterium bovis put directly into the bladder. It helps the body fight cancer cells.
Benefits of BCG Therapy:
- High response rate
- Ability to preserve bladder function
- Effective in reducing recurrence
Alternative Intravesical Treatments
If BCG doesn’t work or causes too many side effects, other treatments are available. These include:
- Intravesical chemotherapy
- Other immunotherapies
These treatments can be used alone or with other therapies.
Radical Cystectomy
When CIS doesn’t respond to treatments or is at high risk of getting worse, radical cystectomy might be suggested. This surgery removes the bladder and creates a new way for urine to leave the body.
Considerations for Radical Cystectomy:
- Significant lifestyle changes
- Potential for complications
- Impact on quality of life
Emerging Therapies
New treatments for CIS of the bladder are being researched. These include:
- Checkpoint inhibitors
- Gene therapy
- Targeted therapy
These new methods aim to better outcomes and lessen side effects.
Here’s a summary of the treatment options in a tabular format:
| Treatment Option | Description | Key Considerations |
| Intravesical BCG Therapy | Immunotherapy using weakened Mycobacterium bovis | High response rate, preserves bladder function |
| Alternative Intravesical Treatments | Chemotherapy or other immunotherapies | For BCG failures or intolerance |
| Radical Cystectomy | Surgical removal of the bladder | Significant lifestyle changes, possible complications |
| Emerging Therapies | Checkpoint inhibitors, gene therapy, targeted therapy | Ongoing research, possible better outcomes |
Prognosis and Survival Rates for Patients with Bladder CIS
Knowing the prognosis for carcinoma in situ (CIS) of the bladder is key. It’s important for both patients and doctors. The good news is that CIS bladder cancer has a good outlook when caught early and treated right.
Factors Affecting Prognosis
Many things can change how well CIS bladder cancer does. How well the first treatment works, any other health issues, and the patient’s overall health matter a lot. For example, those who do well with BCG therapy inside the bladder tend to do better.
Response to Treatment: How well the first treatment works is a big deal. Patients who get rid of the cancer completely after treatment usually do better than those who don’t.
Presence of Comorbidities: Having other health problems can also affect how well a patient does. Things like diabetes or heart disease can make treatment harder and change survival chances.
Five-Year Survival Statistics
The National Cancer Institute says that for patients with CIS alone, the five-year survival rate is 97 percent. This shows that CIS patients have a good chance of doing well if they get the right treatment.
But, survival rates can change based on many things. Like how early the cancer was found and the patient’s health.
Quality of Life Considerations
Even though CIS bladder cancer has a good outlook, how well patients feel is also important. Side effects from treatment and the emotional impact of finding out they have cancer can affect their quality of life.
Supportive Care: It’s vital to offer supportive care. This includes counseling and helping manage side effects. It helps improve the quality of life for CIS patients.
By knowing what affects prognosis and survival, doctors can give more tailored care. And patients can make better choices about their treatment.
Living with CIS: Management Strategies and Lifestyle Modifications
Living with CIS bladder cancer means using a mix of medical care, follow-up, and lifestyle changes. A good plan helps lower the chance of the cancer coming back or getting worse.
Follow-up Care
Getting regular check-ups is key to catching any problems early. People with CIS need to see a doctor every 3-6 months. This depends on their risk and how well they’re doing.
A study in the Journal of Urology found that regular check-ups help find CIS again early. This can lead to better treatment and results.
| Follow-up Interval | Procedure |
| 3-6 months | Cystoscopy |
| 6-12 months | Urine Cytology |
| Annually | Imaging Studies (e.g., CT Urogram) |
Coping with Treatment Side Effects
It’s important to handle the side effects of CIS treatment to keep living well. BCG therapy can make the bladder feel irritated, among other things. Talking to a doctor about these issues can help a lot.
“The key to managing CIS is not just about treating the cancer, but also about improving the patient’s quality of life,” said Dr. [Last Name], a leading urologist.
Support Resources
There are many ways to get help if you have CIS. Support groups, counseling, and online forums can offer emotional support and advice. They help you feel less alone and more connected.
- Support Groups: Local and online groups where patients can share their experiences and receive support.
- Counseling Services: Professional counseling to help patients cope with the emotional aspects of their diagnosis.
- Online Forums: Websites and forums dedicated to bladder cancer and CIS, where patients can ask questions and share information.
By following a detailed plan that includes regular check-ups, managing side effects, and using support, CIS patients can do better. They can live a better life despite their diagnosis.
Conclusion: The Importance of Early Detection and Treatment
Early detection and treatment of carcinoma in situ bladder cancer are key to stopping it from becoming invasive. We’ve covered important facts about CIS, like its definition, how it’s studied, and why it matters. CIS is a serious step before invasive cancer, and finding it early is vital for better patient results.
Bladder cancer CIS needs quick action because it can get worse. We stress the need for being aware and acting fast to handle CIS bladder cancer well. Using treatments like BCG and keeping an eye on the bladder are important steps.
Knowing about CIS risks and traits helps patients and doctors prevent it from getting worse. We urge people to see a doctor if they have symptoms or worry about their risk. This teamwork is essential in fighting CIS bladder cancer.
FAQ
What is carcinoma in situ (CIS) of the bladder?
CIS of the bladder is a flat, high-grade urothelial carcinoma. It has not invaded the bladder wall. It’s considered a precursor lesion for invasive urothelial carcinoma.
What are the symptoms of CIS bladder cancer?
Symptoms of CIS bladder cancer include hematuria, dysuria, and frequency. Some patients may not show any symptoms.
How is CIS bladder cancer diagnosed?
Diagnosing CIS involves several steps. These include cystoscopy, urine cytology, and pathological examination of biopsy samples.
What are the treatment options for CIS of the bladder?
Treatment options for CIS include intravesical therapies like BCG. Other options include alternative intravesical treatments and surgical interventions such as radical cystectomy.
What is the prognosis for patients with CIS bladder cancer?
The prognosis for CIS bladder cancer depends on several factors. These include response to treatment and presence of comorbidities. Overall survival rates vary based on these factors.
How can CIS bladder cancer be managed and what lifestyle modifications are recommended?
Managing CIS involves regular follow-up care and coping with treatment side effects. Lifestyle modifications are also recommended. Support resources are available to patients.
What is the risk of CIS progressing to invasive cancer if left untreated?
CIS is considered a high-grade lesion. It has a high risk of progressing to invasive urothelial carcinoma if not treated promptly.
What is the difference between primary, concurrent, and secondary CIS?
Primary CIS occurs alone. Concurrent CIS is found with other bladder cancers. Secondary CIS develops after previous bladder cancer. Each type has different implications for treatment.
How often does CIS bladder cancer recur?
CIS bladder cancer has a high recurrence rate. Even after successful initial treatment, it can recur. Regular surveillance and follow-up care are necessary.
What are the emerging therapies for CIS bladder cancer?
Emerging therapies for CIS include new intravesical treatments and immunotherapies. These offer alternatives for patients who do not respond to standard treatments.
Can CIS bladder cancer be asymptomatic?
Yes, some patients with CIS bladder cancer may be asymptomatic. Regular check-ups and screenings are important for early detection.
What is the role of cystoscopy in diagnosing CIS?
Cystoscopy, including blue light cystoscopy, is key in diagnosing CIS. It allows visualization of the bladder mucosa and identification of abnormal areas.
References
National Center for Biotechnology Information – https://pubmed.ncbi.nlm.nih.gov/35353130/y








