Last Updated on December 1, 2025 by Bilal Hasdemir

Approximately 80,000 people in the United States are diagnosed with lymphoma each year. Early detection is key, and blood tests are a big help in finding it.
Knowing how lymphoma lab tests work is important. These tests are not the only way to find lymphoma. But, they are a key tool to spot signs of this cancer.
Key Takeaways
- Lymphoma diagnosis often involves a combination of tests, including blood work and lab tests.
- Understanding the role of blood tests in lymphoma diagnosis is important for patients.
- Early detection of lymphoma greatly improves treatment chances.
- Blood tests can show signs that might mean lymphoma.
- Finding out you have lymphoma is more than just blood tests.
The Nature of Lymphoma and Detection Challenges
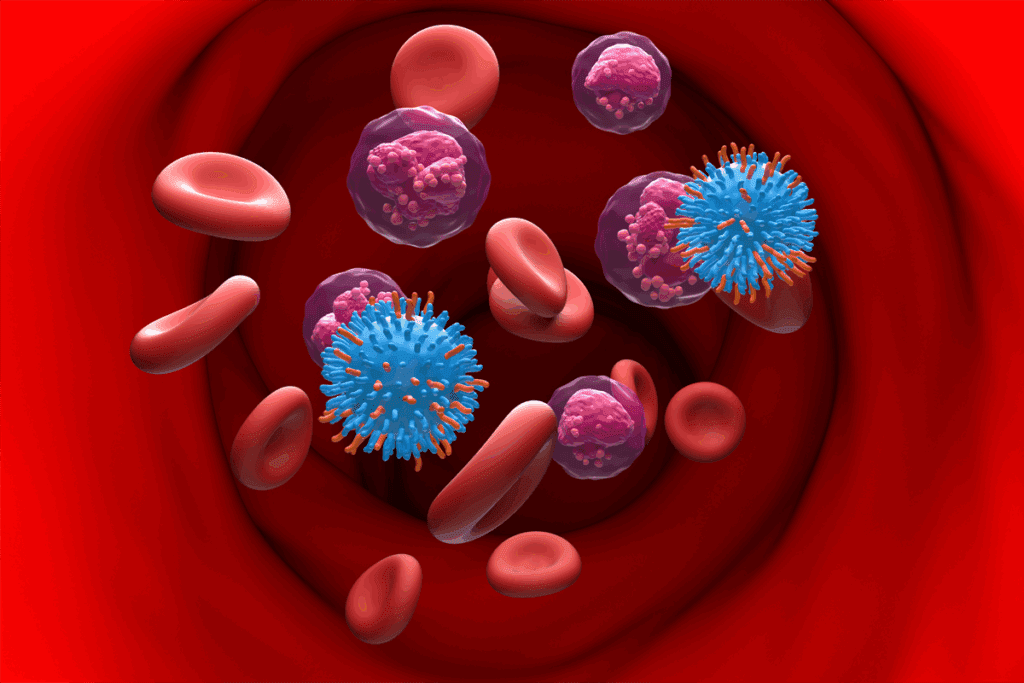
Lymphoma is a complex cancer that affects the immune system. It starts in the lymphocytes, which are white blood cells important for fighting off infections. Because of its different forms and early symptoms that are hard to spot, finding lymphoma early is tough.
What is Lymphoma?
Lymphoma is a cancer that starts in the lymphatic system, which is part of our immune system. It happens when lymphocytes grow out of control. Lymphoma is divided into two main types: Hodgkin lymphoma and non-Hodgkin lymphoma. Each type has its own characteristics and treatment options.
Types of Lymphoma: Hodgkin vs. Non-Hodgkin
Hodgkin lymphoma is known for having Reed-Sternberg cells in the lymph nodes. It usually grows in a predictable way and is easier to treat if caught early. Non-Hodgkin lymphoma, by contrast, is a group of lymphomas without Reed-Sternberg cells. It can be more aggressive and harder to treat.
Why Lymphoma Detection Can Be Complex
Finding lymphoma can be hard because its symptoms are not specific. Symptoms like swollen lymph nodes, fever, night sweats, and weight loss can look like other illnesses. This can cause delays in getting a correct diagnosis. Also, lymphoma can grow in different parts of the body, so doctors need to use many tests to find it.
Lymphoma Blood Work: Overview of Diagnostic Approach
Blood tests are key in finding lymphoma. They check your health and look for signs of lymphoma or other problems.
Can Blood Tests Definitively Diagnose Lymphoma?
Blood tests are very important but can’t always say for sure if you have lymphoma. They might show signs that suggest lymphoma, but more tests are needed for a clear diagnosis.
Blood tests can reveal:
- Abnormal white blood cell counts
- Abnormal lymphocyte morphology
- Elevated levels of certain proteins or enzymes
Blood Tests as Screening Tools
Blood tests are great for spotting people who might need more tests. They help keep an eye on your health and catch problems early.
The Diagnostic Pathway
Diagnosing lymphoma involves several steps. It starts with blood tests and might include imaging and biopsies. Knowing this process is important for both patients and doctors.
| Diagnostic Step | Purpose |
| Blood Tests | Initial screening, overall health assessment |
| Imaging Studies | Assess the extent of disease |
| Biopsy | Definitive diagnosis |
Complete Blood Count (CBC) and Lymphoma Signs
A Complete Blood Count (CBC) is a key test for finding lymphoma signs. It checks the blood for red and white cells and platelets. This gives clues about the body’s health and any problems.
Components of a CBC
A CBC looks at several important parts of the blood. These parts help show if lymphoma or other health issues are present. The main parts are:
- White Blood Cell Count (WBC): Shows how many white blood cells are in the blood. These cells fight off infections.
- Red Blood Cell Count (RBC): Counts the red blood cells, which carry oxygen.
- Platelet Count: Checks the number of platelets, which help the blood clot.
- Hemoglobin (Hb): Measures the hemoglobin in red blood cells.
- Hematocrit (Hct): Looks at the red blood cells’ proportion in the blood.
Common CBC Abnormalities in Lymphoma
Lymphoma can change the results of a CBC. Some common changes include:
| CBC Component | Abnormality | Possible Indication |
| White Blood Cell Count | Elevated or abnormal cells | Lymphoma or infection |
| Red Blood Cell Count | Low count (anemia) | Lymphoma affecting bone marrow |
| Platelet Count | Low or high count | Bone marrow involvement or other conditions |
Changes in a CBC might suggest lymphoma. But, more tests are needed to be sure.
Abnormal White Blood Cells in Lymphoma Patients
Abnormal white blood cells are a key sign of lymphoma. They play a big role in diagnosing this complex disease. White blood cells help fight off infections and diseases. When they change, it can mean lymphoma is present.
Elevated White Blood Cell Count
Many lymphoma patients have more white blood cells than normal. This is called leukocytosis. It happens when the body makes more white blood cells than it should. This can be a sign of cancer in lymphoma patients.
The meaning of having more white blood cells can vary. For example, in some non-Hodgkin lymphoma, the count goes up a lot. This is because cancerous lymphocytes are growing.
Abnormal Lymphocyte Morphology
Lymphocytes are white blood cells important for fighting off infections. In lymphoma, these cells can change shape or size. They might look bigger or have strange shapes.
Doctors can see these changes with a blood smear. This tool lets them look at blood cells closely. Finding these changes helps doctors tell lymphoma apart from other diseases.
Atypical Lymphocytes vs. Malignant Cells
Telling apart atypical lymphocytes and malignant cells is key in diagnosing lymphoma. Atypical lymphocytes can show up in many conditions, not just lymphoma. Malignant cells, though, are cancerous and point directly to lymphoma or other cancers.
Doctors use advanced tests like flow cytometry and molecular testing to find these cells. Knowing the difference between them is vital for the right diagnosis and treatment.
Low Red Blood Count and Anemia as Cancer Signs
Anemia, a low red blood count, is a big worry for lymphoma patients. It causes fatigue, weakness, and shortness of breath. These symptoms really hurt the quality of life.
Anemia is more than just a simple condition. It often means there’s something serious going on, like in cancer patients. For lymphoma patients, knowing about anemia is key to managing their disease well.
Types of Anemia Associated with Lymphoma
There are several anemia types linked to lymphoma, including:
- Anemia of chronic disease
- Iron deficiency anemia
- Vitamin deficiency anemia
Each type has its own causes and effects on lymphoma patients.
| Type of Anemia | Causes | Implications |
| Anemia of Chronic Disease | Inflammation, chronic illness | Common in lymphoma patients, reflects disease activity |
| Iron Deficiency Anemia | Lack of iron, chronic blood loss | May require iron supplements, indicates possible gastrointestinal issues |
| Vitamin Deficiency Anemia | Lack of vitamin B12 or folate | Can be treated with vitamin supplements, dietary changes |
How Lymphoma Causes Anemia
Lymphoma can lead to anemia in several ways. Cancer cells can fill up the bone marrow, causing inflammation and nutritional deficiencies.
The presence of anemia in lymphoma patients can significantly impact treatment outcomes and quality of life, making its management a critical aspect of care.
Differentiating Lymphoma-Related Anemia from Other Causes
It’s important to tell if anemia is from lymphoma or something else. A detailed diagnostic process is needed. This includes blood tests, bone marrow biopsies, and nutritional checks.
Knowing why a patient has anemia is vital. It helps doctors create a treatment plan that tackles both the anemia and the lymphoma.
Platelet Count Abnormalities in Lymphoma
Lymphoma patients often see changes in their platelet count. This is a key part of their blood work. Changes in platelet count can affect how lymphoma is diagnosed, treated, and managed.
Thrombocytopenia in Lymphoma
Thrombocytopenia, or low platelet count, is common in lymphoma patients. It can happen for many reasons, like lymphoma cells in the bone marrow, chemotherapy, or radiation therapy. Thrombocytopenia can increase the risk of bleeding, which is a big concern for those being treated.
- Bone marrow infiltration by lymphoma cells
- Chemotherapy-induced myelosuppression
- Radiation therapy affecting the bone marrow
Mechanisms of Platelet Disruption
There are many reasons why platelet counts can be abnormal in lymphoma. Lymphoma cells can invade the bone marrow, disrupting how blood cells are made. Also, treatments like chemotherapy can weaken the bone marrow, making fewer platelets.
The bone marrow is a common site for lymphoma involvement, and its infiltration can lead to various cytopenias, including thrombocytopenia.
No specific author cited
Clinical Significance of Platelet Abnormalities
It’s important to understand the impact of platelet count abnormalities in lymphoma. Keeping an eye on platelet counts helps figure out the risk of bleeding and adjust treatment plans. Also, if platelet counts stay low, it might mean changing the treatment or looking for other reasons.
| Condition | Impact on Platelet Count | Clinical Significance |
| Thrombocytopenia | Low platelet count | Increased risk of bleeding |
| Lymphoma Treatment | Variable effects on platelet count | Requires careful monitoring |
In conclusion, changes in platelet count, like thrombocytopenia, are big concerns in managing lymphoma. Knowing why these changes happen and what they mean is key to giving the best care to lymphoma patients.
Blood Markers for Lymphoma: Biochemical Indicators
Biochemical indicators are key in diagnosing and tracking lymphoma. These markers in the blood offer vital info on the disease’s presence and growth.
LDH (Lactate Dehydrogenase) Blood Levels
Lactate Dehydrogenase (LDH) is an enzyme in all living cells. High LDH blood levels suggest tissue damage or disease, like lymphoma. More aggressive lymphoma types often have higher LDH levels.
Monitoring LDH levels is vital for understanding lymphoma’s severity and treatment response. A drop in LDH levels usually means the treatment is working well.
ESR (Erythrocyte Sedimentation Rate) Test
The ESR test shows how fast red blood cells settle in a blood sample. It measures body inflammation. Lymphoma can cause inflammation, raising ESR levels.
An elevated ESR suggests more tests and studies are needed. It’s not specific to lymphoma but is a clue for further investigation.
Blood Protein Markers
Certain blood protein markers are linked to lymphoma. Blood tests can find these proteins. They help diagnose and track the disease.
| Marker | Description | Clinical Significance |
| LDH | Lactate Dehydrogenase enzyme | Elevated levels indicate tissue damage or disease severity |
| ESR | Erythrocyte Sedimentation Rate | Indirect measure of inflammation |
| Blood Protein Markers | Various proteins associated with lymphoma | Aids in diagnosis and monitoring |
Knowing about these biochemical indicators is key to managing lymphoma. By looking at LDH blood levels, ESR test results, and blood protein markers, doctors can understand the disease’s progress and treatment response.
Specialized Blood Tests for Lymphoma Detection
Lymphoma diagnosis often uses special blood tests. These include flow cytometry and molecular testing. These methods have greatly improved how accurately we can find lymphoma.
Flow Cytometry Test
Flow cytometry is a detailed lab method. It looks at cells in a fluid, like blood. It helps spot abnormal lymphocytes by checking their surface markers and other traits.
Key benefits of flow cytometry include:
- Identifying specific types of lymphoma cells
- Distinguishing between different lymphoma subtypes
- Providing information on the genetic characteristics of the lymphoma cells
Peripheral Blood Smear Analysis
A peripheral blood smear is a tool for diagnosing. It involves looking at blood under a microscope. This test can show if there are odd shapes, sizes, or numbers of blood cells, which might mean lymphoma.
A peripheral blood smear can show:
- Atypical lymphocytes or other abnormal cells
- Changes in the morphology of blood cells
- Presence of lymphoma cells in the bloodstream
Cytogenetic Testing
Cytogenetic testing looks at cell chromosomes for genetic issues linked to lymphoma. This info is key for diagnosis, understanding the disease’s outlook, and planning treatment.
“Cytogenetic analysis has become an essential tool in the diagnosis and management of hematological malignancies, including lymphoma.”
Molecular Testing
Molecular testing uses various methods to find specific genetic changes linked to lymphoma. These tests give important details for diagnosis, understanding the disease’s outlook, and guiding treatment choices.
| Molecular Test | Purpose |
| PCR (Polymerase Chain Reaction) | Detects specific genetic mutations |
| FISH (Fluorescence In Situ Hybridization) | Identifies chromosomal abnormalities |
| Next-Generation Sequencing (NGS) | Analyzes multiple genes simultaneously |
These blood tests, like flow cytometry, peripheral blood smear analysis, cytogenetic testing, and molecular testing, are critical for finding and diagnosing lymphoma. They give detailed info about lymphoma cells. This helps doctors create effective treatment plans.
Beyond Blood Work: Confirmatory Diagnostic Tests
Tests like lymph node biopsy and imaging studies are key in diagnosing lymphoma. Blood tests give a first look, but these tests confirm the diagnosis and show how far the disease has spread.
Lymph Node Biopsy: The Gold Standard
A lymph node biopsy is the top choice for diagnosing lymphoma. It involves taking out a lymph node or part of it for a closer look. The sample is then checked for cancer cells to figure out the type and stage of lymphoma.
Types of Lymph Node Biopsies:
- Excisional biopsy: Removing an entire lymph node
- Incisional biopsy: Removing a part of a lymph node
- Core needle biopsy: Using a needle to take a sample from a lymph node
Bone Marrow Biopsy Procedures
A bone marrow biopsy is also a key test for lymphoma. It takes a sample of bone marrow for examination. This test shows if lymphoma has reached the bone marrow.
The Procedure:
- The patient is given local anesthesia
- A needle is inserted into the bone to extract marrow
- The sample is examined for cancer cells
| Diagnostic Test | Purpose | Procedure |
| Lymph Node Biopsy | Diagnose lymphoma, determine type and stage | Remove a lymph node or part of it for examination |
| Bone Marrow Biopsy | Check if lymphoma has spread to the bone marrow | Extract a bone marrow sample using a needle |
| Imaging Studies | Assess the extent of lymphoma spread | Use CT, PET, or MRI scans to visualize lymphoma |
Imaging Studies in Lymphoma Diagnosis
Imaging studies like CT scans, PET scans, and MRI are vital for seeing how far lymphoma has spread. They help in figuring out the disease’s stage and planning treatment.
By combining results from lymph node biopsy, bone marrow biopsy, and imaging studies, doctors can accurately diagnose lymphoma. They can then create a good treatment plan.
Pediatric Lymphoma: Special Considerations in Blood Work
Diagnosing lymphoma in kids is different from adults. It has its own set of challenges. These differences make pediatric lymphoma diagnosis unique.
Blood Test Differences in Children
Blood tests for kids are similar to adults but have key differences. Kids’ bodies are growing, which changes how we read blood test results. For example, what’s normal for blood cell counts changes with age.
Key differences in pediatric blood tests include:
- Age-dependent normal ranges for blood cell counts
- Higher lymphocyte counts in children compared to adults
- Different implications of certain abnormalities
Common Blood Abnormalities in Pediatric Lymphoma
In kids with lymphoma, some blood issues are common. These include:
- Elevated white blood cell count
- Anemia or low red blood cell count
- Thrombocytopenia or low platelet count
These signs might point to lymphoma, but they’re not the only cause. A full check-up is needed to confirm the diagnosis.
| Blood Abnormality | Possible Indication |
| Elevated WBC | Potential lymphoma or infection |
| Anemia | Lymphoma or bone marrow involvement |
| Thrombocytopenia | Bone marrow suppression or lymphoma |
Diagnostic Challenges in Children
Diagnosing lymphoma in kids is tough. Symptoms can be vague, and the disease can grow fast. Kids’ smaller size and growing bodies make tests and readings tricky.
Healthcare providers need to know these challenges. This helps them make accurate diagnoses and plan effective treatments for kids with lymphoma.
Limitations of Blood Tests in Lymphoma Diagnosis
Diagnosing lymphoma with blood tests has its challenges. Blood tests are important but only part of the process.
Why Blood Tests Alone Are Not Sufficient
Blood tests can show if lymphoma might be present. But they can’t confirm it on their own. This is because lymphoma cells might not be in the blood or hard to find.
Lymphoma diagnosis often requires a combination of diagnostic approaches. This includes imaging, biopsies, and other tests. Blood tests can hint at lymphoma, but more tests are needed to be sure.
False Positives and False Negatives
Blood tests for lymphoma can also have false positives and negatives. False positives mean a test says you have lymphoma when you don’t. False negatives mean a test misses lymphoma when it’s there.
| Result Type | Description | Implication |
| False Positive | Test indicates lymphoma when it’s not present | Unnecessary anxiety and further testing |
| False Negative | Test fails to detect lymphoma when it’s present | Delayed diagnosis and treatment |
Types of Lymphoma Less Likely to Show in Blood
Some lymphomas are harder to find with blood tests. For example, lymphomas stuck in lymph nodes or tissues might not show up in blood tests.
It’s key for doctors and patients to know these limits. This shows the need for a full diagnostic plan, not just blood tests.
Interpreting Lymphoma Blood Work Results
Understanding blood test results for lymphoma can be tricky. But it’s key to diagnosing the disease. Blood tests give important clues about lymphoma’s presence and growth. This helps doctors make the best care plans for patients.
Understanding Your Blood Test Report
A blood test report for lymphoma has several important parts. These include the Complete Blood Count (CBC), blood chemistry tests, and markers like LDH. Knowing what these parts mean is vital for correct interpretation.
- Complete Blood Count (CBC): Checks different blood cell types, like red and white blood cells, and platelets.
- Blood Chemistry Tests: Looks at blood chemicals, such as LDH, which can be high in lymphoma.
- Specific Markers: Markers like LDH can show if lymphoma is present or getting worse.
What Different Abnormalities May Indicate
Abnormal blood test results can point to different aspects of lymphoma. For example, a high white blood cell count might mean lymphoma cells are in the blood. Low red blood cells or anemia could also hint at lymphoma, as it might affect the bone marrow.
- Elevated White Blood Cell Count: Could mean lymphoma cells are in the blood.
- Low Red Blood Cell Count or Anemia: Linked to lymphoma because it might affect the bone marrow.
- Abnormal Platelet Count: Thrombocytopenia or thrombocytosis can happen if lymphoma impacts the bone marrow.
The Importance of Trend Analysis
Watching how blood test results change over time is key. This helps doctors see how lymphoma is growing. It also lets them check if treatments are working and adjust plans as needed.
“Monitoring blood test results over time is vital for understanding lymphoma’s dynamics and tailoring treatments.”
Expert Opinion
When to Seek Additional Testing
Even with blood tests, sometimes more is needed. Tests like lymph node or bone marrow biopsies might be required. They help confirm the diagnosis or see how far lymphoma has spread.
- Unclear or Inconclusive Blood Test Results: May need more tests to be sure.
- Suspected Lymphoma: Biopsies can confirm if it’s lymphoma.
- Monitoring Treatment Response: Regular tests help see if treatments are working.
Monitoring Lymphoma Through Blood Work After Diagnosis
Monitoring lymphoma through blood work is key to check treatment success and catch relapse early. After a lymphoma diagnosis, regular blood tests are vital for ongoing care.
Tracking Treatment Response
Blood work after a lymphoma diagnosis helps track treatment success. Blood tests measure proteins or markers linked to lymphoma activity. For example, a drop in lactate dehydrogenase (LDH) levels shows treatment is working well.
A study in the Journal of Clinical Oncology showed LDH levels are critical in monitoring lymphoma treatment. Patients with normal LDH levels after treatment had better outcomes than those with high levels.
| Marker | Significance | Implication for Treatment Response |
| LDH | Lactate Dehydrogenase levels | Decrease indicates positive response |
| White Blood Cell Count | Measure of immune response | Normalization suggests recovery |
| Absolute Lymphocyte Count | Indicator of lymphoma activity | Decrease may indicate effective treatment |
Detecting Relapse Through Blood Tests
Blood work is also key for catching lymphoma relapse. Regular tests can spot changes in blood markers that signal disease return. Early detection of relapse can significantly impact treatment outcomes, allowing for timely intervention.
Regular blood tests are vital for monitoring lymphoma patients, enabling early detection of relapse and prompt initiation of salvage therapy.
Long-term Monitoring Protocols
Long-term monitoring of lymphoma patients includes regular blood tests to keep the disease in remission. The test frequency depends on lymphoma type, stage, and treatment.
A typical long-term monitoring protocol might include:
- Regular CBCs to monitor blood cell counts
- Periodic LDH tests to assess lymphoma activity
- Imaging studies as recommended by the healthcare provider
By using these methods, healthcare providers can give thorough care to lymphoma patients. This improves outcomes and quality of life.
Conclusion
Blood tests are key in finding and tracking lymphoma. Tests like the Complete Blood Count (CBC) and flow cytometry help spot signs of the disease. This is because they can find odd white blood cell counts and other signs.
These tests are important for catching lymphoma early. They also help see how well treatments are working. This way, doctors can catch any signs of the disease coming back.
Getting lymphoma right means understanding blood tests well. This knowledge helps both patients and doctors make better choices. It’s all about making sure treatments work well.
Thanks to blood tests, doctors can create better treatment plans. This leads to better health for patients. As science moves forward, blood tests will keep being a big help in fighting lymphoma.
FAQ
What blood tests are used to diagnose lymphoma?
To diagnose lymphoma, doctors use several blood tests. These include the Complete Blood Count (CBC), Lactate Dehydrogenase (LDH) test, and Erythrocyte Sedimentation Rate (ESR) test. Blood protein markers are also important. Tests like Flow Cytometry and Peripheral Blood Smear Analysis may be used too.
Can lymphoma be detected through a CBC test?
A CBC test can show signs of lymphoma. It might show an abnormal white blood cell count or low red and platelet counts. But, a CBC alone can’t confirm the diagnosis.
What is the role of LDH in lymphoma diagnosis?
LDH is an enzyme found in many body tissues. High LDH levels in the blood can mean tissue damage or lymphoma. It helps doctors diagnose and monitor lymphoma.
How does lymphoma affect white blood cell count?
Lymphoma can cause an abnormal increase in white blood cells. These cells are not normal and can be seen through blood tests.
Can anemia be a sign of lymphoma?
Yes, anemia can be a sign of lymphoma. It can happen because of cancer cells in the bone marrow, chronic disease, or poor nutrition.
What is the significance of platelet count abnormalities in lymphoma?
Low platelet count, or thrombocytopenia, can happen in lymphoma. It’s due to bone marrow involvement or other reasons. It’s important for diagnosis and treatment.
Are there specific blood markers for lymphoma?
There are no specific blood markers for lymphoma. But, tests like LDH, ESR, and blood protein markers can help support a diagnosis.
How is lymphoma diagnosed beyond blood work?
Beyond blood work, lymphoma diagnosis includes tests like lymph node biopsy and bone marrow biopsy. Imaging studies like CT or PET scans are also used.
Can lymphoma be missed if relying solely on blood tests?
Yes, relying only on blood tests can miss lymphoma. Some types may not show up in blood work. A full diagnostic approach is needed.
How are blood test results interpreted in the context of lymphoma?
Interpreting blood test results for lymphoma means looking at different abnormalities. This includes changes in white, red, and platelet counts. These findings are considered with other diagnostic results.
Can blood work be used to monitor lymphoma after diagnosis?
Yes, blood work is used to monitor lymphoma after diagnosis. It helps track treatment response, detect relapse, and manage long-term care.
Reference
National Cancer Institute (NCI) – Childhood Acute Lymphoblastic Leukemia Treatment:https://www.cancer.gov/types/leukemia/patient/child-all-treatment-pdq





