Last Updated on November 4, 2025 by mcelik
Degenerative disc disease affects millions, causing a lot of pain. Knowing what triggers disc pain flare-ups is key to managing it well.
The spine is complex, and when discs wear out, it can cause back pain triggers. So, what makes these flare-ups happen?
Studies show that lifestyle and health issues can start disc pain flare-ups. Knowing these degenerative disc triggers helps people take steps to lessen their pain.
Key Takeaways
- Degenerative disc disease affects the spine, causing discomfort and pain.
- Understanding the causes of flare-ups is key to managing the condition.
- Lifestyle choices and health conditions can trigger disc pain flare-ups.
- Identifying degenerative disc triggers can help mitigate symptoms.
- Managing back pain triggers is important for spinal health.
Understanding Degenerative Disc Disease and Its Flare-ups

As we get older, our spinal discs change naturally. For some, this leads to degenerative disc disease. It’s not a disease but a normal aging process. It can cause pain if it leads to inflammation or nerve compression.
What is Degenerative Disc Disease?
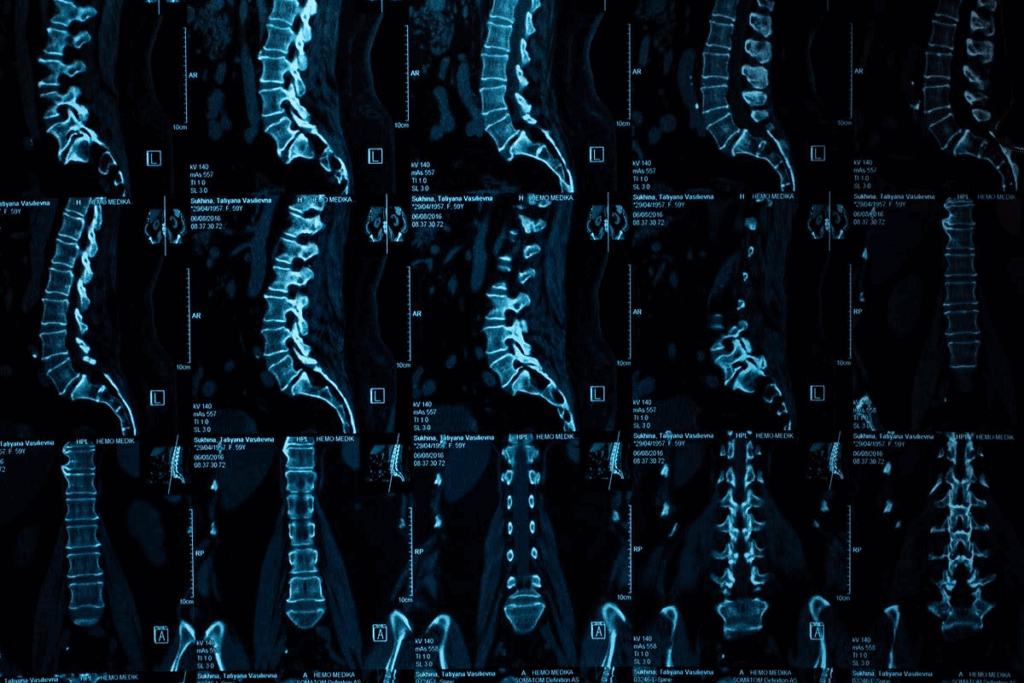
Degenerative disc disease is when the spinal discs wear out. The spinal discs are important for absorbing shock and keeping the spine flexible. With age, these discs can lose their effectiveness, leading to degeneration.
The discs dry out with age, becoming less flexible and more likely to crack or tear. This can cause pain and discomfort. If the degeneration is severe, it can irritate the nerves around it.
How Flare-ups Manifest in Disc Degeneration
Flare-ups happen when the spinal disc degeneration causes a lot of pain. They can be triggered by sudden movements, heavy lifting, or even simple actions like bending or twisting. During a flare-up, the pain can vary from mild to severe. It may also include numbness or tingling in the limbs.
It’s important to understand degenerative disc disease and its flare-ups to manage it well. Knowing the triggers and taking steps to prevent them can help reduce flare-ups.
The Mechanics Behind Disc Pain Flare Ups
It’s important to know how disc pain flare-ups work to manage degenerative disc disease well. We’ll look at the difference between normal and degenerated disc function. We’ll also explain how pain signals start during flare-ups.
Normal Disc Function vs. Degenerated Disc Function
Spinal discs are like shock absorbers between vertebrae, helping with smooth movement and shock absorption. They have a tough outer layer and a soft inner part. As we get older, we lose water and become less flexible, which can cause pain.
This loss of function puts more stress on the spine.
A degenerated disc, on the other hand, has less water and is less flexible. It’s more likely to hurt and cause pain. The discs shrinking can make the vertebrae rub together, leading to inflammation and pain. Many things can speed up this degeneration, like genetics, lifestyle, and past injuries.
How Pain Signals Develop During Flare-ups
Pain during flare-ups usually comes from irritated nerve endings in the disc and around it. When a disc is degenerated, it can bulge or herniate. This presses on nerves, causing pain. The pain can be mild or very severe and often comes with inflammation.
The process of pain signal development is complex. Inflammatory chemicals are released, making nerve endings more sensitive and increasing pain. This chemical process can make us more sensitive to pain during flare-ups.
Understanding these mechanics helps us manage disc pain flare-ups better. It improves life quality for those with degenerative disc disease.
Physical Movements That Trigger Flare-ups
Knowing what movements can make back pain worse is key to managing pain. Some actions can make degenerative disc disease symptoms worse, leading to more pain.
Bending and Twisting Spine Pain
Bending forward and twisting can strain the spine, hurting the discs. When you bend forward, you press on the disc’s front, which can cause it to bulge or herniate. This leads to pain. Twisting adds more stress, irritating nerves and causing twisting spine pain.
To avoid flare-ups, learn how to bend correctly. Bend at the knees, not the waist, to keep your back straight. This reduces pressure on your spine and discs.
Heavy Lifting Back Pain
Lifting heavy things can also trigger back pain. It puts extra stress on your spine and muscles. Bad lifting habits can make heavy lifting back pain worse, hurting your discs.
To lift safely, use your legs, not your back. Keep the object close and don’t twist. If it’s too heavy, get help or use tools.
“Proper lifting techniques can significantly reduce the strain on your back, minimizing the risk of flare-ups.”
Sudden Movements and Jerking Actions
Sudden or jerky movements can also cause flare-ups. These can stress the spine, irritating discs and nerves. Quick changes in direction or speed are often the worst.
Move slowly and deliberately to avoid sudden stress. Do exercises that improve flexibility and strength. This can help stabilize your spine and lower flare-up risks.
Posture-Related Triggers for Disc Pain

The way we sit, stand, and sleep greatly affects our disc health. Posture issues are a common cause of disc pain. Knowing these triggers helps us manage and prevent pain.
Sitting Too Long Spine Problems
Sitting for long periods strains the spine, mainly in the lower back. When we sit, our spine faces more pressure, which can cause pain. This is because our discs get compressed and inflamed.
To avoid this, it’s key to stand and stretch often. Keeping a straight spine while sitting helps too. Make sure your feet are on the floor or on a footrest.
“Sitting for long periods can lead to disc degeneration and pain. Regular movement and proper posture can help alleviate this issue.”
A Spine Specialist
Poor Posture Disc Pain Development
Poor posture, whether sitting or standing, can cause disc pain. When our posture is bad, it puts uneven weight on the spine. This leads to some discs bearing more pressure than others.
To improve posture, strengthen your core and be mindful of your standing and sitting. Avoid slouching. Making ergonomic changes to your workspace and daily habits also helps reduce disc pain from poor posture.
| Posture Type | Effect on Discs | Corrective Action |
| Slouching | Increased pressure on lumbar discs | Strengthen core, ergonomic adjustments |
| Forward Head Posture | Strain on cervical discs | Improve neck posture, take breaks |
Sleeping Positions That Worsen Disc Pain
Sleeping in certain ways can make disc pain worse, like twisting or bending the spine. For example, sleeping on your stomach twists your neck, irritating your cervical discs.
To help with disc pain from sleeping, sleep on your back with a pillow under your knees. Or, sleep on your side with a pillow between your knees. This keeps your spine’s natural curve and reduces disc pressure.
Being mindful of our posture and making small changes in our daily life can greatly reduce disc pain. It also improves our spinal health.
Impact of Physical Activity on Disc Health
Physical activity affects disc health in many ways. It can be good or bad. Exercise keeps the back healthy, but too much can hurt. Not moving enough can also cause problems like stiffness.
Overexertion and Exercise Strain Back Pain
Too much physical activity can strain the back, causing pain. This is common with heavy lifting, bending, or twisting. Such actions stress the spinal discs, making problems worse.
“Exercise is essential, but it must be done correctly to avoid injury,” says the need for proper form and moderation.
Lack of Movement Spine Problems
Sitting too much can harm the spine, including the discs. Without movement, discs lose their cushioning, leading to pain and stiffness.
Moving regularly keeps discs healthy by exchanging nutrients and waste. Without enough movement, discs can become unhealthy, causing pain.
Finding the Right Balance of Activity
Finding the right balance in physical activity is key to disc health. We should avoid too much or too little activity. Walking or swimming is good for keeping the back healthy without straining the discs too much.
Exercises that strengthen the core muscles are also important. A strong core supports the spine, helping to prevent pain and future problems.
Being mindful of our posture, lifting techniques, and overall physical condition is important. A balanced approach to physical activity helps keep the back healthy and reduces pain risk.
Environmental Factors Affecting Disc Pain
The link between environmental factors and disc pain is complex. It involves things like temperature and humidity. Understanding these can help those with degenerative disc disease manage their condition better.
Weather Changes Back Pain Connections
Research shows that weather changes can impact back pain. This might be due to pressure and temperature shifts. Many people notice their back pain gets worse with weather changes.
One idea is that pressure changes make spine discs expand or contract. This can irritate nerves and cause pain. While this idea is being looked into, it’s good for those with degenerative disc disease to watch out for weather-related pain spikes.
Cold Weather Spine Pain Mechanisms
Cold weather often makes spine pain worse. The cold stiffens muscles, which can increase pain for those with degenerative disc disease. Cold weather also might reduce blood flow, adding to pain and stiffness.
To fight cold-weather effects, people can keep warm, use heating pads, or do gentle exercises. This helps keep muscles flexible.
Humidity and Its Influence on Disc Hydration
Humidity affects disc hydration, which is key for healthy discs. Dehydration can cause discs to degenerate and worsen pain. While research is ongoing, staying hydrated is vital for disc health.
Extreme humidity, whether too high or too low, can also affect the spine. So, being aware of your environment and staying hydrated is helpful.
Biological Processes Behind Disc Degeneration Flare-ups
It’s important to know how disc degeneration works to handle flare-ups. This condition is influenced by several factors, like inflammation, dehydration, and aging.
Spine Inflammation Causes
Inflammation in the spine plays a big role in flare-ups. Spine inflammation can be from mechanical stress or autoimmune responses. When the spine is stressed, it can get inflamed, causing pain.
Inflammatory responses can also happen naturally when the body reacts to injury or degeneration. As discs degenerate, they release chemicals that can make inflammation worse, leading to flare-ups.
Disc Dehydration Pain
Disc dehydration is another key factor in pain. As we age, our spinal discs lose water, leading to degeneration and pain. Disc dehydration pain happens when dehydrated discs can’t cushion the spine well, putting stress on joints and muscles.
When discs lose water, they shrink, making the spine unstable. This instability can cause pain, mainly during activities that stress the spine.
Aging Disc Flare Ups
Aging disc flare-ups are common as discs naturally degenerate with age. As we get older, discs lose water and flexibility, making them more prone to injury and degeneration.
| Biological Change | Effect on Discs | Potential Outcome |
| Loss of Hydration | Reduced disc height and cushioning | Increased stress on spinal joints |
| Inflammation | Release of pro-inflammatory chemicals | Pain and discomfort |
| Aging | Loss of disc elasticity and hydration | Increased susceptibility to injury |
Knowing these biological processes helps us manage flare-ups better. It improves life quality for those dealing with disc degeneration.
Stress and Emotional Factors in Disc Pain
Disc pain is often linked to stress and emotions. The mind and body are closely connected, affecting how we feel pain.
Stress Back Flare Ups
Stress can make back pain worse. When stressed, our body’s “fight or flight” response kicks in. This causes muscle tension, which strains the spine and discs, leading to pain.
Mechanisms Behind Stress-Induced Flare-Ups:
- Muscle tension due to stress
- Increased inflammation
- Altered pain perception
Stress Hormones Spine Impact
Stress hormones like cortisol affect the body’s stress response. High levels of cortisol can harm the spine, including the discs.
“Chronic stress can lead to an overproduction of cortisol, which can affect the health of spinal discs.”
| Stress Hormone | Effect on Spine |
| Cortisol | Disc Degeneration |
| Adrenaline | Muscle Tension |
Emotional Well-being and Pain Perception
Our emotional state affects how we feel pain. People with anxiety or depression might feel pain more easily.
Managing emotional well-being through techniques such as mindfulness and cognitive-behavioral therapy can help in mitigating pain perception.
Understanding stress and emotional factors in disc pain helps us manage it better. We can tackle both physical and mental aspects of the condition.
Weight and Body Composition Influences
Our body weight greatly affects our spinal discs’ health. Too much weight, mainly around the belly, puts extra pressure on the lower back. This can cause discomfort and pain.
Weight Gain and Back Pain Connections
When we gain weight, our spine works harder to support it. This extra effort wears down the spinal discs faster. It can make conditions like degenerative disc disease worse.
Mechanisms Behind Weight-Related Back Pain:
- Increased pressure on the spinal discs
- Inflammation due to excess body fat
- Altered biomechanics and posture
Abdominal Fat and Its Effect on the Lumbar Spine
Visceral fat in the belly can cause chronic inflammation. This affects the lower back. This type of fat is active and can irritate the spinal tissues.
Weight Management for Disc Health
Keeping a healthy weight helps with back pain from degenerative disc disease. A healthy weight reduces spine pressure. This slows down the degeneration process.
| Weight Management Strategies | Benefits for Disc Health |
| Balanced Diet | Reduces inflammation and supports overall health |
| Regular Exercise | Strengthens back muscles and improves flexibility |
| Healthy Lifestyle Choices | Enhances overall well-being and reduces back pain |
Understanding how weight affects our spinal health is key. By making healthy lifestyle choices, we can manage and prevent back pain from degenerative disc disease.
Ergonomic Factors in Daily Activities
Improving our daily routines can help with disc pain. Ergonomics is about designing our spaces to reduce body strain, focusing on the spine.
Bad Ergonomics Disc Pain
Poor ergonomics can cause disc pain. A workspace that doesn’t support good posture can lead to discomfort. For example, a monitor that’s too low or a chair that’s too high can strain our discs.
To fix this, we need to set up our workspace for good posture. This means having our monitor at eye level, keeping our keyboard and mouse close, and using a supportive chair.
Driving and Transportation Stressors
Driving can also hurt our spines. Long drives in cars without good lumbar support can make disc pain worse. The constant movement can irritate our discs.
To lessen the impact of driving, we should take breaks to stretch and move. Adjusting the car seat for better lumbar support and using a cushion can also help.
Home Environment Considerations
Our home environment affects our spine, too. From furniture to household chores, there are many ways to help or hurt our discs.
For instance, using a supportive mattress and maintaining good posture while doing chores can reduce strain. We should also think about the height and design of our work surfaces and storage to avoid bending or stretching.
| Ergonomic Adjustment | Benefit |
| Monitor at eye level | Reduces neck strain |
| Lumbar support while driving | Decreases lower back pain |
| Supportive mattress | Improves sleep quality and reduces disc pain |
By making these ergonomic changes, we can lessen the strain on our spine and reduce disc pain. It’s about creating a supportive environment for our spinal health.
Specific Conditions That Exacerbate Disc Pain
Some spinal conditions can make disc pain worse, affecting our daily lives. Knowing about these conditions helps us manage and treat them better.
Disc Bulge Flare Ups
A disc bulge happens when the disc’s outer layer weakens. This lets the soft inner gel bulge out, irritating nerves and causing pain. Disc bulge flare-ups often come from sudden movements or heavy lifting.
Symptoms include pain, numbness, or tingling in the arms or legs. This depends on where the bulge is.
Sciatica Flare Triggers
Sciatica is pain that spreads along the sciatic nerve from the lower back to the legs. Sciatica flare triggers include sitting for too long, heavy lifting, or sudden twists.
To manage sciatica, avoid these triggers. Also, do exercises that strengthen the back and improve flexibility.
Spinal Instability Flare Mechanisms
Spinal instability happens when the spine can’t stay in its normal position. This is often due to loose ligaments or degenerating discs. It can cause pain flare-ups, mainly after long activities or at night.
| Condition | Common Triggers | Symptoms |
| Disc Bulge | Sudden movements, heavy lifting | Localized pain, numbness, tingling |
| Sciatica | Prolonged sitting, heavy lifting, and twisting | Radiating pain down the leg |
| Spinal Instability | Prolonged activity, poor posture | Pain flare-ups, especially after activity |
Understanding these conditions and their triggers helps us manage disc pain. It also improves our spinal health.
Core Strength and Muscle Support
A strong core is key to a healthy spine and avoiding flare-ups from degenerative disc disease. Our core and back muscles support the spine. Their strength is vital in managing the condition.
The Impact of Weak Core Muscles on Spine Health
Weak core muscles can cause spine instability, raising the risk of flare-ups. Without strong core muscles, the spine takes more stress. This can lead to disc degeneration and pain. Strengthening these muscles is essential for spinal stability.
The Role of Back Muscles in Supporting the Spine
The back muscles work with the core to support the spine. They help keep posture right, move smoothly, and absorb shock. A well-conditioned back can significantly reduce the strain on the spinal discs.
“The strength of your back and core muscles is directly related to the health of your spine. By strengthening these muscles, you can reduce the risk of flare-ups and improve your overall spinal health.”
Building Proper Support for Disc Health
To support disc health, it’s important to do exercises that strengthen the core and back. This includes:
- Planks and other core-strengthening exercises
- Pelvic tilts to improve flexibility and strength
- Latissimus dorsi exercises to strengthen the back
Being consistent with exercise is important. Regular physical activity can greatly improve spinal health.
| Exercise | Benefit | Frequency |
| Plank | Core Strengthening | 3 times a week |
| Pelvic Tilt | Flexibility and Strength | Daily |
| Lat Pulldown | Back Strengthening | 3 times a week |
By focusing on a strong core and back, people can greatly improve their spinal health. This can also reduce flare-ups from degenerative disc disease.
Recognizing Early Warning Signs of Flare-ups
It’s important to know the early signs of flare-ups to manage degenerative disc disease well. By spotting these signs early, people can lessen the impact of flare-ups. This helps improve their overall quality of life.
Prodromal Symptoms Before Major Flare-ups
Prodromal symptoms are early signs that may happen before a big flare-up. These can be slight changes in pain, stiffness, or discomfort in the back. Recognizing these symptoms early helps take action to stop pain from getting worse.
Some common prodromal symptoms include:
- Increased stiffness in the morning
- Mild pain that gradually worsens
- Sensitivity to certain movements
Tracking Patterns in Your Disc Pain
Tracking your disc pain patterns is key to understanding what triggers flare-ups. Keeping a pain journal helps find links between activities, environment, and pain episodes.
| Activity | Duration | Pain Level (1-10) |
| Heavy Lifting | 30 minutes | 6 |
| Prolonged Sitting | 2 hours | 4 |
| Bending and Twisting | 1 hour | 7 |
When to Seek Medical Attention
Knowing when to get medical help is key to managing flare-ups. If pain is severe, lasts a long time, or comes with numbness or weakness, seek help right away.
Red flags that require immediate medical attention include:
- Sudden onset of severe pain
- Loss of bladder or bowel control
- Progressive numbness or weakness
Being alert to early signs and knowing when to get help can help manage degenerative disc disease. This reduces the impact of flare-ups on daily life.
Conclusion: Managing and Preventing Disc Pain Flare-ups
Understanding what causes flare-ups helps us manage degenerative disc disease better. We’ve looked at many factors, like how we move, our posture, and even our environment. We’ve also talked about how our bodies work.
Managing disc pain needs a few steps. We should balance activity and rest, keep good posture, and handle stress well. This helps lower the chance of flare-ups and makes pain easier to handle.
To stop flare-ups, we need to act early. Keeping a healthy weight, exercising regularly, and strengthening our core are key. These habits help our spine stay healthy and reduce flare-up risks.
Dealing with disc pain is a long-term effort. It takes patience, commitment, and the right advice. Working with doctors and using a full plan for managing pain can greatly improve our lives.
FAQ
What is degenerative disc disease and how does it cause flare-ups?
Degenerative disc disease happens when spinal discs lose their moisture and flexibility. This leads to pain and swelling. Flare-ups occur when the affected disc is stressed, causing pain signals.
How do physical movements trigger flare-ups in degenerative disc disease?
Actions like bending, twisting, heavy lifting, and sudden movements can cause flare-ups. They put extra stress on the degenerated disc, causing pain and swelling.
Can poor posture contribute to disc pain flare-ups?
Yes, poor posture can lead to disc pain flare-ups. It puts extra stress on the spinal discs, mainly when sitting or standing for long times.
How does physical activity impact disc health?
Physical activity can both help and harm disc health. Regular exercise keeps discs healthy, but too much can strain and cause pain. Finding the right balance is key.
Can environmental factors such as weather changes affect disc pain?
Yes, weather changes, cold weather, and humidity can affect disc pain. They can change disc hydration and swelling.
How does stress contribute to disc pain flare-ups?
Stress can make disc pain worse by releasing hormones that increase pain and swelling.
Can weight gain and body composition influence disc health?
Yes, weight gain and body composition can affect disc health. Excess abdominal fat can stress the lumbar spine.
How can ergonomic factors contribute to disc pain?
Poor workspace setup, driving, and home environment can cause disc pain. They put extra stress on the spinal discs.
What specific conditions can exacerbate disc pain?
Conditions like disc bulge, sciatica, and spinal instability can worsen disc pain. They put extra stress on the spinal discs and nerves.
How can core strength and muscle support help alleviate disc pain?
Core strength and muscle support can ease disc pain. They provide extra support to the spine and reduce stress on the discs.
What are the early warning signs of flare-ups, and when should I seek medical attention?
Early signs of flare-ups include increased pain or stiffness. If you have severe or ongoing pain, seek medical help to avoid further issues.
How can I manage and prevent disc pain flare-ups?
To manage and prevent flare-ups, maintain a healthy weight, improve posture, and exercise regularly. Avoid overexertion and make ergonomic changes to daily activities.
References
- Singh, S., et al. (2021). Intervertebral Disc Degeneration: The Role and Evidence of Catabolic and Anabolic Imbalance. Journal of Orthopaedic Research, 39(5), 919-929. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8092937/
- Spine-Health. (2017). Causes of Degenerative Disc Disease Pain. https://www.spine-health.com/conditions/degenerative-disc-disease/causes-degenerative-disc-disease-pain
- Fakhoury, J. (2025). Cervical Degenerative Disc Disease. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK560772/