We understand the importance of carcinoma in situ (CIS). It’s a serious type of bladder cancer that stays in the bladder lining. CIS is a non-muscle-invasive cancer that hasn’t spread yet. 5 key facts about bladder cancer in situ, including the use of cystoscopy and biopsy for diagnosis of this Stage 0 tumor.
Getting it early is key because CIS can turn into invasive cancer if not treated. At Liv Hospital, we offer top-notch care and expertise. We help manage and treat complex cancers.
Knowing about CIS is vital for its treatment. We stress the need for awareness and quick action. This helps stop it from getting worse.
Key Takeaways
- CIS is a high-grade urothelial malignancy confined to the urothelium.
- Early diagnosis is critical to prevent progression to invasive carcinoma.
- Patient-centered care is essential for effective management of CIS.
- Liv Hospital provides thorough evaluation and management for complex malignancies.
- Timely intervention is key to prevent progression.
What is Bladder Cancer In Situ? Definition and Characteristics

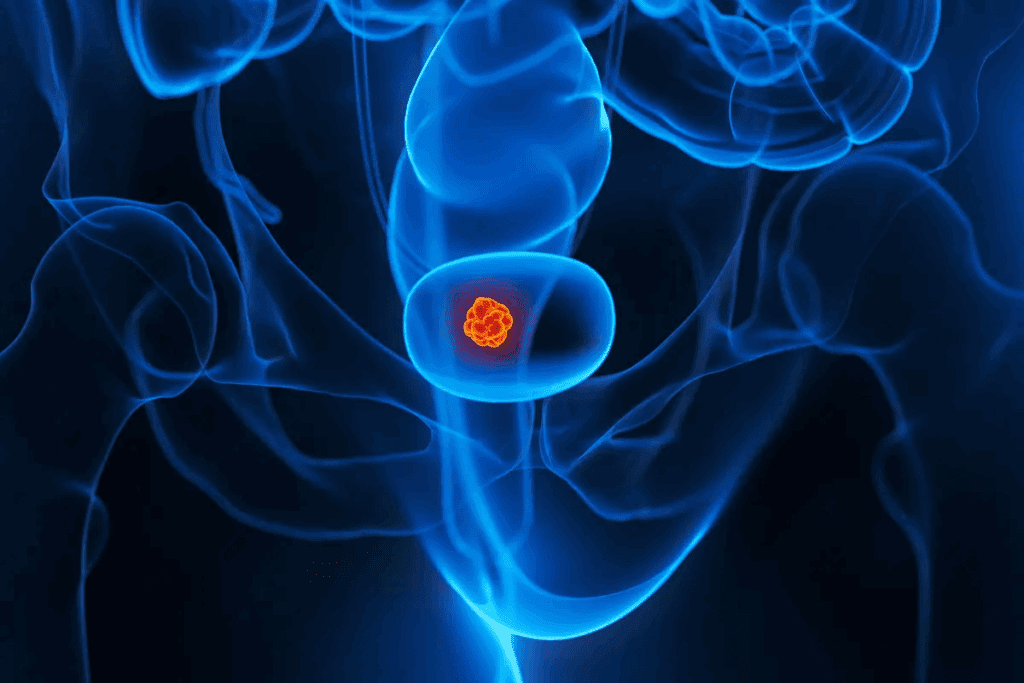
Bladder cancer in situ, or urothelial carcinoma in situ (CIS), is a non-invasive cancer. It is considered high-grade and has a higher risk of coming back and growing. This type of cancer is found in the bladder and is a serious concern.
Urothelial carcinoma in situ is a flat lesion with high-grade malignant cells. These cells are found only in the urothelium. This is what makes CIS different from other bladder cancers.
Flat Lesion Characteristics of CIS
CIS lesions are flat, making them hard to spot with regular methods. They spread like a thin sheet over the urothelium, often without forming visible tumors. The flat nature of CIS is what sets it apart from other bladder cancers.
Distinction from Other Bladder Cancer Types
CIS is different from other bladder cancers because of its flat look and high-grade malignancy. Unlike papillary tumors, CIS doesn’t grow outwards. Instead, it changes the urothelial lining, which can be found with special tests.
Potential for Progression to Invasive Carcinoma
One big worry with CIS is that it can turn into invasive carcinoma if not treated right. The high-grade cells in CIS mean there’s a higher chance of it spreading into the bladder wall. Catching it early and treating it right is key to stopping this from happening.
Key Fact #1: Epidemiology and Demographics of Bladder CIS
To understand bladder CIS, we need to look at its epidemiology. Bladder CIS, or carcinoma in situ, is a serious cancer that doesn’t grow into the bladder wall. Knowing about it helps us find who’s at risk and how to prevent it.
Prevalence Rate: Less Than 3% of De Novo Cases
De novo CIS makes up less than 3 percent of bladder cancers. This shows how important it is to find CIS correctly among other bladder issues.
Studies show CIS is found in a small number of bladder cancers. This means CIS is often missed or wrongly diagnosed. We need better ways to find it early.
Male to Female Ratio (7:1) and Age Distribution
Men are 7 times more likely to get CIS than women, with an average age of 65.6 years. Knowing this helps us understand who’s at risk.
| Demographic Characteristic | Value |
| Male to Female Ratio | 7:1 |
| Mean Age at Diagnosis | 65.6 years |
Risk Factors Associated with CIS Development
Smoking and exposure to chemicals increase CIS risk. These are key to figuring out why CIS happens and how to stop it.
“Smoking is a well-established risk factor for bladder cancer, including CIS. The chemicals in tobacco smoke can damage the bladder’s lining, leading to cancerous changes over time.”
Source: American Cancer Society
Knowing these risks helps us catch CIS early. People who smoke or are exposed to chemicals should be watched closely for CIS signs.
Key Fact #2: Clinical Presentation and Anatomical Distribution
It’s important to know how bladder cancer in situ (CIS) shows up and where it usually happens. This knowledge helps find it early and treat it well. We’ll look at how CIS shows up and where it likes to be in the bladder.
Multifocality in 50% of Cases
CIS often shows up in many places, in about 50% of cases. This makes it hard to diagnose and treat because it can affect many parts of the bladder lining.
Predilection Sites: Trigone, Lateral Wall, and Dome
CIS has a preference for certain spots in the bladder. It usually likes the trigone, lateral wall, and dome. Knowing this helps doctors find it more easily.
Symptom Patterns and Detection Challenges
The signs of CIS can be tricky to spot because they’re similar to other bladder issues. Symptoms include blood in the urine, pain while urinating, needing to go often, and a sudden urge to urinate. CIS looks like inflammation, making it hard to diagnose.
| Symptom | Description | Frequency |
| Hematuria | Blood in the urine | Common |
| Painful Urination | Pain or discomfort while urinating | Frequent |
| Frequent Urination | Need to urinate more often than usual | Frequent |
| Urgent Urination | Sudden, urgent need to urinate | Frequent |
We need to understand these signs and where CIS likes to be to better find and treat it.
Key Fact #3: Primary vs. Secondary Bladder Cancer In Situ
It’s important to know the difference between primary and secondary bladder cancer in situ. This knowledge helps doctors diagnose and treat the disease better. Bladder CIS can show up in different ways, which affects how it’s handled.
De Novo (Primary) CIS: Presentation Without Papillary Tumors
Primary CIS, or de novo CIS, doesn’t have a history of papillary tumors. It looks like a flat lesion, making it hard to spot with regular methods. This type of CIS is a serious cancer without the usual papillary shape.
Research shows primary CIS is aggressive and can turn into invasive cancer if not treated. So, finding it early and acting fast is key.
Secondary CIS: Association with Existing Urothelial Carcinoma
Secondary CIS is linked to existing or past urothelial carcinoma. It often appears with papillary or invasive tumors. This makes treatment plans more complex, suggesting a bigger or recurring disease.
Secondary CIS is more common than primary CIS, mainly in people with bladder cancer history. Finding it needs a detailed check, including cystoscopy and biopsy.
Concurrent vs. Secondary Detection Patterns
CIS detection patterns differ, affecting treatment and outlook. Concurrent CIS is found at the same time as the main tumor. Secondary CIS is spotted later, often during follow-ups.
| Characteristics | Primary CIS | Secondary CIS |
| Presentation | Without papillary tumors | Associated with existing urothelial carcinoma |
| Detection | Often challenging due to flat lesions | May be detected during follow-up for existing tumors |
| Prognosis | High risk of progression if untreated | Indicates potentially widespread or recurrent disease |
A leading urologist notes,
“The difference between primary and secondary CIS is not just for learning; it’s vital for treatment planning and patient results.”
In conclusion, knowing the differences between primary and secondary bladder CIS is critical for good treatment plans. By understanding these differences, doctors can better help their patients.
Key Fact #4: Diagnostic Challenges in CIS Detection
Diagnosing bladder cancer in situ (CIS) is tough because it looks flat and can be mistaken for inflammation. Doctors use different tools and methods to find CIS. Each has its own good points and weaknesses.
Limitations of Conventional White Light Cystoscopy
White light cystoscopy (WLC) is the usual way to spot bladder cancer, including CIS. But, WLC can miss CIS because it looks flat. The flat lesions of CIS can be subtle and may not be readily visible, making it hard to spot with WLC alone.
Urine Cytology: Sensitivity and Specificity
Urine cytology is a key tool, mainly for high-grade tumors like CIS. It checks urine for abnormal cells. The sensitivity of urine cytology for CIS is relatively high, but it can be tricky because of false positives from benign conditions.
Biopsy Requirements and Sampling Considerations
Biopsy is the best way to confirm CIS. It takes tissue samples from the bladder lining for detailed checks. Adequate sampling is key to get a correct diagnosis, as CIS can be scattered. Often, more than one biopsy is needed to confirm CIS.
Key Fact #5: Advanced Diagnostic Techniques for CIS
We are seeing big steps forward in how we diagnose CIS. New ways to detect and manage CIS are being developed. These advancements are key to better treating this condition.
Enhanced Cystoscopy Methods
New cystoscopy methods, like fluorescence cystoscopy, are playing a big role. They help us see lesions that regular cystoscopy can’t. This is a big deal for spotting CIS early.
Fluorescence cystoscopy uses a special agent that lights up cancer cells. This makes them stand out during the procedure. It’s great for finding CIS, even when it’s flat or hard to see.
Molecular Markers and Emerging Technologies
Molecular markers are also a big deal in CIS diagnosis. They can be found in urine or tissue. They help make diagnosis more accurate.
New molecular markers for CIS include proteins and genetic changes linked to urothelial carcinoma. Scientists are working hard to find the best markers. They aim to create tests that doctors can use every day.
| Diagnostic Technique | Description | Advantages |
| Fluorescence Cystoscopy | Uses fluorescent agents to highlight cancerous cells | Improved visibility of flat lesions, enhanced detection of CIS |
| Molecular Markers | Detects specific proteins or genetic mutations in urine or tissue | Potential for non-invasive diagnosis, improved accuracy |
Using these new diagnostic tools in clinics could change how we treat CIS. Better detection means we can offer more effective treatments to patients.
Histopathological Features of Urothelial Carcinoma In Situ
Understanding the histopathological features of urothelial carcinoma in situ is key for accurate diagnosis and treatment planning. The diagnosis of CIS relies heavily on examining tissue samples from biopsies.
Microscopic Characteristics of High-Grade Malignant Cells
CIS is marked by high-grade malignant urothelial cells in the urothelium. These cells have large nuclei, irregular shapes, and big nucleoli. They often don’t line up properly and can go all the way through the urothelium.
The microscopic look shows a range of changes, from mild to severe anaplasia. The presence of these high-grade cells is a key sign of CIS, setting it apart from less serious urothelial lesions.
Immunohistochemical Markers for Confirmation
In some cases, immunohistochemical markers help confirm CIS diagnosis. Markers like CK20, p53, and Ki-67 help spot malignant cells and tell CIS apart from reactive changes. These markers are very helpful when it’s hard to tell by just looking at the cells.
For example, CIS often shows a lot of p53, which means it’s a high-grade cancer. Also, a high Ki-67 score helps tell CIS apart from non-cancerous conditions.
Differential Diagnosis Considerations
When diagnosing CIS, it’s important to rule out other urothelial lesions. This includes benign changes, dysplasia, and invasive cancer. A detailed look at the cells is needed to tell CIS apart from these other conditions.
Important things to look for include nuclear atypia, the urothelium’s disorganized look, and no invasion into the lamina propria. Immunohistochemical staining can also help clear up any doubts.
Imaging Modalities in CIS Assessment
Imaging plays a key role in diagnosing and staging bladder cancer in situ (CIS). Accurate diagnosis and staging help choose the right treatment. This improves patient outcomes.
Role and Limitations of CT Urography
CT urography is a valuable tool for checking the upper urinary tract in bladder CIS. It gives detailed images of the urinary system. This helps spot any abnormalities or tumors.
Key benefits of CT urography include:
- High sensitivity for detecting upper tract urothelial carcinoma
- Ability to assess the entire urinary tract in a single examination
- Detailed visualization of the bladder and surrounding structures
But, CT urography has its downsides. It involves radiation and can cause kidney problems due to contrast.
MRI Applications in Bladder Cancer Staging
MRI is also key in staging bladder cancer. It gives high-resolution images of the bladder and nearby tissues. This helps figure out how far the tumor has spread.
MRI is useful for:
- Assessing the depth of tumor invasion into the bladder wall
- Identifying lymph node involvement
- Evaluating the presence of distant metastases
MRI gives important info for treatment planning. It helps decide if radical cystectomy or other treatments are needed.
Upper Tract Evaluation Importance
Checking the upper tract is vital in managing bladder CIS. Imaging tools like CT urography are key in spotting upper tract involvement.
Regular upper tract checks are essential for bladder CIS patients. They help catch any upper tract issues early.
Treatment Approaches for Bladder CIS
There are many ways to treat bladder CIS. Each method has its own benefits and things to consider. Understanding these options helps doctors tailor treatment to each patient’s needs.
Intravesical BCG Therapy: The Gold Standard
Intravesical Bacillus Calmette-Guérin (BCG) therapy is the top choice for treating CIS. It involves putting a weakened form of the Mycobacterium bovis bacterium into the bladder. This treatment helps the body fight and destroy cancer cells.
Benefits of BCG Therapy:
- High response rate for CIS patients
- Ability to preserve bladder function
- Potential to delay or prevent progression to invasive cancer
Management of BCG-Unresponsive Disease
Some patients may not respond to BCG therapy or may have it come back. For these cases, other treatments are needed. Options include:
- Intravesical chemotherapy
- Device-assisted therapies
- Clinical trials of new agents
Role of Radical Cystectomy
Radical cystectomy, or removing the bladder, is an option for those who don’t respond to BCG or are at high risk. It’s a big surgery but can save lives.
Considerations for Radical Cystectomy:
| Factor | Consideration |
| Patient Health | Overall health and ability to undergo major surgery |
| Cancer Stage | Extent of cancer spread and the chance for a cure |
| Quality of Life | Impact on urinary and sexual function, and overall well-being |
Emerging Treatment Approaches
New treatments for bladder CIS are being researched. These include:
- Immunotherapies beyond BCG
- Targeted therapies
- Gene therapies
These new treatments offer hope for better outcomes and quality of life for patients with bladder CIS.
Surveillance Protocols and Recurrence Monitoring
Surveillance protocols are key in managing bladder CIS. They help catch recurrence early. Regular checks are vital for those with bladder CIS to spot any return quickly.
Follow-up Cystoscopy Schedules
Follow-up cystoscopy is essential for bladder CIS surveillance. Guidelines suggest cystoscopy every 3-6 months for the first two years after diagnosis or treatment. The schedule might change based on the patient’s risk and treatment response.
For example, those with a history of high-grade CIS or who’ve had intravesical therapy might need more checks. “Cystoscopy is the best way to find recurrence in bladder CIS,” say recent urology guidelines. It’s important for patients to keep their cystoscopy appointments to catch any recurrence early.
Urine Marker Surveillance
Urine marker tests are also important in follow-up care for bladder CIS. Markers like UroVysion and NMP22 help spot recurrence and track progression. They’re not a full replacement for cystoscopy but offer extra insight for doctors.
We combine urine marker tests with cystoscopy for better recurrence detection. This method offers a more detailed look at the patient’s condition, catching issues sooner than either test alone.
Long-term Monitoring Considerations
Long-term monitoring for bladder CIS needs a detailed plan. It’s important to remind patients of the need to stick to their surveillance schedule. Their health, any other health issues, and the specifics of their CIS all play a part in the monitoring strategy.
A leading urologist says, “Long-term surveillance is about more than just finding recurrence. It’s about keeping the patient’s health in check and adjusting treatment plans as needed.” We tailor surveillance plans for each patient, considering their unique needs and risks.
Conclusion: Future Directions in Bladder CIS Management
Understanding bladder cancer in situ (CIS) is key to better management and outcomes. CIS is a complex issue that needs a detailed approach to diagnosis and treatment.
New technologies and treatments show promise for CIS management. Ongoing research and advancements in bladder cancer care are expected to improve patient care. We’re moving towards more personalized and precise treatments for CIS, aiming to enhance quality of life and survival rates.
The future of CIS management will likely include advanced diagnostic tools, new therapeutic agents, and innovative strategies. By exploring these areas, we can better understand CIS and develop more effective management plans. This will lead to better outcomes for patients.
FAQ
What is bladder cancer in situ?
Bladder cancer in situ, also known as carcinoma in situ (CIS), is a serious type of bladder cancer. It stays in the bladder lining and can turn into invasive cancer if not treated.
What are the characteristics of CIS lesions?
CIS lesions are flat and often found in many places. They usually appear in the bladder’s trigone, lateral wall, and dome. About 50% of cases have multiple lesions.
How is CIS different from other types of bladder cancer?
CIS is unique because it’s a flat, serious cancer that only affects the bladder lining. Other bladder cancers can be papillary or invasive.
What are the risk factors associated with CIS development?
Smoking, exposure to certain chemicals, and a history of bladder cancer increase the risk of CIS.
How is CIS diagnosed?
Doctors use cystoscopy, urine cytology, and biopsy to diagnose CIS. A biopsy is checked to confirm the diagnosis.
What are the limitations of conventional white light cystoscopy in CIS detection?
White light cystoscopy can miss CIS because it’s hard to see flat lesions. Enhanced methods are needed for better detection.
What is the role of urine cytology in CIS diagnosis?
Urine cytology can spot abnormal cells. But it’s not very good at finding CIS.
What are the treatment options for CIS?
CIS can be treated with BCG therapy, managing BCG-resistant cases, or radical cystectomy. New treatments are also being explored.
How is CIS monitored after treatment?
After treatment, CIS is checked with cystoscopy, urine tests, and long-term monitoring. This helps catch any signs of recurrence or growth.
What is the prognosis for CIS?
CIS’s outcome depends on treatment success and risk factors. Research is ongoing to improve patient results.
What is urothelial carcinoma in situ?
Urothelial carcinoma in situ is another name for bladder cancer in situ or CIS. It’s a serious cancer that only affects the bladder lining.
What is the male to female ratio for CIS?
CIS is more common in men, with a ratio of about 7:1.
What is the role of CT urography in CIS assessment?
CT urography helps check the upper urinary tract for CIS involvement.
What is the role of MRI in bladder cancer staging?
MRI helps stage bladder cancer, including CIS. It checks the disease’s extent and for any invasion or spread.
References
National Center for Biotechnology Information. (2025). Bladder Cancer In Situ 5 Key Facts on. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4647140/








