Last Updated on December 1, 2025 by Bilal Hasdemir

Hepatoblastoma is a rare liver cancer that mainly hits kids. It makes people wonder if it’s caused by genes. New studies have found some biomarkers that might predict liver diseases. This has made people curious about the genetic links to hepatoblastoma.
We look into how hepatoblastoma and genes are connected. We dive into the details of this condition and its ties to hepatoma. Knowing the causes and risks helps us support those with this disease.
Key Takeaways
- Hepatoblastoma is a rare form of liver cancer mainly found in children.
- Research into biomarkers has shown possible genetic ties to hepatoblastoma.
- Understanding the hereditary side of hepatoblastoma helps support families affected.
- Hepatoma, a liver tumor, is closely related to hepatoblastoma in liver health.
- More research is needed to fully grasp the genetic factors behind hepatoblastoma.
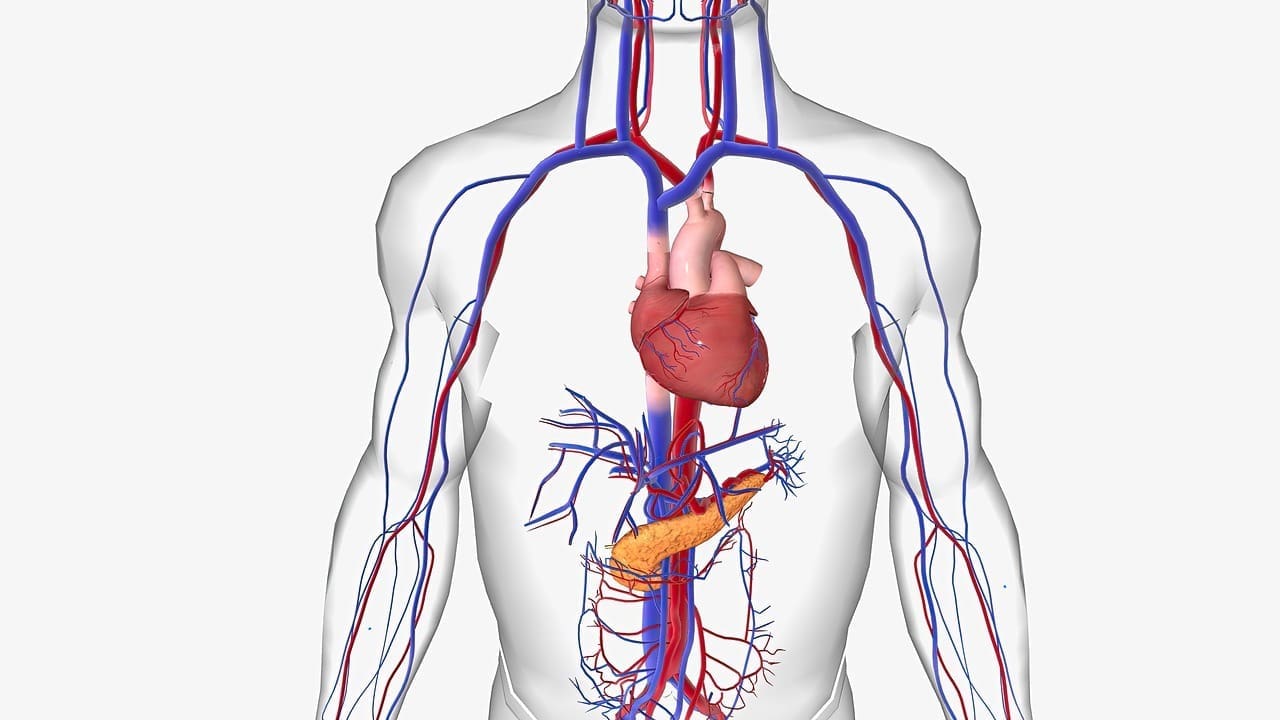
Understanding Liver Cancer: Types and Classifications
Liver cancer includes many types of tumors that start in the liver. Each type has its own features. They are grouped by where they start, when they appear, and how they look under a microscope.
Primary vs. Secondary Liver Cancers
Liver cancers are mainly split into two types: primary and secondary. Primary liver cancer starts in the liver itself. On the other hand, secondary liver cancer comes from cancer spreading to the liver from other places.
Primary liver cancer has several types, with hepatocellular carcinoma (HCC) being the most common in adults. Other types include intrahepatic cholangiocarcinoma and hepatoblastoma, mostly found in kids.
Pediatric vs. Adult Liver Malignancies
Liver cancers in kids and adults are different in many ways. Pediatric liver cancers, like hepatoblastoma, often come with genetic conditions. They face unique challenges in treatment compared to adult liver cancers.
Adult liver cancers, like HCC, are often linked to liver disease, such as cirrhosis. Risk factors include hepatitis B and C, alcohol use, and non-alcoholic fatty liver disease.
What Is a Hepatoma? Defining Hepatocellular Carcinoma

Hepatocellular carcinoma, or hepatoma, is a serious liver cancer. It’s important to understand its clinical definition and characteristics. This liver cancer is a major health issue worldwide.
Clinical Definition and Characteristics
Hepatocellular carcinoma (HCC) starts in the liver’s main cells, called hepatocytes. It’s defined by its unique cell features. Early detection is key because HCC often grows quickly, making treatment harder.
HCC is linked to liver diseases like cirrhosis. It’s also caused by hepatitis B and C, alcohol, and fatty liver disease. Knowing these causes helps prevent and catch HCC early.
“The diagnosis of hepatocellular carcinoma is complex and involves a combination of imaging techniques, laboratory tests, and sometimes liver biopsy.” -A leading medical oncology expert
Epidemiology and Global Prevalence of Hepatoma
HCC rates vary worldwide. They’re higher in areas with lots of hepatitis B, like Asia and Africa. In contrast, North America and Europe have lower rates.
Worldwide, HCC is the fifth most common cancer and the second leading cause of cancer deaths. The number of cases is expected to grow. Public health efforts to lower risk and find HCC early are vital.
- HCC is more common in men than women.
- The incidence of HCC increases with age, typically peaking in the 6th and 7th decades of life.
- Geographic variations in HCC incidence are largely attributed to differences in hepatitis B and C prevalence.
Hepatoblastoma: A Distinct Pediatric Liver Neoplasm
Hepatoblastoma is a special kind of liver cancer in kids. It’s complex and needs a deep understanding of its signs and types.
Clinical Features and Presentation
Hepatoblastoma usually shows up in young children, often before they turn two. It can cause the belly to swell, make kids lose their appetite, and lose weight. Sometimes, doctors can find it during a check-up.
Finding hepatoblastoma can be tricky. Doctors use scans and blood tests to diagnose it. Alpha-fetoprotein (AFP) levels are often high in kids with this cancer, helping doctors spot it.
Histological Subtypes of Hepatoblastoma
Hepatoblastoma has different types based on how the cells look. These are mainly epithelial and mixed types. The epithelial type can be fetal or embryonal, with the fetal type usually being better.
Knowing the type of hepatoblastoma is key for treatment. It helps doctors plan the best care for each child.
In short, hepatoblastoma is a unique liver cancer in kids. Knowing its signs and types is vital for treating it well.
The Genetic Landscape of Hepatoblastoma
Recent studies have uncovered the genetic makeup of hepatoblastoma. This rare liver cancer mainly affects children. It has unique genetic changes that help it grow and spread.
Common Genetic Alterations
Hepatoblastoma has several genetic changes. One key change is in the CTNNB1 gene, which codes for β-catenin. This protein is important in the Wnt signaling pathway. When mutated, β-catenin builds up in the nucleus, turning on genes that help cells grow and live longer.
Other common changes include:
- Mutations in the APC gene, which helps control the Wnt pathway.
- Changes in the NFE2L2 gene, linked to how cells handle oxidative stress.
- Genetic tweaks to the TERT promoter, affecting telomerase activity.
Molecular Pathways Involved in Hepatoblastoma Development
Hepatoblastoma’s growth involves many molecular pathways. The Wnt/β-catenin pathway is key, with CTNNB1 mutations or APC inactivations causing its problems.
Other pathways, like the PI3K/AKT/mTOR and Notch signaling pathways, also play roles. They could be targets for new treatments.
Key molecular pathways involved:
- Wnt/β-catenin signaling pathway.
- PI3K/AKT/mTOR pathway.
- Notch signaling pathway.
Knowing about these genetic changes and pathways is vital. It helps in creating targeted treatments. This can lead to better outcomes for patients with hepatoblastoma.
Hereditary Patterns in Hepatoblastoma Cases
Hepatoblastoma is a rare liver cancer mainly found in children. It often shows up in families, hinting at a genetic link. Researchers are looking into the genes that might cause this cancer.
Studies have found that some families have many cases of hepatoblastoma over generations. This familial clustering hints at a genetic factor in the disease.
Familial Clustering Evidence
The pattern of hepatoblastoma in families suggests a genetic link. Certain genetic syndromes, like Familial Adenomatous Polyposis (FAP) and Beckwith-Wiedemann Syndrome (BWS), raise the risk of this cancer.
For families with a history of this cancer, genetic counseling and screening are key. Early detection is vital for better treatment and outcomes.
Twin Studies and Sibling Risk Assessment
Twin studies have shed light on the genetic risk for hepatoblastoma. They show that twins and siblings of those affected face a higher risk.
A study found that siblings of those with hepatoblastoma are at a higher risk. This underlines the need to watch siblings closely for early signs of the disease.
Understanding the genetic patterns of hepatoblastoma is critical for better screening and prevention in high-risk families. By finding genetic markers and assessing family risk, we can catch this rare cancer early and treat it more effectively.
Familial Adenomatous Polyposis and Hepatoblastoma Risk
Familial adenomatous polyposis (FAP) is a genetic disorder. It increases the risk of developing hepatoblastoma, a rare liver cancer. This shows how important it is to know the genetic factors behind hepatoblastoma.
The APC Gene Mutation Mechanism
The APC gene is key in controlling cell growth and division. Mutations in this gene cause many polyps in the colon, a sign of FAP. Studies link certain APC gene mutations to a higher risk of hepatoblastoma.
APC gene mutations lead to hepatoblastoma risk through complex molecular pathways. Losing APC function causes β-catenin to build up. This protein, when too active, can help tumors grow.
Clinical Management of FAP Families
Managing FAP families requires a detailed plan. Genetic testing is vital to find those with the APC gene mutation. These individuals can then get regular checks and preventive steps to lower their cancer risk, including hepatoblastoma.
For FAP families, genetic counseling is key. It helps them understand their health and make smart choices for their family’s future.
Knowing the genetic link between FAP and hepatoblastoma helps doctors. They can offer specific screenings and early treatments. This could lead to better results for those at risk.
Beckwith-Wiedemann Syndrome as a Hepatoblastoma Predisposition
BWS is a rare genetic disorder that raises the risk of hepatoblastoma in kids. It also increases the chance of other tumors like Wilms tumor. Knowing how BWS works at a genetic and epigenetic level is key to managing this risk.
Genetic and Epigenetic Mechanisms
The genetics of BWS involve changes in genes on chromosome 11p15.5. Abnormalities in the imprinting center 1 (IC1) and imprinting center 2 (IC2) are key. These changes can cause genes that promote growth to be overactive and genes that stop tumors to be silenced.
Important genetic and epigenetic mechanisms include:
- Loss of methylation at IC2, which silences CDKN1C, a tumor suppressor gene.
- Paternal uniparental disomy (UPD) of chromosome 11p15.5, causing IGF2 to be overexpressed, a gene that promotes growth.
- Genetic mutations or deletions in the CDKN1C gene.
Surveillance Guidelines for BWS Patients
Because BWS patients are at higher risk for hepatoblastoma, regular checks are advised. Here are some guidelines:
- Abdominal ultrasounds every 3 months until age 4.
- Checking serum alpha-fetoprotein (AFP) every 3 months until age 4.
- Annual abdominal ultrasounds from age 4 to 7.
These early checks can greatly improve treatment outcomes for BWS kids with hepatoblastoma. It’s vital for families and doctors to follow these guidelines closely.
Other Genetic Syndromes Associated with Hepatoblastoma
Hepatoblastoma is a rare liver cancer that mainly affects kids. It’s linked to several genetic syndromes that raise its risk. Knowing these genetic conditions helps spot high-risk individuals early. This allows for better surveillance and management.
Simpson-Golabi-Behmel Syndrome
Simpson-Golabi-Behmel Syndrome (SGBS) is a rare disorder. It causes kids to grow too fast and have unique facial features. It also raises the risk of tumors, including hepatoblastoma.
The syndrome is caused by GPC3 gene mutations. This gene is important for cell growth. Kids with SGBS need regular check-ups to catch hepatoblastoma early.
Trisomy 18 and Chromosomal Disorders
Trisomy 18, or Edwards syndrome, is a chromosomal disorder. It happens when there’s an extra copy of chromosome 18. This condition leads to severe developmental delays and a higher risk of tumors, like hepatoblastoma.
The exact link between Trisomy 18 and hepatoblastoma isn’t fully understood. But, it’s thought that the extra genetic material can cause tumors to form.
Li-Fraumeni Syndrome and Cancer Predisposition
Li-Fraumeni Syndrome (LFS) is a rare genetic disorder. It greatly increases the risk of many cancers, including breast cancer and sarcomas. In some cases, it also raises the risk of hepatoblastoma.
LFS is caused by TP53 gene mutations. This gene helps prevent cancer by keeping the genome stable. Families with LFS need close cancer surveillance and genetic counseling to manage their risk.
In conclusion, genetic syndromes like Simpson-Golabi-Behmel Syndrome, Trisomy 18, and Li-Fraumeni Syndrome increase the risk of hepatoblastoma. Recognizing these conditions is key for early detection and management of the disease.
Environmental and Non-Genetic Risk Factors
It’s important to know about environmental and non-genetic risk factors for hepatoblastoma. These factors help us find and prevent liver cancer early. While genetics are key, other things also play a part.
Prematurity and Low Birth Weight Correlation
Research links prematurity and low birth weight to a higher risk of hepatoblastoma. Kids born early or with low weight face a greater chance of getting this cancer.
Table: Risk Factors Associated with Prematurity and Low Birth Weight
| Risk Factor | Description | Relative Risk |
| Premature Birth | Birth before 37 weeks of gestation | 2.5 |
| Low Birth Weight | Weight less than 2,500 grams at birth | 1.8 |
Maternal Exposures During Pregnancy
Maternal exposures during pregnancy are linked to hepatoblastoma. This includes chemicals and infections. Some research shows that certain toxins can raise the risk.
Maternal exposure to pesticides and other chemicals is a big worry. Keeping pregnant women safe is key.
Parental Age and Demographic Considerations
Parental age and other factors like socioeconomic status and ethnicity are also studied. Older paternal age, in particular, has been linked to a higher risk in some studies.
Understanding these risk factors helps us spot children at higher risk. We can then work on preventing hepatoblastoma through specific strategies.
Diagnostic Approaches for Hepatic Malignancies
Hepatic malignancies, like hepatoblastoma and hepatoma, need accurate diagnosis for treatment. Doctors use clinical checks, lab tests, and advanced imaging to diagnose these liver cancers.
Biomarkers for Hepatoblastoma and Hepatoma
Biomarkers are key in diagnosing and managing liver cancers. For hepatoblastoma, high alpha-fetoprotein (AFP) levels are common, but not all have it. Hepatoma also shows high AFP levels, but levels can differ a lot.
Other markers, like des-gamma-carboxy prothrombin (DCP) and glypican-3, help in diagnosing hepatoma. These markers help find the disease early and track how it grows.
| Biomarker | Hepatoblastoma | Hepatoma (Hepatocellular Carcinoma) |
| Alpha-fetoprotein (AFP) | Elevated in most cases | Elevated, but variable |
| Des-gamma-carboxy prothrombin (DCP) | Not typically used | May be elevated |
| Glypican-3 | Not typically used | May be elevated |
Advanced Imaging Techniques for Liver Tumors
Advanced imaging is vital for diagnosing and staging liver tumors. Ultrasound, CT, and MRI give important details on tumor size, location, and if it’s invading blood vessels.
CT scans are great for seeing how far the disease has spread and planning surgery. MRI is very sensitive in finding liver lesions and can tell different types of tumors apart.
The right imaging choice depends on the patient’s situation and the tumor’s characteristics.
Genetic Testing and Screening Protocols
Genetic testing plays a key role in understanding hepatoblastoma. It helps us see the disease’s causes and the risk it may pass to families. It’s important to know how genetic testing works and what it means.
When to Consider Genetic Testing
Genetic testing is important for families with a history of hepatoblastoma or related genetic syndromes. For example, conditions like Familial Adenomatous Polyposis (FAP) and Beckwith-Wiedemann Syndrome raise the risk of hepatoblastoma. Families with these conditions should get genetic counseling and testing to learn their risks.
Also, children with early-onset or bilateral hepatoblastoma might benefit from genetic testing. This can help find the genetic causes behind their disease.
Available Testing Methods and Their Accuracy
There are several ways to test for hepatoblastoma risk:
- Gene Panel Testing: Looks at many genes linked to a higher risk of hepatoblastoma.
- Whole Exome Sequencing (WES): Checks the coding parts of most genes for mutations.
- Targeted Mutation Analysis: Focuses on specific known mutations in a family.
These tests are very good at finding known mutations. It’s important to talk about the strengths and weaknesses of each test with a genetic counselor.
| Testing Method | Sensitivity | Specificity |
| Gene Panel Testing | High | High |
| Whole Exome Sequencing | Very High | High |
| Targeted Mutation Analysis | High | Very High |
Interpretation of Genetic Test Results
Understanding genetic test results needs expertise. It’s about knowing what the found mutations mean. A positive result means a higher risk, but it doesn’t mean the disease will definitely happen. A negative result doesn’t mean no risk at all. Genetic counseling is key for families to grasp their test results and make smart choices.
“Genetic testing is a powerful tool, but it must be used judiciously, with careful consideration of the possible psychological impact on families.”
As we go on, genetic testing will keep getting better. It will bring new insights and chances for families dealing with hepatoblastoma.
Treatment Strategies for Hereditary Hepatoblastoma
Treating hereditary hepatoblastoma requires a careful approach. We use the latest in surgery, chemotherapy, and liver transplantation. Let’s look at the different ways to manage this condition.
Surgical Approaches and Considerations
Surgery is key in treating hereditary hepatoblastoma. Complete surgical resection is the main goal, aiming to remove the tumor fully. We look at several factors when choosing surgery, like the tumor’s size, location, and the patient’s health.
- Preoperative imaging to assess tumor extent and vascular involvement
- Surgical techniques such as liver resection or lobectomy
- Intraoperative ultrasound to ensure complete tumor removal
Every case is different, and we weigh the risks and benefits of surgery carefully.
Chemotherapy Regimens and Response Patterns
Chemotherapy is a big part of treating hereditary hepatoblastoma, often used with surgery. Neoadjuvant chemotherapy can shrink tumors, making them easier to remove. We look at different chemotherapy plans, like:
- Platinum-based chemotherapy (e.g., cisplatin)
- Combination regimens (e.g., cisplatin, vincristine, and 5-fluorouracil)
We watch how well chemotherapy works by checking images and tumor markers.
Liver Transplantation in Hereditary Cases
Liver transplantation is an option for patients with big tumors or liver disease. We check if a patient is a good candidate for a transplant based on:
| Criteria | Description |
| Tumor extent | Evaluation of tumor size and vascular involvement |
| Liver function | Assessment of underlying liver disease |
For some patients, liver transplantation could be a cure for hereditary hepatoblastoma.
Long-Term Surveillance for High-Risk Families
High-risk families can greatly benefit from long-term surveillance. This approach helps spot early signs of hepatoblastoma or other cancers. It allows for quick action to be taken.
Monitoring Protocols for Siblings and Relatives
Monitoring siblings and relatives of families with hepatoblastoma history is key. Regular check-ups, screenings, and genetic tests are used. These help find those at higher risk.
Key components of monitoring protocols include:
- Regular abdominal ultrasounds to detect liver tumors early
- Serum alpha-fetoprotein (AFP) level checks, as elevated levels can indicate hepatoblastoma
- Genetic counseling for families with known genetic syndromes associated with hepatoblastoma
Psychosocial Impact of Hereditary Cancer Risk
Knowing you’re at high risk for hepatoblastoma can deeply affect family members. Anxiety, fear, and uncertainty are common. These feelings come from the ongoing surveillance.
Supportive care is vital to manage these effects. This includes psychological counseling, support groups, and educational resources. They help families deal with their situation.
Genetic Counseling for Affected Families
Genetic counseling is key for families facing hepatoblastoma. It gives them vital info and support. Families with a hepatoblastoma diagnosis face not just medical issues but also worry about genetic risks for their family.
Risk Assessment and Communication Strategies
Genetic counseling starts with a detailed risk assessment. It looks at family history, genetic tests, and more to see if others might get hepatoblastoma. It’s important to clearly share this risk so families can make smart health choices.
“Genetic counseling helps families grasp their risks and choices. This tailored approach is vital for families dealing with hepatoblastoma’s emotional and medical challenges.
Reproductive Options and Family Planning
For families with hepatoblastoma history, planning a family is tough. Genetic counseling offers guidance on options like preimplantation genetic diagnosis (PGD) and prenatal tests. These can lower the chance of passing on the genetic risk to kids.
Choosing reproductive options is a personal decision. Our genetic counselors give families all the info and support they need. This ensures they can make choices that fit their values and situation.
As we learn more about hepatoblastoma’s genetics, genetic counseling’s role grows. It offers accurate risk info, clear communication, and reproductive choices. This helps families face this disease with more confidence and understanding.
Conclusion: Current Understanding and Future Directions
We’ve looked into hepatoblastoma and hepatoma, two serious liver cancers. We’ve seen how genetics play a big role, like in familial adenomatous polyposis and Beckwith-Wiedemann syndrome. This shows why genetic tests are key for families at risk.
Looking ahead, research will aim to improve how we diagnose and treat these cancers. New tools like surface-enhanced Raman spectroscopy (SERS) could help a lot. We’re excited to see how this research will help us understand and tackle these diseases better.
Our goal is to make a difference in the lives of those with these cancers. We’re dedicated to top-notch healthcare and support for patients from around the world. This is our promise to advance the field and help more people.
FAQ
What is the difference between hepatoblastoma and hepatoma?
Hepatoblastoma is a rare liver cancer in kids. Hepatoma, or hepatocellular carcinoma, is a liver cancer that mostly affects adults.
Is hepatoblastoma hereditary?
Most cases of hepatoblastoma happen by chance. But, some cases might be linked to genetic syndromes or family history.
What are the genetic syndromes associated with hepatoblastoma?
Certain genetic syndromes raise the risk of hepatoblastoma. These include Familial Adenomatous Polyposis (FAP), Beckwith-Wiedemann Syndrome (BWS), and others.
What is the role of genetic testing in hepatoblastoma diagnosis?
Genetic testing can find genetic mutations linked to hepatoblastoma. This helps doctors plan treatment and check family members.
How is hepatoma (hepatocellular carcinoma) diagnosed?
Doctors use CT or MRI scans and biomarkers like alpha-fetoprotein (AFP) to diagnose hepatoma.
What are the treatment options for hereditary hepatoblastoma?
Treatment for hereditary hepatoblastoma might include surgery, chemotherapy, and liver transplant. It depends on the disease’s extent and the person’s health.
What is the significance of long-term surveillance for high-risk families?
Long-term checks are key for families with a history of hepatoblastoma. They help catch cancers early for treatment.
How does genetic counseling support families affected by hepatoblastoma?
Genetic counseling helps families understand genetic risks of hepatoblastoma. It also guides on reproductive choices and family planning.
What are the environmental and non-genetic risk factors for hepatoblastoma?
Risk factors for hepatoblastoma include being premature, low birth weight, and exposures during pregnancy. Parental age also plays a role.
What is the current understanding of the molecular pathways involved in hepatoblastoma development?
Research shows several molecular pathways in hepatoblastoma development. This includes genetic and epigenetic changes.
What is the relationship between Familial Adenomatous Polyposis (FAP) and hepatoblastoma risk?
FAP increases the risk of hepatoblastoma, mainly in children.
How does Beckwith-Wiedemann Syndrome (BWS) predispose individuals to hepatoblastoma?
BWS involves genetic and epigenetic changes. These increase the risk of developing hepatoblastoma.
References
- Meyers, R. L., Tiao, G., de Ville de Goyet, J., Superina, R., & Aronson, D. C. (2016). Hepatoblastoma state of the art: Pre-treatment extent of disease, surgical resection guidelines and the role of liver transplantation. Current Opinion in Pediatrics, *28*(1), 29–36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4774578/