Understanding urothelial carcinoma in situ is key for doctors and pathologists. It helps them spot this aggressive cancer correctly. Carcinoma in situ bladder cystoscopy: Learn how this procedure is used to visualize and biopsy the flat lesions of CIS.
At Liv Hospital, we know how serious CIS is. It mainly happens in the bladder and can turn into invasive carcinoma if not treated.
We focus on accurate diagnosis. Our goal is to give the best care and follow the latest research.
Key Takeaways
- Urothelial carcinoma in situ is a high-grade, high-risk form of urothelial cancer.
- Accurate diagnosis is key to stop it from becoming invasive carcinoma.
- Liv Hospital is dedicated to delivering evidence-based pathology insights.
- Patient-centered care is our top priority.
- We use the latest academic protocols for diagnosis and treatment.
Pathological Definition and Classification of Urothelial Carcinoma In Situ
Knowing how to define and classify Urothelial Carcinoma In Situ (CIS) is key for treating bladder cancer right. CIS is a flat growth on the bladder lining that hasn’t invaded the wall yet. But, it can turn into invasive cancer if not treated.
Historical Perspective and Evolution of CIS Diagnosis
The idea of CIS has changed a lot over time. It was first seen as a unique type of cancer because it could turn into invasive cancer. At first, doctors used urine samples to spot CIS. Now, we use more advanced tests like histopathology and immunohistochemistry.
Today, we know CIS has a different look and feel than normal bladder cells. This knowledge helps doctors spot CIS correctly.
Current WHO Classification Criteria
The World Health Organization (WHO) has set clear rules for diagnosing CIS. The WHO says CIS is when the bladder cells look very different and cover the whole lining. These cells are big, have big centers, and don’t look like normal cells.
The WHO rules help doctors tell CIS apart from other flat bladder issues. This is important for choosing the right treatment and knowing how the patient will do.
Clinical Significance in Bladder Cancer Management
Getting CIS right is very important for treating bladder cancer. CIS is a serious type of cancer that can quickly become worse. So, finding it early and treating it strongly is key.
Doctors need to understand CIS to take good care of their patients. Mixing what they find in tests with what they know about the patient helps make the best treatment plans.
Key Insight #1: Histomorphological Features of Urothelial Carcinoma In Situ

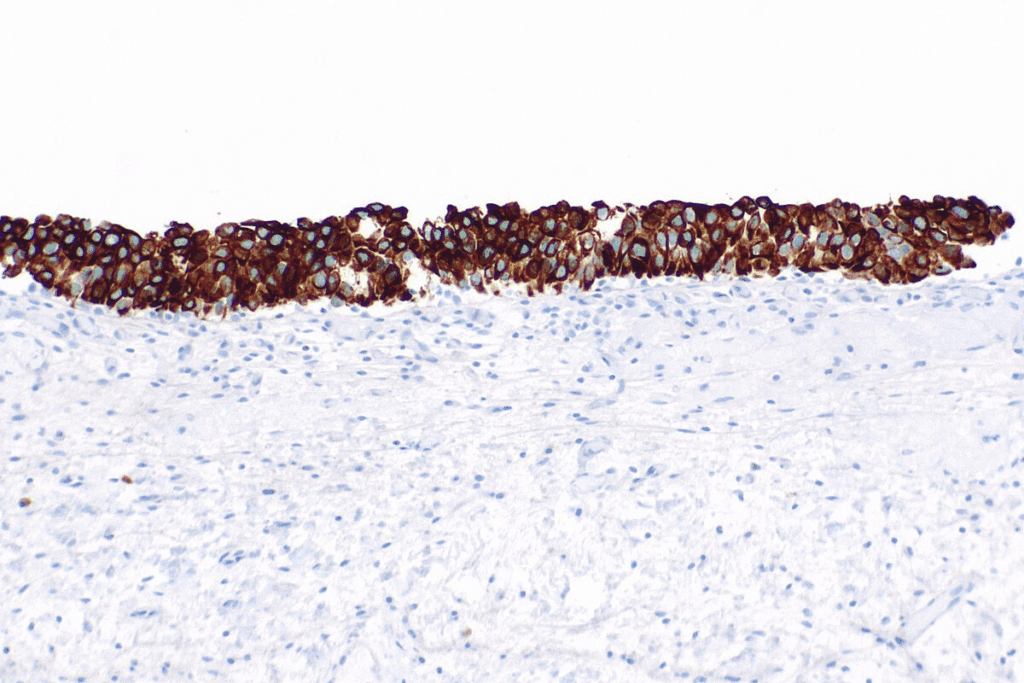
Understanding the histomorphological features of Urothelial Carcinoma In Situ is key for accurate diagnosis. Urothelial CIS is marked by malignant cells replacing the urothelium. These cells show severe nuclear atypia. The diagnosis of CIS relies on spotting these distinctive features.
Cellular Architecture and Organizational Patterns
The cells in CIS are disordered, often losing the normal urothelial maturation. They show significant nuclear pleomorphism, hyperchromasia, and an irregular nuclear-to-cytoplasmic ratio. The presence of large, irregular nuclei with prominent nucleoli is a hallmark of CIS.
Distinguishing CIS from Reactive Conditions
Distinguishing CIS from reactive urothelial atypia can be tricky. Reactive conditions have a more orderly pattern and less nuclear atypia than CIS. Immunohistochemical staining can be a useful adjunct in difficult cases. CIS often shows full-thickness staining for CK20, unlike reactive conditions.
“The distinction between CIS and reactive urothelial atypia requires careful histological examination and, in some cases, additional diagnostic tools.”
Histological Variants of CIS
CIS can have different histological variants, like pagetoid spread and large cell CIS. These variants can be confused with other urothelial lesions. Accurate identification of these variants is essential for proper diagnosis and management.
| Histological Feature | CIS | Reactive Urothelial Atypia |
| Nuclear Pleomorphism | Significant | Mild to Moderate |
| Architectural Pattern | Disordered | More Orderly |
| CK20 Staining | Full-thickness | Variable, often limited to umbrella cells |
In conclusion, the histomorphological features of CIS are critical for its diagnosis. Understanding the cellular architecture, organizational patterns, and histological variants, as well as distinguishing CIS from reactive conditions, are essential for accurate diagnosis and effective management.
Key Insight #2: Primary vs. Secondary Urothelial Carcinoma In Situ
It’s important to know the difference between primary and secondary urothelial carcinoma in situ. This knowledge helps doctors diagnose and treat bladder cancer better. Urothelial carcinoma in situ (CIS) is divided into two types based on its connection to other bladder cancers.
Primary CIS: Diagnostic Criteria and Clinical Presentation
Primary CIS is found when there’s no history of bladder cancer. Doctors look for cancer cells in the bladder lining without invasion. Patients might have symptoms like painful urination, frequent need to urinate, or blood in the urine, but some don’t show any symptoms.
Doctors use a microscope to check for cancer cells. They look for big nuclei, prominent nucleoli, and loss of cell shape. Getting the diagnosis right is key to start the right treatment and stop the cancer from getting worse.
Secondary CIS: Association with Invasive and Non-invasive Urothelial Neoplasms
Secondary CIS happens when there’s a history of bladder cancer, either invasive or non-invasive. It’s often found when checking on patients with bladder cancer history or when new symptoms appear in those with known bladder issues.
Finding secondary CIS means the cancer might be coming back or getting worse. The symptoms can vary based on the type of cancer and how much CIS is present.
In short, knowing the difference between primary and secondary CIS is vital. It helps doctors create better treatment plans and improve patient care for urothelial carcinoma in situ.
Key Insight #3: Immunohistochemical Profile in Diagnosis
In diagnosing CIS, immunohistochemical profiling is key. It uses specific markers to tell CIS apart from other urothelial lesions.
CK20 Full Thickness Staining Pattern
CK20 is a critical marker for CIS. In CIS, CK20 stains the whole urothelial layer. This is different from normal urothelium or reactive atypia, where CK20 only stains the top layer.
p53 Expression Patterns and Significance
p53 is another important marker. In CIS, p53 often shows overexpression or is completely absent. These patterns suggest TP53 gene mutations, which are common in CIS and increase its risk of becoming cancerous.
CD44 Expression Loss as Diagnostic Marker
CD44 is a protein found in the basal and intermediate layers of the urothelium. In CIS, CD44 is often lost. This loss, along with other markers, helps doctors tell CIS apart from other conditions.
These markers together create a strong profile for diagnosing CIS. Here’s a table that shows what to look for in CIS:
| Marker | Typical Expression Pattern in CIS | Diagnostic Significance |
| CK20 | Full-thickness staining | Distinguishes CIS from normal/reactive urothelium |
| p53 | Overexpression or null phenotype | Indicates TP53 gene mutations, contributing to malignancy |
| CD44 | Loss of expression | Aids in distinguishing CIS from reactive/dysplastic conditions |
Using these markers improves CIS diagnosis accuracy. It also helps us understand CIS’s pathology better.
Diagnostic Challenges and Pitfalls in Urothelial Carcinoma In Situ
Diagnosing CIS is hard because of several challenges. The subtlety of its features and the quality of the specimen play big roles.
Sampling Adequacy and Specimen Quality Issues
Getting a good sample is key for CIS diagnosis. Inadequate sampling can miss CIS. It’s important to handle specimens with care.
Specimen quality can be affected by crush artifact or inadequate fixation. These problems make it hard for pathologists to diagnose accurately.
Mimics of CIS in Urinary Bladder
Some conditions can look like CIS in the bladder, making diagnosis tough. Reactive atypia and urothelial dysplasia are examples.
To tell CIS apart from these mimics, pathologists need to look closely at the tissue. Sometimes, immunohistochemical stains help too.
Interpretative Challenges in Difficult Cases
Even with good samples, some cases are hard to interpret. CIS can be tricky to diagnose, thanks to variant histology or atypical features.
In these tough cases, getting a second opinion or using more tools might be needed. This helps ensure a correct diagnosis.
Key Insight #4: Molecular Pathology of Urothelial Carcinoma In Situ
The molecular makeup of CIS shows unique genetic and chromosomal changes. These changes set it apart from other urothelial tumors. Recent studies have uncovered a complex mix of genetic and chromosomal changes that help CIS grow and progress.
Genetic Alterations and Chromosomal Abnormalities
CIS often has genetic changes like TP53 and PIK3CA mutations. It also has chromosomal issues, such as aneuploidy and loss of heterozygosity. These changes disrupt normal cell function, leading to CIS.
Chromosomal instability is a key feature of CIS. It’s linked to a high risk of turning into invasive cancer. CIS lesions often show a lot of aneuploidy, with certain chromosomes or regions being gained or lost.
Molecular Progression Pathway from CIS to Invasive Carcinoma
The move from CIS to invasive cancer is complex. It involves more genetic changes. CIS lesions often share genetic changes with invasive cancers, showing a close relationship.
The journey from CIS to invasive cancer involves many genetic and epigenetic changes. These changes help tumor cells break through the bladder wall and spread. Knowing this pathway is key to finding better ways to diagnose and treat CIS.
Comparison with Molecular Features of Papillary Urothelial Neoplasms
CIS and papillary urothelial neoplasms have different molecular traits. While papillary neoplasms have distinct genetic changes, CIS has a more complex and varied molecular profile.
| Molecular Feature | CIS | Papillary Urothelial Neoplasms |
| TP53 Mutations | Frequent | Less Frequent |
| Chromosomal Instability | High | Variable |
| Genetic Alterations | Complex and Heterogeneous | Distinct and Relatively Homogeneous |
Knowing the molecular differences between CIS and papillary neoplasms is vital for accurate diagnosis and treatment. The unique molecular profiles of these lesions guide diagnostic and treatment plans. This can lead to better patient outcomes.
Differential Diagnosis in Flat Urothelial Lesions
Distinguishing urothelial CIS from other flat urothelial lesions is key. Accurate identification is vital for the right treatment and care.
Flat urothelial lesions are tricky to diagnose because of their varied looks and meanings. We need to think about different diagnoses to make sure we treat them right.
Reactive Atypia vs. CIS
Reactive atypia is a harmless condition that looks like CIS. It happens when the bladder gets inflamed or injured. We must look closely at the cells to tell them apart.
Both conditions can have big nuclei and prominent nucleoli. But CIS has more nuclear atypia and disorder than reactive atypia.
Urothelial Dysplasia vs. CIS
Urothelial dysplasia is a pre-cancerous condition that might turn into CIS or cancer. It’s hard to tell CIS and dysplasia apart because they both have abnormal cells.
The main difference is in how bad the cell changes are. CIS has more severe nuclear changes and disorganization than dysplasia.
Urothelial Proliferation of Uncertain Malignant Potentia
This condition has more cells than usual but doesn’t show clear signs of cancer. It’s diagnosed when the cell growth is suspicious but not CIS or dysplasia.
We need to keep an eye on these patients. Some might develop CIS or cancer. Regular check-ups are important for catching problems early.
Key Insight #5: Advanced Diagnostic Techniques and Emerging Biomarkers
The field of urothelial carcinoma in situ diagnosis is changing fast. New diagnostic techniques and biomarkers are key to better diagnosis and care for patients.
Fluorescence In Situ Hybridization (FISH) Applications
Fluorescence In Situ Hybridization (FISH) is a big help in finding urothelial carcinoma in situ. It spots genetic changes in urine, helping find CIS even when tests are not clear. FISH is a great tool to add to traditional tests.
Next-Generation Sequencing in CIS Diagnosis
Next-generation sequencing (NGS) is changing pathology. It lets us look at many genes at once for CIS. NGS finds specific mutations in CIS, giving us important info for diagnosis and treatment. It’s very promising for finding new treatments.
Novel Biomarkers for Early Detection and Monitoring
Finding new biomarkers is key for early CIS detection and tracking. Studies have found biomarkers linked to cell cycle, DNA repair, and signaling. Using these biomarkers could lead to better patient care by catching problems early.
As we keep working on new diagnostic tools and biomarkers, the future of CIS diagnosis looks bright. Using these new methods will help us diagnose better, care for patients better, and fight this disease more effectively.
Clinical Correlation and Prognostic Implications
It’s important to understand the clinical correlation and prognostic implications of urothelial carcinoma in situ (CIS). CIS is a high-grade, flat lesion. It is considered a precursor to invasive bladder cancer.
Natural History and Progression Risk of Untreated CIS
CIS has a high risk of progressing to muscle-invasive bladder cancer if not treated. Studies show that many patients with untreated CIS will develop invasive cancer. This makes early detection and treatment very important.
The natural history of CIS is complex. It can stay indolent or progress to invasive cancer. Genetic alterations, the size of the lesion, and the patient’s health play a role in this progression.
Response Patterns to Intravesical Therapy
Intravesical therapy is a common treatment for CIS. It involves putting therapeutic agents directly into the bladder. The response to this therapy varies among patients.
Some patients fully respond, while others see recurrence or persistence of CIS. The type of therapy, treatment duration, and patient characteristics influence these outcomes.
| Therapy Type | Complete Response Rate | Recurrence Rate |
| BCG Therapy | 60-70% | 20-30% |
| Mitomycin C | 50-60% | 30-40% |
Predictive Factors for Treatment Resistance
It’s key to identify predictive factors for treatment resistance. Factors include prior treatment failure, CIS in the prostatic urethra, and certain genetic markers.
Knowing these factors helps tailor treatment strategies. This can improve patient outcomes.
Conclusion: Future Directions in CIS Pathology and Management
Understanding urothelial carcinoma in situ (CIS) is key to managing bladder cancer. CIS bladder is a high-risk lesion that can turn into invasive carcinoma.
New diagnostic and therapeutic strategies are needed for CIS. Molecular pathology and biomarkers could help in early detection and monitoring.
Techniques like next-generation sequencing and fluorescence in situ hybridization (FISH) are improving CIS diagnosis and management. These advancements will lead to more tailored treatments, better patient outcomes.
Research on CIS will help develop more effective treatments and management plans. Our knowledge of CIS is essential in the battle against bladder cancer.
FAQ
What is urothelial carcinoma in situ (CIS) and how is it defined?
Urothelial carcinoma in situ is a flat, non-invasive lesion. It has malignant urothelial cells in the urothelium but doesn’t go through the basement membrane. It’s seen as a step before invasive urothelial carcinoma.
How is CIS distinguished from reactive atypia?
CIS is different from reactive atypia because of more atypia and disorder. It lacks umbrella cells. CK20 and p53 staining help in diagnosis.
What is the significance of primary vs. secondary CIS?
Primary CIS starts on its own. Secondary CIS comes after urothelial neoplasia. Secondary CIS often goes with invasive or non-invasive tumors.
What is the role of immunohistochemistry in the diagnosis of CIS?
Immunohistochemistry, like CK20, p53, and CD44 staining, helps diagnose CIS. It shows the unique protein expressions in CIS.
What are the diagnostic challenges and pitfalls in CIS?
Diagnosing CIS can be tough due to sampling issues and quality. It can look like reactive conditions. Careful look at histology and immunohistochemistry is needed.
What are the molecular alterations associated with CIS?
CIS has genetic changes, like chromosomal issues and mutations in TP53 and FGFR3. These changes help CIS develop and grow.
How is CIS managed clinically?
CIS is treated with intravesical therapy, like BCG or chemotherapy. How well it responds and what makes it resistant are key in treatment.
What is the natural history of untreated CIS?
Untreated CIS has a high chance of turning into invasive cancer. Its natural course is marked by a high risk of tumor growth and spread.
What are the emerging biomarkers for CIS detection and monitoring?
New biomarkers, found through next-generation sequencing, promise better CIS detection and tracking.
How does CIS relate to other flat urothelial lesions?
CIS is different from other flat urothelial lesions like reactive atypia and dysplasia. It’s based on histology and immunohistochemistry.
What is the role of Fluorescence In Situ Hybridization (FISH) in CIS diagnosis?
FISH helps diagnose CIS by finding chromosomal changes typical of urothelial neoplasia.
What is carcinoma in situ (CIS) of the bladder?
CIS of the bladder is when malignant cells are in the urothelium but haven’t invaded the basement membrane. It’s a high-grade lesion with a big risk of progression.
What does “urothelial carcinoma pathology outlines” refer to?
Urothelial carcinoma pathology outlines describe and classify urothelial carcinomas, including CIS. It’s based on histology and molecular features.
What is the urinary bladder is grossly unremarkable?
A urinary bladder that is grossly unremarkable looks normal. There are no obvious abnormalities or lesions.
References
National Center for Biotechnology Information. (2025). 5 Key Pathology Insights on Urothelial Carcinoma In. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19176205/


































