Last Updated on December 1, 2025 by Bilal Hasdemir
The liver is key to our health, doing over 500 jobs. It cleans our body, makes proteins, and helps with digestion. It’s a vital part of our bodily functions, and without it, we face serious health problems. Is living without a liver possible? Get the crucial facts on this powerful organ and the amazing transplant process.
Even though we can’t live without a liver forever, doctors have found ways to help. We’ll look into liver health and what happens if the liver fails or is removed.
Key Takeaways
- The liver plays a vital role in maintaining overall health.
- Liver failure can lead to severe health complications.
- Medical advancements have improved the management of liver-related health issues.
- Liver health is critical for our overall well-being.
- Understanding liver function is essential for maintaining good health.
The Essential Role of the Liver in Human Survival
The liver is key to our survival, doing many important jobs. It cleans the blood, makes proteins, and helps digest fats by making bile.
Key Functions of the Liver
The liver does a lot for us. It detoxifies bad stuff, synthesizes proteins for blood clotting, and produces bile for fat digestion. It also stores glycogen, controls hormone levels, and breaks down medicines.
| Liver Function | Description |
| Detoxification | Removing harmful substances from the blood |
| Protein Synthesis | Producing proteins for blood clotting and other processes |
| Bile Production | Aiding in fat digestion and absorption |
Why the Liver Is Considered a Vital Organ
The liver is vital because it’s essential for life. Without it, we can’t clean our blood, digest food, or make proteins. Liver problems can cause serious health issues, showing how important it is.
Keeping the liver healthy is key to avoiding liver disease. It helps the liver do its job well.
Understanding Liver Anatomy and Physiology
The liver is a vital organ in our bodies. It plays a key role in keeping us healthy. Knowing about its structure and functions helps us see its importance.
Structure and Location of the Liver
The liver sits in the upper right part of our belly. It’s hidden by our rib cage. It has four lobes: right, left, caudate, and quadrate.
The liver’s blood system is complex. It has the hepatic artery and portal vein. These bring it oxygen and nutrients.
The liver is made up of tiny units called lobules. These are hexagonal and full of hepatocytes. Hepatocytes do the liver’s main work, like detoxifying and making proteins.
| Liver Structure | Function |
| Hepatic Artery | Supplies oxygenated blood |
| Portal Vein | Supplies nutrients from the digestive tract |
| Liver Lobules | Site of metabolic functions, including detoxification and protein synthesis |
How the Liver Interacts with Other Body Systems
The liver works closely with the digestive and circulatory systems. It breaks down nutrients and makes bile for fat digestion. It also helps control blood sugar and fats.
The liver filters blood from the digestive system. It removes toxins and waste. This shows how important it is for our health.
Living without a Liver: The Medical Reality
Living without a liver is a complex medical scenario. It raises questions about survival and quality of life. The liver is key for detoxification, metabolism, and making vital proteins.
When we think about living without a liver, we must look at the medical reality. We need to understand the implications of liver removal or failure.
Can Humans Survive Complete Liver Removal?
Humans cannot survive without liver function. The liver is vital for removing toxins, regulating metabolism, and making proteins for blood clotting. Liver transplantation is the only option for patients with end-stage liver disease.
Without a functioning liver, the body builds up toxins. This leads to severe health problems and eventually death.
Liver failure is a life-threatening condition that requires immediate medical attention.
Time Constraints Without Liver Function
The time a person can survive without liver function varies. It depends on the cause of liver failure and any medical treatments. In acute liver failure, the outlook is usually poor without immediate transplant.
| Condition | Survival Time Without Liver Function |
| Acute Liver Failure | Few days to a week |
| Chronic Liver Disease | Weeks to months |
| Supportive Care (e.g., dialysis) | Can extend survival temporarily |
In conclusion, liver transplantation gives many patients a second chance at life. But, living without a liver is very challenging. Understanding the liver’s role and the consequences of failure is key. It helps us appreciate the complexities of liver disease and the need for medical interventions.
Liver Failure: Causes and Consequences
Liver failure happens when the liver can’t work anymore. This can happen quickly or slowly. It’s very serious and needs quick medical help. The liver is key for cleaning the body, breaking down food, and making important proteins.
Acute vs. Chronic Liver Failure
Liver failure is divided into acute and chronic types. Acute liver failure is when the liver stops working suddenly in someone without liver problems before. It’s often caused by viruses, too much medicine, or toxins.
Chronic liver failure is when the liver gets damaged over time. This can be due to cirrhosis, hepatitis, or metabolic problems like MASLD.
Recent studies show MASLD is a term for liver issues with too much fat in the liver. This can lead to worse liver diseases like steatohepatitis, fibrosis, and cirrhosis.
Immediate Health Impacts of Liver Failure
The effects of liver failure are serious and happen right away. They include jaundice, which makes the skin and eyes turn yellow. Coagulopathy makes it hard for blood to clot, raising the risk of bleeding. Hepatic encephalopathy causes brain problems, from confusion to coma.
| Condition | Description | Common Causes |
| Acute Liver Failure | Rapid loss of liver function | Viral infections, drug overdoses, toxins |
| Chronic Liver Failure | Long-term liver damage | Cirrhosis, hepatitis, MASLD |
Knowing about liver failure’s causes and effects is key for getting help fast. Both acute and chronic liver failures have big health effects. This shows why it’s important to keep the liver healthy and treat liver diseases quickly.
Recognizing Liver Disease Symptoms
Liver disease often starts quietly, making it key to spot its signs early. The liver is tough, but stress or damage can show symptoms. These should not be ignored.
Early Warning Signs of Liver Problems
Spotting liver disease early can greatly help treatment. Some early signs include:
- Fatigue: Feeling very tired or weak without a clear reason.
- Jaundice: Yellow skin and eyes from too much bilirubin.
- Abdominal Swelling: Swelling in the belly, often from fluid.
- Nausea and Loss of Appetite: Feeling sick or eating less.
When to Seek Medical Attention
If you or someone you know has these symptoms, get medical help fast:
- Severe Abdominal Pain: Pain that lasts and is very bad.
- Vomiting Blood: Vomiting blood or dark, tarry stools.
- Confusion or Difficulty Concentrating: Signs of a brain problem from liver disease.
Seeing these symptoms early and talking to a doctor can greatly help manage liver disease.
Liver Transplantation: A Life-Saving Procedure
Liver transplantation is a complex medical procedure that gives a second chance at life. It involves replacing a diseased liver with a healthy one from a donor. We will guide you through the transplantation process and discuss the success rates and survival statistics associated with this procedure.
The Transplantation Process
The process of liver transplantation is complex. It starts with a thorough evaluation to see if the patient is a good candidate. This includes checking the severity of their liver disease and their overall health.
Once the patient is deemed suitable, they are put on a waiting list for a donor liver. The waiting time can vary a lot. It depends on the availability of a matching donor liver and the patient’s medical urgency.
Surgery is the next critical step. It involves removing the diseased liver and putting in the donor liver. This is a very detailed procedure that needs a skilled surgical team.
After the surgery, post-transplant care is very important. It includes managing immunosuppression to prevent rejection and monitoring for any complications.
Success Rates and Survival Statistics
Liver transplantation has become more successful over the years. Advances in surgical techniques, immunosuppressive medications, and post-transplant care have helped. Survival rates have improved a lot, with many patients living for decades after their transplant.
According to studies, the one-year survival rate after liver transplantation is over 90%. Five-year survival rates range between 70% to 80%. These statistics show how effective liver transplantation is for treating end-stage liver disease.
Understanding these success rates and the factors that influence them can help patients and their families make informed decisions. We continue to monitor and report on the latest developments in liver transplantation to provide the most current information available.
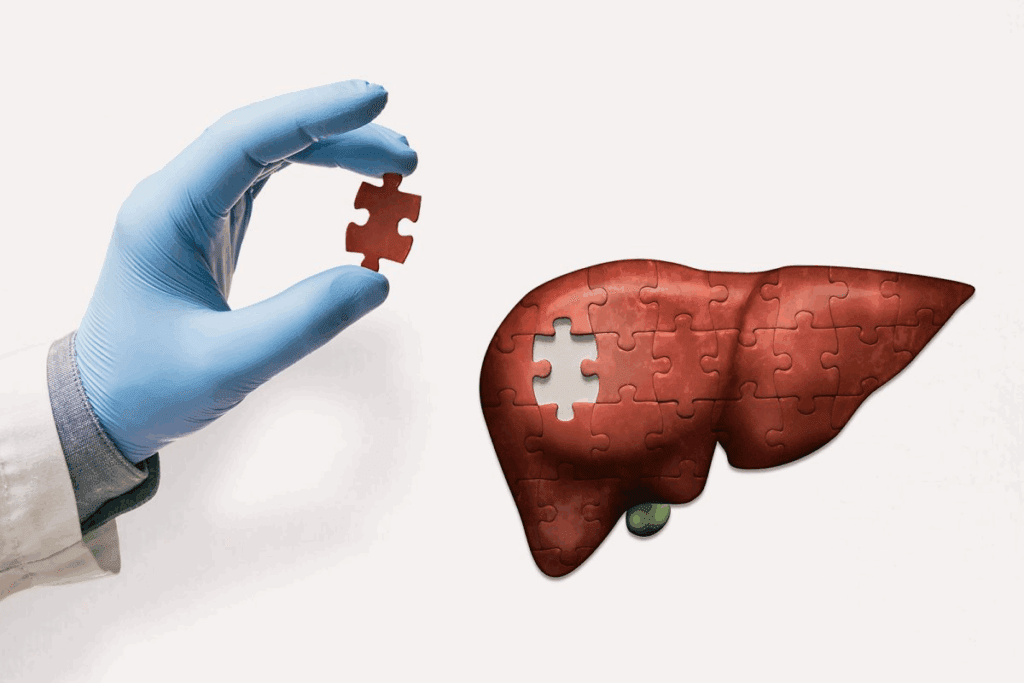
Living with a Partial Liver
Living with a partial liver is possible thanks to the liver’s amazing ability to heal itself. The liver is key for our survival, helping with detox, making proteins, and aiding digestion. If part of the liver gets damaged or removed, the rest can grow back, restoring its full function.
Liver Regeneration Capabilities
The liver can heal itself in a unique way. It grows new liver cells and gets back to full size and function. Liver regeneration depends on how much damage there is and the person’s overall health. Sometimes, the liver can fully recover in just a few weeks.
Research shows the liver can heal even when a big part is damaged or taken out. It can adjust and make up for lost tissue. The regenerative capacity of the liver is vital for those recovering from liver surgery or damage.
Minimum Liver Mass Required for Survival
The amount of liver needed to survive varies by person and liver health. Usually, about 25% of the liver’s original size is enough, if the remaining liver is healthy. But, the exact amount needed can differ greatly from one person to another.
If a lot of liver is lost or damaged, the remaining liver must be able to meet the body’s needs. This includes keeping liver function and liver health in check. The liver’s ability to regenerate and adapt is key for those living with a partial liver.
Living-Donor Liver Transplants: A Modern Medical Marvel
Medical technology has made living-donor liver transplants a real option for saving lives. This method takes a part of a healthy liver from a donor and puts it in someone whose liver isn’t working right.
The Process of Living-Donor Liver Transplants
Getting a living-donor liver transplant is a detailed process. First, doctors check if the donor and recipient are a good match. They look at the donor’s liver to make sure it’s the right size for the recipient.
The surgery takes a part of the donor’s liver and puts it in the recipient. The liver can grow back, helping both the donor and the recipient to heal.
Risks and Recovery for Donors
Donors face risks with living-donor liver transplants. They might get infections, bleed, or have bad reactions to anesthesia.
Donors need a few weeks to recover. They are watched closely for any problems. Most donors can get back to normal in a few months.
| Aspect | Donor | Recipient |
| Surgical Risks | Infection, bleeding | Rejection, infection |
| Recovery Time | Several weeks | Several months |
| Long-term Outcomes | Generally good | Improved survival |
Living-donor liver transplants are a big step forward in treating liver disease. They give hope to patients who had few options before.
Artificial Liver Support Systems
Patients with liver failure often face a critical shortage of donor livers. This makes artificial liver support systems very important. These systems help patients waiting for a liver transplant by providing temporary support.
Current Technologies and Their Limitations
Artificial liver support systems use different methods. Some use living cells, while others are purely mechanical. Despite their promise, these systems have big challenges. For example, bioartificial livers struggle with finding and growing cells, while mechanical devices can’t fully replace a human liver.
A study compared these systems and found their differences:
| Technology | Functionality | Limitations |
| Bioartificial Liver | Uses living cells to perform liver functions | Cell sourcing, scalability issues |
| Mechanical Liver Support | Performs specific liver functions mechanically | Limited functionality compared to human liver |
Future Developments in Artificial Liver Technology
Future advancements aim to fix current problems. Researchers are looking into new materials and cell sources for bioartificial livers. Also, biotechnology and engineering are being improved to make mechanical systems better.
The future of artificial liver support lies in the integration of biotechnology and engineering to create systems that can more closely mimic the human liver’s functions. As these technologies get better, patients waiting for liver transplants will see better results. Developing more advanced artificial liver support systems is key to saving lives of those with liver failure.
Life After Liver Transplantation
Getting a new liver is a big change, giving you a second chance at life. But, it needs a detailed care plan after the transplant. The recovery path is complex, covering the immediate post-surgery and long-term care to keep the new liver healthy.
Post-Transplant Care and Medication
Right after the transplant, patients stay in the ICU to watch for any issues or rejection. Immunosuppressive medications are key to stop the body from rejecting the liver. It’s important to take these meds as told and get regular blood tests to check their levels.
Managing side effects of these meds, like being more prone to infections, is part of post-transplant care. A team of doctors, including liver specialists and transplant surgeons, helps a lot in dealing with these challenges.
| Medication Type | Purpose | Common Side Effects |
| Immunosuppressants | Prevent liver rejection | Increased infection risk, kidney damage |
| Antiviral medications | Prevent viral infections | Nausea, fatigue |
Long-term Lifestyle Adjustments
For long-term success after a liver transplant, big lifestyle changes are needed. Eating well and exercising regularly help keep the new liver working right. It’s also important to avoid alcohol and certain meds that can hurt the liver.
Going to regular check-ups with the transplant team is key to keep an eye on the liver’s health. Staying current with vaccinations and health checks also helps prevent problems.
By following these steps and being proactive about health, people who got a liver transplant can live better and healthier lives.
Preventing Liver Disease and Maintaining Liver Health
A healthy liver is key for detoxifying and processing nutrients. Keeping our liver healthy is vital for our overall well-being. There are many ways to protect our liver.
Dietary Recommendations for Liver Health
Eating lots of fruits, vegetables, and whole grains is good for the liver. We should also cut down on processed foods and sugars, as they can stress the liver. Drinking plenty of water is also important for liver function.
Recent studies show that keeping a healthy weight is essential. Too much body fat can damage the liver. Eating right and staying active can help us keep a healthy weight and support our liver.
Lifestyle Choices That Protect Your Liver
Our lifestyle choices also affect our liver health. Not drinking too much alcohol is very important, as it’s a big risk for liver disease. Also, avoiding toxins and chemicals at home or work helps protect the liver.
Regular health checks and screenings can catch liver problems early. By making smart choices about our lifestyle and diet, we can lower the risk of liver disease. This helps keep our liver working well.
Common Misconceptions About Liver Function and Health
Many myths surround liver function, and it’s time to set the record straight. The liver is a vital organ that performs many functions. It detoxifies the body and helps make proteins. Yet, many misconceptions about its health and function are common.
Debunking Liver Cleanse Myths
Liver cleanses have become popular, but do they really work? They often involve dietary changes or supplements to remove toxins. But, do these methods really work?
Research shows the liver can detoxify itself without special diets or supplements. In fact, some liver cleanse products can harm more than help.
Understanding Actual Liver Detoxification
The liver’s detoxification process is complex and highly efficient. It converts toxins into water-soluble compounds that are then excreted. This process happens all the time, and the liver is very good at it.
| Liver Detoxification Phase | Process | Outcome |
| Phase 1 | Toxins are converted into intermediate compounds | Toxins become more water-soluble |
| Phase 2 | Intermediate compounds are conjugated with other molecules | Toxins become fully water-soluble and are excreted |
Understanding how the liver naturally detoxifies the body helps us appreciate its amazing abilities. It also helps us debunk myths about liver health.
Advances in Liver Disease Treatment Beyond Transplantation
Medical research has made big strides in treating liver disease, moving beyond traditional transplant methods. We’re seeing a big change in how liver disease is managed. Now, there’s a focus on treatments that can reverse or stop disease progress.
Medications and Therapies for Liver Conditions
New medicines and therapies are being developed for liver diseases. For example, treatments for metabolic dysfunction-associated steatotic liver disease (MASLD) are being looked into. Researchers are studying drugs that target liver inflammation and fibrosis.
Current Treatment Approaches:
| Treatment | Description | Target Condition |
| Antiviral Medications | Drugs that directly target viral replication | Hepatitis C |
| Anti-inflammatory Agents | Medications that reduce liver inflammation | NASH, MASLD |
| Lifestyle Interventions | Dietary changes and exercise programs | Fatty Liver Disease |
Emerging Research and Clinical Trials
New research and clinical trials are key to better liver disease treatments. Studies are testing new drugs and strategies, giving hope for better patient outcomes. For instance, stem cell and gene editing research show promise for future treatments.
Exploring new ways to treat liver disease is essential. A mix of old and new treatments will improve patient care. We’re dedicated to advancing liver care through ongoing research and innovation.
Conclusion: The Irreplaceable Nature of the Liver
The liver is key to human survival, playing a vital role in health. It’s responsible for detoxification, metabolism, and making vital proteins. Without a liver, life is not possible.
Keeping the liver healthy is a must. Knowing the risks of liver disease helps us prevent it. Thanks to medical progress, treatments like liver transplants are available. But, we must always value liver function.
We’ve looked at liver health from many angles. This includes liver failure and the latest treatments. By focusing on liver health and living well, we can lower liver disease risks. Medical research and technology will keep improving, making liver disease treatment better. This shows how important liver health initiatives are.
FAQ
Can you survive without a liver?
No, you can’t survive without a liver. The liver can grow back, but losing it completely is deadly without a transplant.
How long can you live without a liver function?
How long you can live without a liver depends on many things. Generally, liver failure can be fatal in days or weeks without treatment.
What are the symptoms of liver disease?
Liver disease symptoms include jaundice, fatigue, and swelling. Dark urine is another sign. Seeing a doctor is key if you notice these.
Can a liver transplant cure liver disease?
A liver transplant can save lives and cure some diseases. But, success depends on the disease and your health.
How does the liver regenerate?
The liver can grow back if damaged. This means it can fix itself if part of it is lost.
What is the minimum liver mass required for survival?
The needed liver size varies by person. Usually, 20-30% of the liver is enough for it to grow back.
What are the risks associated with living-donor liver transplants?
Living-donor transplants have risks for both the giver and the receiver. Donors might face bleeding, infection, or bile duct issues. Recipients could face rejection or other problems.
Can artificial liver support systems replace a transplant?
Artificial systems can help patients waiting for a transplant. But, they can’t replace a transplant for long-term care.
What lifestyle changes are necessary after a liver transplant?
After a transplant, you must follow a strict medicine schedule. You’ll also need to change your diet and lifestyle to stay healthy.
How can I protect my liver health?
Eating well, avoiding too much alcohol, and managing health issues can protect your liver. Regular doctor visits can also catch problems early.
Are liver cleanses effective?
Liver cleanses don’t have scientific backing. The liver naturally cleanses itself. Relying on unproven cleanses can be risky.
What are the latest advances in liver disease treatment?
New treatments for liver disease are being researched. This includes medicines, therapies, and new technologies. Keeping up with these advances can help in making care choices.
References:
- Michalopoulos, G. K. (2023). Physiology, Liver. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK535438