Last Updated on December 3, 2025 by Bilal Hasdemir
When surgeons remove part of the liver, stopping bleeding is key. The Pringle maneuver is a method used to reduce blood loss. It’s a vital part of liver surgery. What is the Pringle maneuver? Learn about this essential surgical technique clearly explained in a simple and quick guide.
This technique is important in liver surgeries. It’s based on a deep understanding of the liver’s structure. The Pringle maneuver has a long history and is essential for successful liver surgeries.
Key Takeaways
- The Pringle maneuver is a surgical technique used to control bleeding during liver surgery.
- It involves hepatic vascular exclusion to minimize blood loss.
- This technique is critical for the success of liver resection operations.
- The Pringle maneuver has a significant impact on patient outcomes.
- Understanding the Pringle maneuver is essential for medical professionals involved in liver surgery.
Historical Development of Hepatic Vascular Control
The growth of hepatic vascular exclusion techniques has been key in liver surgery’s evolution. Looking back, we see early breakthroughs led to today’s surgical methods.
Early Approaches to Liver Surgery
Liver surgery has a long history, with early efforts facing big blood loss and unclear liver anatomy. Early surgeons had big challenges, like the risk of bleeding and complex liver structures. The start of basic vascular control was a big step forward. It let surgeons do more complex surgeries safely.
- Early liver surgeries had high death rates because of uncontrolled bleeding.
- Basic vascular control techniques cut down on blood loss, improving results.
- Surgeons started trying different ways to block hepatic vessels, setting the stage for better methods.
James Hogarth Pringle’s Contribution to Surgical Science
James Hogarth Pringle made a huge leap in hepatic vascular control. His method, known as Pringle’s maneuver, clamps the hepatoduodenal ligament. This blocks the hepatic artery and portal vein, making liver surgery safer by controlling bleeding.
Pringle’s work did more than just introduce a technique. It showed how vital vascular control is in liver surgery. His insights have shaped how surgeons manage liver blood vessels, influencing many.
- Pringle’s method made liver surgery easier by providing a simple way to control blood flow.
- Using Pringle’s maneuver greatly reduced blood loss during surgery.
- Pringle’s work set the stage.
As we move forward in liver surgery, knowing the history and contributions of pioneers like James Hogarth Pringle is vital. Their work saved many lives and paved the way for today’s advanced surgical techniques.
Understanding the Pringle Maneuver
The Pringle maneuver is a key method to cut down on blood loss during liver surgery. It controls the blood flow to the liver. This is very important during liver surgeries.
Definition and Basic Concept
The Pringle maneuver is a way to stop bleeding from the liver. It involves clamping the hepatoduodenal ligament. This stops the blood flow to the liver, reducing bleeding during surgery.
“The Pringle maneuver is a simple yet effective method for reducing blood loss during liver surgery,” as noted by surgical experts. By temporarily halting the blood flow, surgeons can operate with greater precision and safety.
Evolution of the Technique Over Time
Over the years, the Pringle maneuver has changed a lot. It was first used by James Hogarth Pringle. Now, it includes new ways to stop blood flow, like intermittent clamping.
The Pringle maneuver has gotten better over time. Experts innovative approach has been improved upon. This makes liver surgery safer and more effective.
Today, the Pringle maneuver is a key part of liver surgery. Its improvement shows how far surgery has come.
Anatomical Foundations of the Procedure
The Pringle maneuver is based on knowing the liver’s blood flow. It’s important to understand the liver’s blood structure and the ligaments around it.
Hepatic Vascular Anatomy
The liver gets blood from two main sources: the hepatic artery and the portal vein. The hepatic artery brings oxygenated blood. The portal vein carries blood full of nutrients from the stomach.
The liver’s blood system is complex, with many branches and variations. It’s divided into lobes, each with its own blood supply. The right and left hepatic arteries and portal veins supply these lobes. Knowing this is key for surgeons doing the Pringle maneuver.
- The hepatic artery and portal vein are in the hepatoduodenal ligament.
- The liver’s blood supply is vital for its function and healing.
- Understanding the liver’s blood system is essential for liver surgery.
The Hepatoduodenal Ligament and Portal Triad
The hepatoduodenal ligament connects the liver to the duodenum. It holds the portal triad, which includes the portal vein, hepatic artery, and common bile duct. The portal triad is a key landmark for surgeons doing the Pringle maneuver.
To do the Pringle maneuver, surgeons must find and clamp the hepatoduodenal ligament. This stops blood flow to the liver. They need to know the ligament’s anatomy well.
The portal triad is very important in liver surgery. It supplies the liver with blood and helps drain bile.
- The portal vein brings blood rich in nutrients from the stomach.
- The hepatic artery brings oxygenated blood to the liver.
- The common bile duct drains bile from the liver to the duodenum.
By knowing the basics of the Pringle maneuver, surgeons can do it more accurately and safely. This helps improve patient care.
Clinical Indications for the Pringle Maneuver
Surgeons use the Pringle maneuver in many situations, mainly in liver surgery. It’s key in both urgent and planned surgeries.
Trauma and Emergency Applications
For severe liver trauma, the Pringle maneuver stops bleeding. This is vital in emergencies where fast bleeding can cause serious harm.
It’s also used in urgent cases like ruptured liver tumors or accidental liver injury during surgery.
| Clinical Scenario | Application of Pringle Maneuver |
| Severe Liver Trauma | Control of hemorrhage |
| Ruptured Liver Tumors | Emergency hemorrhage control |
| Iatrogenic Liver Injury | Management of unintended bleeding |
Elective Liver Resections
In elective liver surgeries, the Pringle maneuver reduces blood loss. This makes the surgery clearer and cuts down on blood transfusions.
Contraindications and Limitations
The Pringle maneuver is useful but has certain limits. It’s important for surgeons to know these to use it safely and effectively.
Absolute Contraindications
There are some situations where the Pringle maneuver is not recommended. These include:
- Known or suspected malignant involvement of the hepatoduodenal ligament, as clamping could potentially spread cancer cells.
- Severe portal hypertension with variceal bleeding, where the Pringle maneuver could exacerbate bleeding.
- Thrombosis of the portal vein or hepatic artery, as this could lead to ischemia or other complications.
Relative Contraindications
Some conditions make the Pringle maneuver riskier but not always off-limits. These include:
- Cirrhosis, which can make the liver more vulnerable to damage.
- Pre-existing liver dysfunction, where extra stress from the Pringle maneuver could harm liver function further.
- Previous liver surgery or interventions that may have changed the anatomy or liver function.
Surgeons need to think carefully about these factors before using the Pringle maneuver.
In summary, the Pringle maneuver is a key tool in liver surgery. But, knowing its limits is key for the best results for patients.
Preoperative Planning and Patient Preparation
To get the best results from the Pringle maneuver, surgeons focus on detailed planning and patient prep. This step is key to making sure patients are ready for surgery. It helps lower risks and boosts success rates.
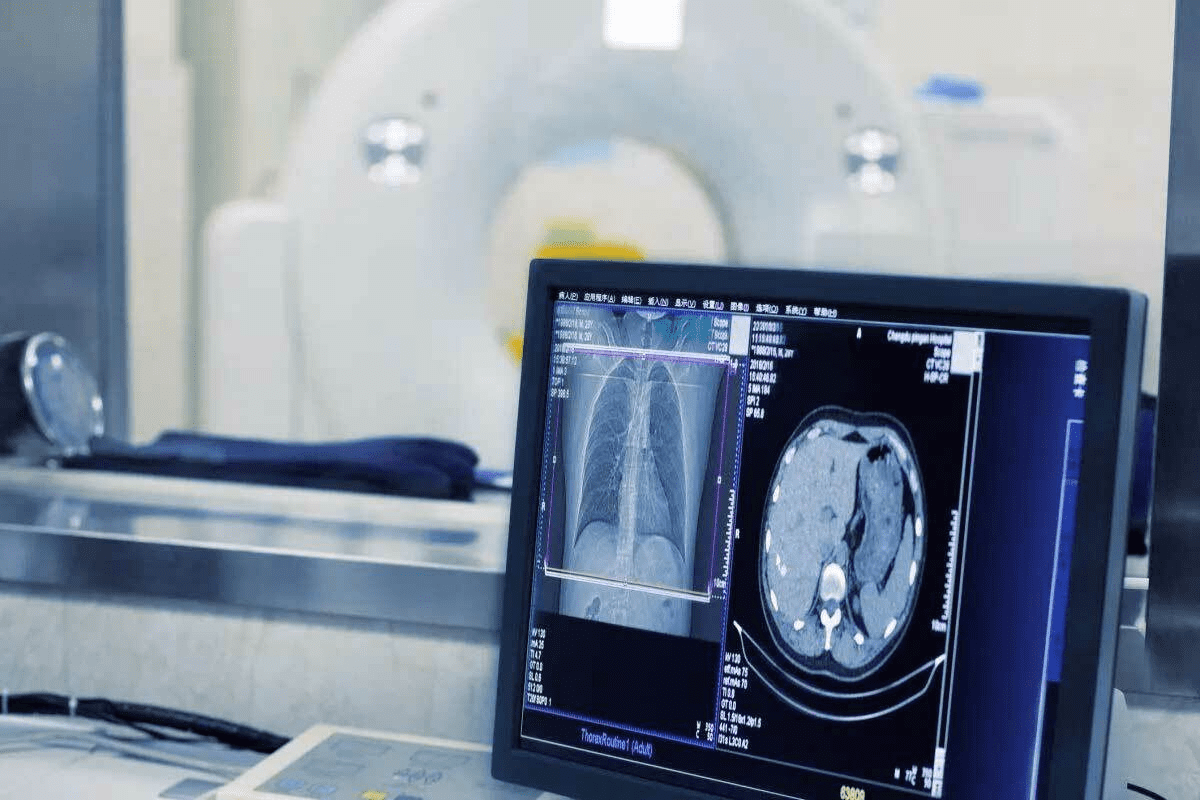
Imaging and Assessment
Imaging before surgery is very important for the Pringle maneuver. We use high-tech scans like CT and MRI. These help us see the liver’s shape, find any special blood vessel patterns, and check liver health or damage.
Good imaging lets us:
- Choose the best way to do the Pringle maneuver
- Understand the risk of bleeding and plan for any problems
- See how well the liver is working and how much it can handle
Patient Optimization Strategies
Getting patients ready for surgery is key to lowering risks. We use several ways to make sure patients are as ready as possible for the Pringle maneuver.
| Optimization Strategy | Description |
| Nutritional Support | Helping patients eat well to aid in healing and prevent problems |
| Management of Coagulopathy | Fixing blood clotting issues to lower bleeding risks |
| Cardiovascular Optimization | Checking and managing heart risks to make sure patients can handle surgery |
Step-by-Step Technique of the Pringle Maneuver
The Pringle maneuver is a key step in liver surgery. It requires careful steps to ensure safety and success.
Patient Positioning and Surgical Access
Getting the patient in the right position is essential. We place them on their back with arms out. This makes the liver area easy to reach.
To get to the liver, we make a cut in the right upper abdomen or a longer cut down the middle. The choice depends on the patient and the surgery needed.
Approach to the Hepatoduodenal Ligament
We then carefully cut through tissues to find the hepatoduodenal ligament. It’s a key area with important blood vessels and ducts.
Being precise is key to avoiding harming these vital structures. We use both sharp and gentle cuts to open up the ligament.
Clamping Techniques and Instruments
With the ligament in sight, we clamp it to stop blood flow. We use tools like the Satinsky clamp or bulldog clamps. The right tool depends on the surgeon and the patient’s body.
| Clamping Instrument | Description | Advantages |
| Satinsky Clamp | A curved clamp used for partial occlusion | Allows for precise control, minimizing damage to surrounding tissues |
| Bulldog Clamp | A spring-loaded clamp for temporary occlusion | Easy to apply, atraumatic, and effective for temporary vascular control |
After clamping, we check if the bleeding has stopped. The clamp stays on for 15-30 minutes to prevent too much damage.
Variations of Vascular Occlusion Techniques
Now, surgeons have many vascular occlusion techniques. This makes liver surgeries safer. The choice of method depends on the patient’s health, the surgery type, and the surgeon’s style.
Continuous vs. Intermittent Pringle Maneuver
The Pringle maneuver can be done in two ways. Continuous occlusion means clamping the hepatoduodenal ligament all the time during surgery. Intermittent occlusion means clamping for a bit, then letting blood flow back.
“The intermittent Pringle maneuver is often preferred,” studies say. It lets the liver get blood back, which might help it stay healthier.
Choosing between continuous and intermittent depends on how long the surgery will take and the liver’s health.
Selective Vascular Occlusion Approaches
Selective vascular occlusion means stopping blood flow to specific liver areas. This helps cut down on bleeding while keeping other parts of the liver alive.
This method needs a good understanding of the liver’s blood system. It’s very useful for complex surgeries or when the liver is already sick.
By picking which blood vessels to block, surgeons can protect the liver from damage.
Physiological Impact During Liver Surgery
The Pringle maneuver affects the body in many ways during liver surgery. It impacts blood flow and can cause injury when blood flow is restored. Knowing these effects is key to avoiding problems and improving patient care.
Hemodynamic Changes During Clamping
Applying the Pringle maneuver causes blood flow to the liver to stop. This leads to a drop in blood flow to the liver. It also makes blood pressure go up, which can be dangerous.
The liver’s work is also affected. It helps clean the blood, make proteins, and control sugar levels. When the Pringle maneuver is used, these functions slow down. This can cause problems that need careful attention after surgery.
Ischemia-Reperfusion Injury Mechanisms
Ischemia-reperfusion injury is a big worry with the Pringle maneuver. When blood flow stops and then starts again, liver cells get damaged. This damage is caused by many factors, including harmful chemicals and inflammation.
This injury happens because of how liver cells work together. Knowing this helps doctors find ways to reduce injury and improve results for patients. By managing the Pringle maneuver carefully, doctors can lessen the risk of injury and its complications.
Benefits of the Pringle Maneuver in Hepatobiliary Surgery
Hepatobiliary surgeons use the Pringle maneuver a lot. It helps cut down on blood loss and makes the surgery area clearer. This method is key in liver surgery, leading to better results for patients.
Blood Loss Reduction and Transfusion Requirements
The Pringle maneuver cuts down on blood loss during liver surgeries. It works by stopping the blood flow to the liver. This makes the surgery area less bloody.
Using the Pringle maneuver also means fewer blood transfusions. A study showed that using this method led to fewer blood transfusions. This is good news for patients.
Improved Surgical Visibility and Technical Control
Less blood means a clearer view for the surgeon. This makes it easier to do precise work. It also lowers the chance of mistakes during surgery.
| Outcome | With Pringle Maneuver | Without Pringle Maneuver |
| Blood Loss (ml) | 300 ± 100 | 800 ± 200 |
| Transfusion Rate (%) | 20 | 50 |
| Surgical Time (minutes) | 180 ± 30 | 240 ± 40 |
In summary, the Pringle maneuver is very helpful in liver surgery. It reduces blood loss, lowers the need for blood transfusions, and makes the surgery area clearer. All these benefits lead to better results for patients.
Potential Complications and Risk Management
It’s important to know the risks of the Pringle maneuver in liver surgery. This technique is useful but comes with dangers. Surgeons need to be ready to handle these risks.
Immediate Surgical Complications
Right away, problems can happen like hemorrhage or vascular injury. To avoid these, surgeons plan carefully before surgery and use precise techniques.
Another issue is cardiac instability from the procedure’s stress. It’s key to watch the patient’s heart closely during the Pringle maneuver.
Long-term Hepatic Function Consequences
The Pringle maneuver can affect the liver long-term. Ischemia-reperfusion injury is a big worry, leading to liver problems after surgery. It’s important to understand this injury to lessen its effects.
Keeping an eye on the liver’s function over time is needed. This means checking liver enzymes and function tests for any lasting damage.
Managing risks well is key to avoiding problems with the Pringle maneuver. This means taking care of the patient from start to finish, including after surgery.
Postoperative Care and Management
After the Pringle maneuver, care is key to avoid complications and ensure good results. It’s important to manage challenges that come up after surgery well.
Immediate Recovery Considerations
Right after surgery, keeping an eye on vital signs and blood flow is vital. We also focus on pain management. It’s important for comfort and recovery.
Using advanced monitoring and care plans helps spot problems early. For example, serial lactate measurements and liver function tests help track recovery. They help us see if things are going as planned.
| Monitoring Parameter | Immediate Postoperative Period | First 24 Hours |
| Vital Signs | Continuous monitoring | Frequent checks |
| Liver Function Tests | Baseline assessment | Serial measurements |
| Pain Management | Aggressive pain control | Adjust as necessary |
Monitoring for Delayed Complications
Watching for complications later on is also important. Issues like ischemia-reperfusion injury or hepatic dysfunction can show up later.
“The key to managing delayed complications lies in vigilant monitoring and a proactive approach to addressing any deviations from the expected recovery pathway.”— Expert in Hepatobiliary Surgery
Regular check-ups with tests and scans help catch problems early. We also teach patients to watch for signs that need quick medical help. This helps them stay involved in their healing.
With a detailed care plan, we can make sure patients do well after the Pringle maneuver. This helps avoid complications.
Alternative Vascular Control Techniques
Liver surgery is getting better, thanks to new ways to control blood flow. The Pringle maneuver is key, but new methods help in different situations. They aim to make surgery safer and better for patients.
Different surgeries need different approaches. New techniques let surgeons handle tough cases better. They’re vital for both planned and emergency surgeries, helping control bleeding and keeping blood flow stable.
Total Hepatic Vascular Exclusion
Total Hepatic Vascular Exclusion (THVE) stops blood from flowing into and out of the liver. It’s great for complex surgeries or tumors near major veins.
THVE needs careful planning and doing. It involves clamping the liver’s main blood supply and the vena cava above and below it. This makes the liver area bloodless, helping in some surgeries.
Selective Inflow Occlusion Methods
Selective inflow occlusion stops blood to just the liver part being removed. It’s good for localized problems, giving better control over bleeding.
There are many ways to do selective inflow occlusion. You can clamp the liver’s blood supply or use hemihepatic vascular occlusion. This way, less of the liver is affected, which might lower the risk of liver problems after surgery.
Total Hepatic Vascular Exclusion and Selective Inflow Occlusion are great alternatives to the Pringle maneuver. They help surgeons tackle complex liver surgeries better. Learning these techniques can lead to better results for patients having liver surgery.
Special Considerations for Different Patient Populations
The Pringle maneuver is used differently for various patients, like those with cirrhosis or children. We must consider each patient’s unique needs to get the best results.
Application in Cirrhotic Patients
Cirrhotic patients face special challenges with the Pringle maneuver. Their liver disease can make it harder for the liver to handle ischemia, raising the risk of liver failure after surgery. It’s important to carefully plan and assess each patient before surgery.
The severity of cirrhosis, measured by the Child-Pugh score, helps us decide how to proceed. Those with more severe cirrhosis might need different approaches or strategies for controlling blood flow.
| Child-Pugh Score | Liver Function | Pringle Maneuver Considerations |
| A (5-6) | Mild impairment | Generally safe with standard precautions |
| B (7-9) | Moderate impairment | Requires careful consideration and potentially modified |
| C (10-15) | Severe impairment | High risk; alternative strategies may be preferable |
Pediatric Liver Surgery Adaptations
Pediatric liver surgery comes with its own set of challenges. The smaller size and developing bodies of children require special tools and techniques. Miniaturized instruments and precise surgical techniques are key to safely using the Pringle maneuver in kids.
The specific conditions of pediatric patients, like biliary atresia or liver tumors, also play a role. We must tailor our approach to meet each child’s unique needs.
By understanding these special considerations and adapting our approach, we can improve outcomes for all patients. This ensures better care and results for everyone.
Technological Advancements in Hepatic Vascular Control
New technology is changing how we do surgery on the liver. We’re moving towards more precise and less invasive methods. This makes patients recover faster and do better overall.
Imaging-Guided Precision Techniques
Imaging-guided techniques are making a big difference in liver surgery. They let surgeons see the liver’s blood vessels in real time. This makes it easier to work on complex areas.
Key Benefits of Imaging-Guided Techniques:
- Enhanced precision in vascular control
- Reduced risk of complications
- Improved patient outcomes
Tools like intraoperative ultrasound and cone-beam CT are key. They give detailed pictures of the liver’s blood vessels. This helps surgeons plan and do vascular control more accurately.
Minimally Invasive and Robotic Applications
More surgeons are using minimally invasive and robotic methods for liver surgery. These methods are better than old-school open surgery. They cause less damage and help patients heal faster.
Advantages of Minimally Invasive and Robotic Surgery:
| Feature | Minimally Invasive | Robotic |
| Precision | High | Very High |
| Recovery Time | Reduced | Reduced |
| Scarring | Minimal | Minimal |
Robotic systems give surgeons more control and a better view. This makes it easier to do complex surgeries. As tech gets better, we’ll see even more improvements in robotic liver surgery.
Conclusion
The Pringle maneuver is key in liver surgery. It helps control blood flow and cuts down on blood loss during complex surgeries. We’ve looked at its history, how it works, and its uses in this article.
It’s important for surgeons to know about the Pringle maneuver. This knowledge helps them do better surgeries. It makes the surgery safer and less bloody.
Choosing the right patients and planning well are also key. This way, the Pringle maneuver can help a lot. But, it’s also important to be careful to avoid problems.
As liver surgery gets better, so does the Pringle maneuver. New tech and ways to do things are coming. This means surgeons need to keep up with the Pringle maneuver.
The Pringle maneuver will keep being a big help in liver surgery. It will help make surgeries better for patients. This is good news for everyone involved in liver surgery.
FAQ
What is the Pringle maneuver and its significance in liver surgery?
The Pringle maneuver is a surgical method used to stop bleeding in liver surgery. It involves clamping the hepatoduodenal ligament. This ligament holds the hepatic artery and portal vein. It’s key for reducing blood loss and making the surgery area clearer.
Who developed the Pringle maneuver?
James Hogarth Pringle, a renowned surgeon, created the Pringle maneuver. He made big contributions to liver surgery.
What are the indications for using the Pringle maneuver?
The Pringle maneuver is used in many situations. This includes emergency cases and planned liver surgeries. It helps control bleeding and improve surgery results.
Are there any contraindications to using the Pringle maneuver?
Yes, there are times when the Pringle maneuver should not be used. This includes certain health conditions and unique body structures.
How is the Pringle maneuver performed?
To perform the Pringle maneuver, a clamp is placed on the hepatoduodenal ligament. This blocks the hepatic artery and portal vein.
What are the benefits of using the Pringle maneuver in hepatobiliary surgery?
Using the Pringle maneuver has many benefits. It cuts down on blood loss and the need for blood transfusions. It also makes the surgery area clearer and improves control during surgery. All these help in better patient outcomes.
What are the possible complications of the Pringle maneuver?
Complications can include immediate issues like bleeding or damage to blood vessels. There can also be long-term effects on liver function, like ischemia-reperfusion injury.
How can patients be optimized for the Pringle maneuver?
Patients can be prepared for the Pringle maneuver through detailed planning before surgery. This includes imaging and health assessments. It also involves strategies to improve overall health and reduce surgery risks.
Are there alternative vascular control techniques to the Pringle maneuver?
Yes, there are other methods like total hepatic vascular exclusion and selective inflow occlusion. These are used in specific situations.
How does the Pringle maneuver impact different patient populations?
The Pringle maneuver needs special care in certain groups, like those with cirrhosis or children. It’s important to ensure safe and effective use in these cases.
What are the latest advancements in hepatic vascular control?
New advancements include using imaging for precise techniques and minimally invasive surgeries. These are making liver surgery safer and more effective.
What is the difference between continuous and intermittent Pringle maneuver?
Continuous Pringle involves keeping the clamp on all the time. Intermittent Pringle means clamping and then releasing to reduce damage from blood flow changes.
How does the Pringle maneuver affect hepatic function?
The Pringle maneuver can affect liver function due to damage from blood flow changes. Careful management and monitoring can help minimize this damage.
References:
- Hora, S. (2023). Liver Injury and Regeneration: Current Understanding, New Perspectives. Frontiers in Medicine. https://pmc.ncbi.nlm.nih.gov/articles/PMC10486351