Recent statistics show that some cancers are hard to treat. This creates big medical oncology challenges. It’s tough for patients and doctors to find ways to fight these tumors.
Now, researchers are working hard to find new ways to treat cancer. They want to beat the current treatment limits. For those looking for top-notch medical care, we offer help and support.
Key Takeaways
- Cancer treatment limitations pose significant challenges for patients and healthcare providers.
- Certain types of cancer remain resistant to current treatments.
- Advancements in cancer treatment are being explored to overcome existing limitations.
- Comprehensive support services are available for international patients seeking advanced medical care.
- Understanding the complexities of incurable tumors is key to finding better treatments.
Understanding Tumor Curability
The idea of curability in oncology is complex. It depends on many factors. These factors affect how well a tumor can be treated and the patient’s chances of recovery.
Defining “Curable” in Oncology
In oncology, a tumor is curable if treatment can remove it completely. This means the patient can live a long time without cancer. The type and stage of cancer, along with the patient’s health, play a big role.
Getting an accurate diagnosis is key. Modern tests like imaging and molecular testing help us understand the tumor. This information guides how to treat it.
Factors That Determine Tumor Curability
Many things affect if a tumor can be cured. The type and stage of cancer, the biology of the tumor, and the patient’s health are important. For example, some cancers like certain leukemias are easier to cure. But others, like pancreatic cancer, are harder to treat because they are often found later.
- Tumor Type and Stage: Early-stage cancers are easier to cure than those found later.
- Molecular Characteristics: Certain genetic changes or biomarkers can change how well a tumor responds to treatment.
- Patient Health: A patient’s overall health, age, and other health issues affect their ability to get and respond to treatment.
The Spectrum of Prognosis
Prognosis varies a lot among different cancers and patients. Some patients get completely better, while others face a tougher road ahead. This can be due to treatment not working well or the cancer coming back.
Knowing the range of possible outcomes helps doctors tailor treatments. They aim to balance the chance of a cure with keeping the patient’s quality of life good. Thanks to ongoing research, treatments are getting better for more patients.
Characteristics of Incurable Tumors
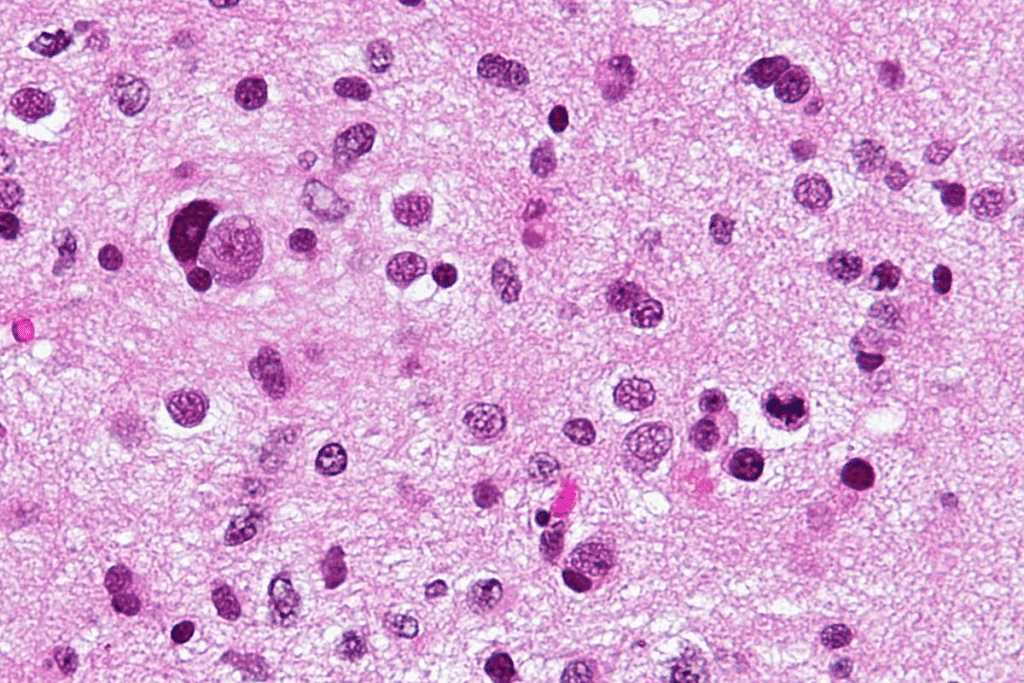
Incurable tumors have complex biology. They involve molecular, genetic, and anatomical factors. These factors make them hard to treat and aggressive.
Molecular and Genetic Factors
Genetic mutations and epigenetic modifications are key. They help cancer cells survive and resist treatment.
For example, TP53 gene mutations are common in cancer. They often lead to a poor prognosis. Knowing these changes helps in creating targeted treatments.
Anatomical Considerations
The location of a tumor affects its curability. Tumors in vital or hard-to-reach areas, like the brainstem or pancreas, are tough to treat.
Diffuse intrinsic pontine glioma (DIPG) is a brain tumor that can’t be surgically removed. Its location in the brainstem limits treatment options.
Metastatic Patterns
How a tumor spreads is also important. Tumors that spread early and far, like pancreatic ductal adenocarcinoma, have a worse prognosis.
Knowing how tumors spread helps in planning better treatments. This can improve patient outcomes.
Treatment Resistance Mechanisms
Treatment resistance is a big problem with incurable tumors. Many factors contribute to this, including genetic changes, the tumor environment, and cell diversity.
| Mechanism | Description | Impact on Treatment |
| Genetic Adaptations | Mutations that confer resistance to therapy | Reduces effectiveness of targeted therapies |
| Tumor Microenvironment | Factors such as hypoxia and immune suppression | Impairs delivery and efficacy of treatments |
| Cellular Heterogeneity | Diversity within the tumor cell population | Complicates treatment due to varied responses among subclones |
The Most Challenging Incurable Tumors in Clinical Practice
In oncology, we face tough incurable tumors. These are rare and aggressive, needing new treatments. They are hard to diagnose and treat because of their rarity and aggressive nature.
Rare and Aggressive Malignancies
Rare and aggressive tumors are hard to manage. They often have vague symptoms, making early detection tough. Their fast growth limits treatment options.
Some examples include:
- Angiosarcomas: Rare vascular tumors that can grow anywhere and are aggressive.
- Pleomorphic sarcomas: Rare, complex tumors with poor outcomes.
- Nasal and sinonasal malignancies: Rare, aggressive tumors often diagnosed late.
Treatment-Resistant Recurrent Tumors
Treatment-resistant tumors are another big challenge. These tumors keep coming back after many treatments, showing strong resistance.
Key traits of these tumors include:
- Genetic instability: High genetic instability makes them hard to treat.
- Tumor microenvironment changes: The environment around these tumors supports resistance.
- Epigenetic modifications: Changes that help them survive and resist treatment.
Understanding these traits is key to finding new ways to treat these tumors.
Pancreatic Ductal Adenocarcinoma
Pancreatic ductal adenocarcinoma is the main type of pancreatic cancer. It’s hard to diagnose and treat. We’ll look at why it’s tough, like its late detection and how it resists treatment. We’ll also talk about how doctors manage it today.
Late Detection Challenges
One big problem with pancreatic ductal adenocarcinoma is finding it early. Symptoms show up when it’s too late. This makes treatment less effective and affects patient outcomes.
Because early symptoms are rare, patients are often diagnosed too late. Looking for ways to detect it sooner is key to saving lives.
Desmoplastic Stroma Barriers
The desmoplastic stroma around the tumor makes treatment hard. It blocks drugs from reaching the tumor. Figuring out how to get past this stroma is important.
Resistance to Conventional Therapies
Pancreatic ductal adenocarcinoma doesn’t respond well to common treatments like chemo and radiation. Its genetic makeup makes it resistant. Researchers are working on new treatments that target these specific traits.
Current Management Approaches
Doctors are working hard to improve treatment for pancreatic ductal adenocarcinoma. They use a mix of surgery, chemo, and radiation. New treatments offer hope for better results.
Researchers are testing new ideas like immunotherapy and targeted therapy. They might help make treatments more effective.
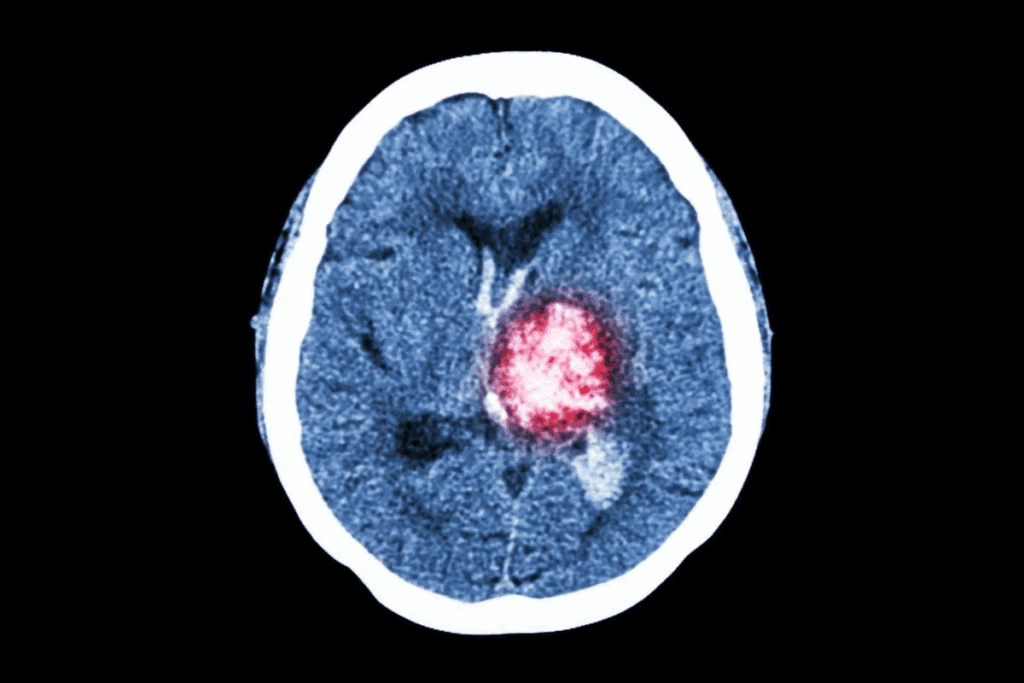
Diffuse Intrinsic Pontine Glioma (DIPG)
DIPG is a rare and aggressive brain tumor that mainly affects kids. It grows in the pons, a key part of the brainstem. This makes treating it very hard.
Challenges in Pediatric Brain Tumors
DIPG is a very tough brain tumor for kids, with a short survival time. It’s hard to treat because of its location, how fast it grows, and the age of the patients.
Because of its location in the brainstem, surgery is not an option. It would harm important brain areas. So, treatments mainly include radiation and chemotherapy.
Anatomical Barriers to Treatment
The brainstem, where DIPG grows, controls essential functions like breathing and heart rate. This makes treating it very tricky.
Doctors must find ways to target the tumor without harming the brain. But DIPG spreads, making it hard to know where to treat.
Molecular Characteristics
Recent studies have found what makes DIPG grow so fast. It’s due to specific genetic changes, like the H3K27M mutation.
Knowing this helps doctors create treatments that really work. They aim to attack the tumor’s root cause.
Current Research Directions
Researchers are working hard to find better ways to fight DIPG. They’re looking into treatments that target the tumor’s specific traits.
Immunotherapy is also being explored. It could help by focusing on tumor cells. Plus, there are ongoing trials to see if combining treatments can help more kids.
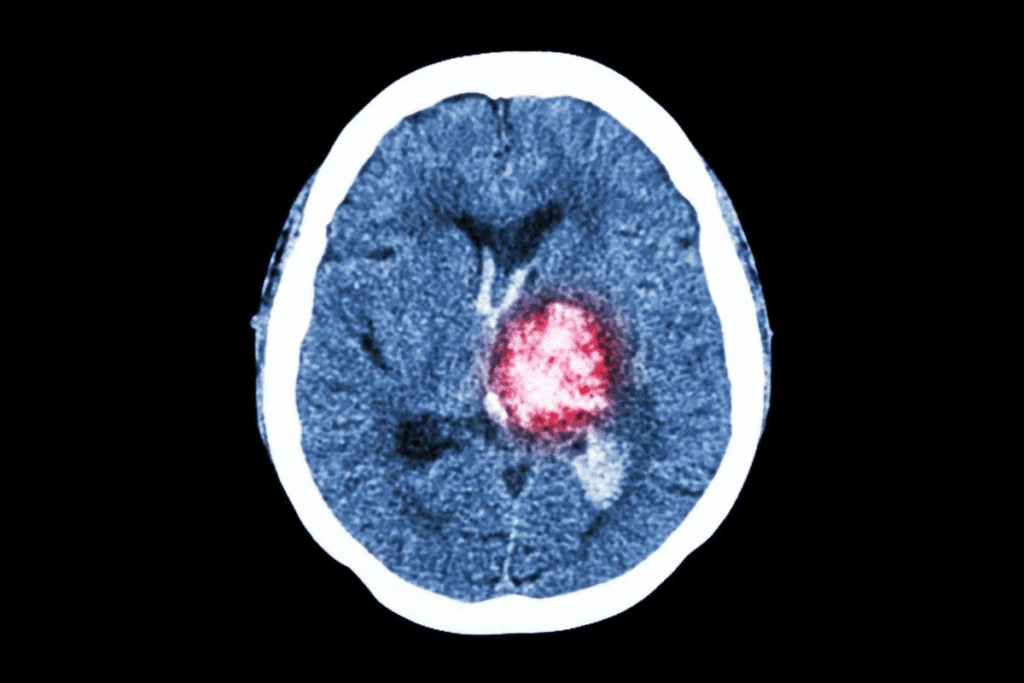
Metastatic Melanoma with Brain Involvement
Dealing with metastatic melanoma in the brain is a big challenge. When melanoma spreads to the brain, treatment gets harder. This often leads to a worse outlook for patients.
Blood-Brain Barrier Challenges
The blood-brain barrier (BBB) is a major hurdle in treating brain metastases. It keeps the brain safe but blocks many drugs. This makes it hard to fight brain metastases effectively.
Strategies to overcome the BBB include making drugs that can get past it. Also, using focused ultrasound to open the barrier for better drug delivery.
Treatment Limitations
Today’s treatments for melanoma in the brain are limited and can have harsh side effects. Surgical resection and stereotactic radiosurgery are used for a few brain tumors. But for many, these options are not enough.
For those with many brain tumors, systemic therapies are the main treatment. But, the BBB and other issues can limit their success.
Immunotherapy Responses
Immunotherapy has changed how we treat metastatic melanoma. It’s also being studied for brain metastases. Checkpoint inhibitors like PD-1 and CTLA-4 blockers show promise.
But, how well patients respond to immunotherapy varies. Some see long-lasting benefits, while others get less help.
Recent Advances and Remaining Hurdles
New research on melanoma brain metastases has led to new treatments. Targeted therapies and combination regimens are being tested to improve results.
Even with these new steps, big challenges remain. We need treatments that can get past the BBB. We also need to tackle the different types of melanoma brain metastases.
Triple-Negative Metastatic Breast Cancer
Triple-negative metastatic breast cancer is a tough challenge in cancer treatment. It grows fast and has few treatment options. This cancer type doesn’t have estrogen or progesterone receptors, and too much HER2 protein. So, it doesn’t respond well to hormone or HER2-targeted therapies.
Lack of Targeted Therapy Options
Managing triple-negative metastatic breast cancer is hard because of the lack of targeted therapy options. Unlike other breast cancers, there’s no specific target for treatment. So, doctors mainly use chemotherapy and other non-specific treatments.
Aggressive Biology and Progression
The aggressive biology of triple-negative metastatic breast cancer makes it grow fast and have a poor outlook. Patients often have bigger tumors and more lymph nodes involved at diagnosis. This highlights the need for early detection and effective treatments.
Chemotherapy Resistance
Chemotherapy is the main treatment for triple-negative metastatic breast cancer. But, chemotherapy resistance is a big problem. Many patients stop responding to different chemotherapy drugs. This means we need new ways to treat the disease.
Emerging Therapeutic Approaches
New treatments offer hope for triple-negative metastatic breast cancer. These include immunotherapy, PARP inhibitors for BRCA mutation patients, and new chemotherapy drugs. Researchers are working hard to find more effective treatments.
We’re making progress in treating triple-negative metastatic breast cancer. But, we need to keep researching to beat this aggressive disease.
Advanced Stage Small Cell Lung Cancer
Advanced stage small cell lung cancer is a big challenge in medicine. It grows fast and has few treatment options. This makes it hard for patients to get better.
Rapid Progression Patterns
This cancer type grows and spreads quickly. It often leads to early metastasis. This makes it hard to treat because the disease can get worse fast.
Factors contributing to rapid progression include:
- High proliferation rates of cancer cells
- Early vascular invasion
- Aggressive tumor biology
Limited Therapeutic Windows
The window for treating this cancer is small. It’s aggressive and quickly becomes resistant to treatments. There are few effective treatments, and they don’t last long.
Current treatment strategies include:
- Chemotherapy as the primary treatment modality
- Radiation therapy for palliation and symptom control
- Immunotherapy in selected cases
Immunotherapy Challenges
Immunotherapy is a promising treatment for many cancers, including small cell lung cancer. But, it’s hard to use in advanced stages. Finding the right biomarkers and dealing with resistance are big challenges.
Ongoing research aims to:
- Enhance the efficacy of immunotherapy
- Identify novel targets for intervention
- Develop combination regimens to overcome resistance
Management of Recurrent Disease
Dealing with recurrent advanced stage small cell lung cancer is tough. It often means the disease is getting worse. Palliative care is key to helping patients feel better.
Key considerations in managing recurrent disease include:
- Assessment of performance status and symptom burden
- Selection of appropriate second-line therapies
- Integration of palliative care services
Tumor Resistance Mechanisms
Understanding how tumors resist treatment is key to better cancer care. Tumors use many ways to avoid or fight off treatments. These methods are complex and involve different biological processes.
Genetic Adaptations and Mutations
Genetic changes are a big part of tumor resistance. Tumors can get mutations that make them less affected by treatments. For example, changes in the TP53 gene are common and can make tumors resistant to chemotherapy.
Tumors can become resistant through genetic changes like point mutations or gene amplification. These changes can turn on pathways that help tumors grow and survive, even when treated.
Tumor Microenvironment Factors
The environment around tumors also plays a big role in resistance. This environment includes different cell types like cancer-associated fibroblasts and immune cells. These cells can interact with tumor cells and affect their growth.
Tumor Microenvironment Components
| Component | Role in Tumor Resistance |
| Cancer-associated fibroblasts | Produce growth factors and cytokines that promote tumor growth and resistance |
| Immune cells | Can be immunosuppressive, creating an environment that protects the tumor |
| Endothelial cells | Form blood vessels that supply the tumor with nutrients and oxygen |
Cellular Heterogeneity
Tumors are made up of many different cell types. This diversity makes it hard to treat them effectively. Each cell type can respond differently to treatments.
Understanding and tackling this diversity is key to finding effective treatments. We need to target the different cell types in tumors.
Epigenetic Modifications
Epigenetic changes, like DNA methylation, also help tumors resist treatment. These changes can affect how genes are turned on or off without changing the DNA itself. This can influence how well tumor cells respond to therapy.
By studying how tumors resist treatment, we can find better ways to fight cancer. This includes looking at genetic changes, the tumor environment, cell diversity, and epigenetic modifications. This knowledge will help us improve cancer treatment outcomes.
Current Management Approaches for Incurable Tumors
Managing incurable tumors needs a mix of treatments. We look at all care options, from slowing tumor growth to improving life quality. This includes treatments that aim to change the disease and those that focus on comfort.
Disease-Modifying Treatments
Disease-modifying treatments try to slow tumor growth and extend life. These can be chemotherapy, targeted therapy, or immunotherapy. The right treatment depends on the tumor and the patient.
Targeted therapies have changed treatment for some incurable tumors. For example, BRAF inhibitors help in BRAF-mutated melanoma.
Palliative Interventions
Palliative care is key in managing symptoms and improving life quality. It includes pain management, nutrition support, and counseling. This care is for patients and their families.
Good palliative care needs a team of doctors, nurses, and specialists. They work together to meet the patient’s physical, emotional, and social needs. This way, we can greatly improve their life quality.
Quality of Life Considerations
Quality of life is very important when treating incurable tumors. We aim to extend life while keeping the patient comfortable and dignified.
Checking quality of life means looking at physical function, symptoms, and mental state. This helps us tailor care to each patient’s needs.
Novel Therapeutic Strategies
New treatments are being tested to help patients with incurable tumors. These include new immunotherapies and treatments that target several tumor growth pathways.
Joining clinical trials gives patients access to these new treatments. It also helps us improve cancer care. We’re committed to providing the best care for those with incurable tumors.
Promising Research and Future Directions
The field of oncology is on the verge of a big change. New research and directions offer hope for those with tough tumors. We’re learning more about cancer biology, leading to new ways to treat it.
Immunotherapy Innovations
Immunotherapy has changed cancer treatment a lot. CAR-T cell therapy is showing great promise in blood cancers. Researchers are working on making CAR-T cells more precise and exploring its use in solid tumors.
Checkpoint inhibitors have also made a big impact. They help the immune system fight cancer better. Trials are looking at combining these treatments and finding new targets to improve results.
Targeted Molecular Approaches
Targeted therapies have been a big step forward. They target specific changes in tumors. Precision medicine is becoming key, leading to more tailored treatments.
New tyrosine kinase inhibitors and PARP inhibitors are being developed. The challenge is to find the best targets and overcome resistance.
Combination Therapy Strategies
Using different treatments together is showing promise. Researchers are looking at combining immunotherapy with other therapies. This could lead to better results and make some tumors treatable.
Trials are testing the best ways to use these combinations. The aim is to get the most benefit while reducing side effects.
Early Detection Technologies
Early detection is key to better cancer outcomes. Liquid biopsy and imaging technologies are helping catch tumors early. These tools can spot cancers when they’re easier to treat and track how well treatments are working.
The next steps are to make these tests even better. The goal is to find cancers before symptoms show up, which could greatly improve survival rates.
Living with an Incurable Tumor Diagnosis
Dealing with an incurable tumor is more than just medical treatment. It needs a full support system. Patients and their families face physical, emotional, and psychological challenges.
Psychological Support Systems
Psychological support is key for those with incurable tumors. It includes counseling, support groups, and therapy. These help manage the emotional struggles that come with a serious diagnosis.
Support groups offer a community where patients can share and find comfort. Professional counseling helps manage anxiety, depression, and other mental health issues.
Palliative Care Integration
Palliative care is essential for managing incurable tumors. It aims to ease symptoms and stress, improving life quality for patients and families.
Palliative care teams help manage pain, symptoms, and offer emotional and spiritual support. This care is not just for end-of-life situations but can be given alongside other treatments.
Patient Advocacy and Resources
Patient advocacy is vital in navigating the healthcare system. Advocates help access resources, understand treatment options, and communicate with healthcare providers.
Many organizations provide resources for those with incurable tumors. These include educational materials, financial help, and support services. These can greatly help patients manage their condition.
Clinical Trial Participation
Clinical trials offer new treatments not available elsewhere. They can give hope and potentially better outcomes for patients with incurable tumors.
It’s important for patients to talk to their healthcare providers about clinical trials. This helps determine if they’re right for their situation.
| Support System | Description | Benefits |
| Psychological Support | Counseling, therapy, support groups | Coping strategies, emotional relief |
| Palliative Care | Symptom management, stress relief | Improved quality of life |
| Patient Advocacy | Navigation of healthcare system, resource access | Better healthcare outcomes, support |
| Clinical Trials | Access to new treatments | Potential improvement in condition, hope |
Conclusion
We’ve looked into the tough issues with tumor curability and the biggest challenges in treating them. Knowing what makes a tumor curable is key to tackling these hard-to-treat cancers.
Tumors like pancreatic cancer and brain tumors are very hard to cure. They don’t respond well to common treatments because of their biology and where they are in the body. But, new research and ideas in cancer care give us hope for better ways to manage these diseases.
As we face the hurdles of cancer treatment, we must value palliative care, patient support, and joining clinical trials. By teaming up to tackle these tough cases, we aim to provide top-notch care and support for those affected.
FAQ
What makes a tumor incurable?
A tumor is incurable if it can’t be fully removed or treated with today’s medicine. This is often because of its location, size, or spread to other parts of the body.
What are the most challenging incurable tumors?
Some of the toughest incurable tumors include pancreatic cancer, brain cancer in kids, and aggressive melanoma. Also, advanced breast cancer and lung cancer are very hard to treat.
What are the molecular and genetic factors that contribute to tumor incurability?
Genetic changes, epigenetic changes, and the tumor’s environment play big roles. These factors help tumors resist treatment and become incurable.
How do anatomical considerations affect tumor curability?
The tumor’s location and how close it is to important parts of the body matter a lot. This affects if surgery can work and how well other treatments will do.
What are the challenges associated with treating metastatic tumors?
Metastatic tumors are hard to treat because cancer cells spread to many places. This makes it tough to hit all the cancer cells with treatment.
What is the role of treatment resistance mechanisms in tumor incurability?
Treatment resistance comes from genetic changes, the tumor’s environment, and different types of cells. These factors make treatments less effective and tumors incurable.
What are the current management approaches for incurable tumors?
For incurable tumors, treatments aim to slow the disease and improve life quality. New treatments are being tested in clinical trials.
What are the promising research directions for incurable tumors?
New research focuses on immunotherapy, targeted treatments, and combining therapies. Early detection is also a key area of study.
How can patients with incurable tumors access psychological support and palliative care?
Patients can get support and care through their doctors. Doctors can help find resources and services to enhance life quality.
What is the importance of patient advocacy and clinical trial participation for patients with incurable tumors?
Being an advocate and joining clinical trials is vital. It offers new treatments and support to navigate the healthcare system.
How can patients with difficult to treat cancers, such as rare and aggressive tumors, find appropriate treatment options?
Patients should talk to their doctors and look into specialized cancer centers. Clinical trials for their cancer type are also worth exploring.
What are the challenges associated with advanced stage malignancies, and how can they be addressed?
Advanced cancers have few treatment options and a poor outlook. A team approach, including palliative care, is needed. Innovative treatments are also key.
How do tumor genetic variations impact treatment outcomes, and what are the implications for cancer therapy?
Genetic changes in tumors can affect how well treatments work. Understanding these changes is essential for creating personalized treatments and improving cancer care.
Reference
- Pillai, R. K., et al. (2017). Rare cancers: Challenges and issues. PMC, National Center for Biotechnology Information. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5460568/
Recent statistics show that some cancers are hard to treat. This creates big medical oncology challenges. It’s tough for patients and doctors to find ways to fight these tumors.
Now, researchers are working hard to find new ways to treat cancer. They want to beat the current treatment limits. For those looking for top-notch medical care, we offer help and support.
Key Takeaways
- Cancer treatment limitations pose significant challenges for patients and healthcare providers.
- Certain types of cancer remain resistant to current treatments.
- Advancements in cancer treatment are being explored to overcome existing limitations.
- Comprehensive support services are available for international patients seeking advanced medical care.
- Understanding the complexities of incurable tumors is key to finding better treatments.
Understanding Tumor Curability
The idea of curability in oncology is complex. It depends on many factors. These factors affect how well a tumor can be treated and the patient’s chances of recovery.
Defining “Curable” in Oncology
In oncology, a tumor is curable if treatment can remove it completely. This means the patient can live a long time without cancer. The type and stage of cancer, along with the patient’s health, play a big role.
Getting an accurate diagnosis is key. Modern tests like imaging and molecular testing help us understand the tumor. This information guides how to treat it.
Factors That Determine Tumor Curability
Many things affect if a tumor can be cured. The type and stage of cancer, the biology of the tumor, and the patient’s health are important. For example, some cancers like certain leukemias are easier to cure. But others, like pancreatic cancer, are harder to treat because they are often found later.
- Tumor Type and Stage: Early-stage cancers are easier to cure than those found later.
- Molecular Characteristics: Certain genetic changes or biomarkers can change how well a tumor responds to treatment.
- Patient Health: A patient’s overall health, age, and other health issues affect their ability to get and respond to treatment.
The Spectrum of Prognosis
Prognosis varies a lot among different cancers and patients. Some patients get completely better, while others face a tougher road ahead. This can be due to treatment not working well or the cancer coming back.
Knowing the range of possible outcomes helps doctors tailor treatments. They aim to balance the chance of a cure with keeping the patient’s quality of life good. Thanks to ongoing research, treatments are getting better for more patients.
Characteristics of Incurable Tumors
Incurable tumors have complex biology. They involve molecular, genetic, and anatomical factors. These factors make them hard to treat and aggressive.
Molecular and Genetic Factors
Genetic mutations and epigenetic modifications are key. They help cancer cells survive and resist treatment.
For example, TP53 gene mutations are common in cancer. They often lead to a poor prognosis. Knowing these changes helps in creating targeted treatments.
Anatomical Considerations
The location of a tumor affects its curability. Tumors in vital or hard-to-reach areas, like the brainstem or pancreas, are tough to treat.
Diffuse intrinsic pontine glioma (DIPG) is a brain tumor that can’t be surgically removed. Its location in the brainstem limits treatment options.
Metastatic Patterns
How a tumor spreads is also important. Tumors that spread early and far, like pancreatic ductal adenocarcinoma, have a worse prognosis.
Knowing how tumors spread helps in planning better treatments. This can improve patient outcomes.
Treatment Resistance Mechanisms
Treatment resistance is a big problem with incurable tumors. Many factors contribute to this, including genetic changes, the tumor environment, and cell diversity.
| Mechanism | Description | Impact on Treatment |
| Genetic Adaptations | Mutations that confer resistance to therapy | Reduces effectiveness of targeted therapies |
| Tumor Microenvironment | Factors such as hypoxia and immune suppression | Impairs delivery and efficacy of treatments |
| Cellular Heterogeneity | Diversity within the tumor cell population | Complicates treatment due to varied responses among subclones |
The Most Challenging Incurable Tumors in Clinical Practice
In oncology, we face tough incurable tumors. These are rare and aggressive, needing new treatments. They are hard to diagnose and treat because of their rarity and aggressive nature.
Rare and Aggressive Malignancies
Rare and aggressive tumors are hard to manage. They often have vague symptoms, making early detection tough. Their fast growth limits treatment options.
Some examples include:
- Angiosarcomas: Rare vascular tumors that can grow anywhere and are aggressive.
- Pleomorphic sarcomas: Rare, complex tumors with poor outcomes.
- Nasal and sinonasal malignancies: Rare, aggressive tumors often diagnosed late.
Treatment-Resistant Recurrent Tumors
Treatment-resistant tumors are another big challenge. These tumors keep coming back after many treatments, showing strong resistance.
Key traits of these tumors include:
- Genetic instability: High genetic instability makes them hard to treat.
- Tumor microenvironment changes: The environment around these tumors supports resistance.
- Epigenetic modifications: Changes that help them survive and resist treatment.
Understanding these traits is key to finding new ways to treat these tumors.
Pancreatic Ductal Adenocarcinoma
Pancreatic ductal adenocarcinoma is the main type of pancreatic cancer. It’s hard to diagnose and treat. We’ll look at why it’s tough, like its late detection and how it resists treatment. We’ll also talk about how doctors manage it today.
Late Detection Challenges
One big problem with pancreatic ductal adenocarcinoma is finding it early. Symptoms show up when it’s too late. This makes treatment less effective and affects patient outcomes.
Because early symptoms are rare, patients are often diagnosed too late. Looking for ways to detect it sooner is key to saving lives.
Desmoplastic Stroma Barriers
The desmoplastic stroma around the tumor makes treatment hard. It blocks drugs from reaching the tumor. Figuring out how to get past this stroma is important.
Resistance to Conventional Therapies
Pancreatic ductal adenocarcinoma doesn’t respond well to common treatments like chemo and radiation. Its genetic makeup makes it resistant. Researchers are working on new treatments that target these specific traits.
Current Management Approaches
Doctors are working hard to improve treatment for pancreatic ductal adenocarcinoma. They use a mix of surgery, chemo, and radiation. New treatments offer hope for better results.
Researchers are testing new ideas like immunotherapy and targeted therapy. They might help make treatments more effective.
Diffuse Intrinsic Pontine Glioma (DIPG)
DIPG is a rare and aggressive brain tumor that mainly affects kids. It grows in the pons, a key part of the brainstem. This makes treating it very hard.
Challenges in Pediatric Brain Tumors
DIPG is a very tough brain tumor for kids, with a short survival time. It’s hard to treat because of its location, how fast it grows, and the age of the patients.
Because of its location in the brainstem, surgery is not an option. It would harm important brain areas. So, treatments mainly include radiation and chemotherapy.
Anatomical Barriers to Treatment
The brainstem, where DIPG grows, controls essential functions like breathing and heart rate. This makes treating it very tricky.
Doctors must find ways to target the tumor without harming the brain. But DIPG spreads, making it hard to know where to treat.
Molecular Characteristics
Recent studies have found what makes DIPG grow so fast. It’s due to specific genetic changes, like the H3K27M mutation.
Knowing this helps doctors create treatments that really work. They aim to attack the tumor’s root cause.
Current Research Directions
Researchers are working hard to find better ways to fight DIPG. They’re looking into treatments that target the tumor’s specific traits.
Immunotherapy is also being explored. It could help by focusing on tumor cells. Plus, there are ongoing trials to see if combining treatments can help more kids.
Metastatic Melanoma with Brain Involvement
Dealing with metastatic melanoma in the brain is a big challenge. When melanoma spreads to the brain, treatment gets harder. This often leads to a worse outlook for patients.
Blood-Brain Barrier Challenges
The blood-brain barrier (BBB) is a major hurdle in treating brain metastases. It keeps the brain safe but blocks many drugs. This makes it hard to fight brain metastases effectively.
Strategies to overcome the BBB include making drugs that can get past it. Also, using focused ultrasound to open the barrier for better drug delivery.
Treatment Limitations
Today’s treatments for melanoma in the brain are limited and can have harsh side effects. Surgical resection and stereotactic radiosurgery are used for a few brain tumors. But for many, these options are not enough.
For those with many brain tumors, systemic therapies are the main treatment. But, the BBB and other issues can limit their success.
Immunotherapy Responses
Immunotherapy has changed how we treat metastatic melanoma. It’s also being studied for brain metastases. Checkpoint inhibitors like PD-1 and CTLA-4 blockers show promise.
But, how well patients respond to immunotherapy varies. Some see long-lasting benefits, while others get less help.
Recent Advances and Remaining Hurdles
New research on melanoma brain metastases has led to new treatments. Targeted therapies and combination regimens are being tested to improve results.
Even with these new steps, big challenges remain. We need treatments that can get past the BBB. We also need to tackle the different types of melanoma brain metastases.
Triple-Negative Metastatic Breast Cancer
Triple-negative metastatic breast cancer is a tough challenge in cancer treatment. It grows fast and has few treatment options. This cancer type doesn’t have estrogen or progesterone receptors, and too much HER2 protein. So, it doesn’t respond well to hormone or HER2-targeted therapies.
Lack of Targeted Therapy Options
Managing triple-negative metastatic breast cancer is hard because of the lack of targeted therapy options. Unlike other breast cancers, there’s no specific target for treatment. So, doctors mainly use chemotherapy and other non-specific treatments.
Aggressive Biology and Progression
The aggressive biology of triple-negative metastatic breast cancer makes it grow fast and have a poor outlook. Patients often have bigger tumors and more lymph nodes involved at diagnosis. This highlights the need for early detection and effective treatments.
Chemotherapy Resistance
Chemotherapy is the main treatment for triple-negative metastatic breast cancer. But, chemotherapy resistance is a big problem. Many patients stop responding to different chemotherapy drugs. This means we need new ways to treat the disease.
Emerging Therapeutic Approaches
New treatments offer hope for triple-negative metastatic breast cancer. These include immunotherapy, PARP inhibitors for BRCA mutation patients, and new chemotherapy drugs. Researchers are working hard to find more effective treatments.
We’re making progress in treating triple-negative metastatic breast cancer. But, we need to keep researching to beat this aggressive disease.
Advanced Stage Small Cell Lung Cancer
Advanced stage small cell lung cancer is a big challenge in medicine. It grows fast and has few treatment options. This makes it hard for patients to get better.
Rapid Progression Patterns
This cancer type grows and spreads quickly. It often leads to early metastasis. This makes it hard to treat because the disease can get worse fast.
Factors contributing to rapid progression include:
- High proliferation rates of cancer cells
- Early vascular invasion
- Aggressive tumor biology
Limited Therapeutic Windows
The window for treating this cancer is small. It’s aggressive and quickly becomes resistant to treatments. There are few effective treatments, and they don’t last long.
Current treatment strategies include:
- Chemotherapy as the primary treatment modality
- Radiation therapy for palliation and symptom control
- Immunotherapy in selected cases
Immunotherapy Challenges
Immunotherapy is a promising treatment for many cancers, including small cell lung cancer. But, it’s hard to use in advanced stages. Finding the right biomarkers and dealing with resistance are big challenges.
Ongoing research aims to:
- Enhance the efficacy of immunotherapy
- Identify novel targets for intervention
- Develop combination regimens to overcome resistance
Management of Recurrent Disease
Dealing with recurrent advanced stage small cell lung cancer is tough. It often means the disease is getting worse. Palliative care is key to helping patients feel better.
Key considerations in managing recurrent disease include:
- Assessment of performance status and symptom burden
- Selection of appropriate second-line therapies
- Integration of palliative care services
Tumor Resistance Mechanisms
Understanding how tumors resist treatment is key to better cancer care. Tumors use many ways to avoid or fight off treatments. These methods are complex and involve different biological processes.
Genetic Adaptations and Mutations
Genetic changes are a big part of tumor resistance. Tumors can get mutations that make them less affected by treatments. For example, changes in the TP53 gene are common and can make tumors resistant to chemotherapy.
Tumors can become resistant through genetic changes like point mutations or gene amplification. These changes can turn on pathways that help tumors grow and survive, even when treated.
Tumor Microenvironment Factors
The environment around tumors also plays a big role in resistance. This environment includes different cell types like cancer-associated fibroblasts and immune cells. These cells can interact with tumor cells and affect their growth.
Tumor Microenvironment Components
| Component | Role in Tumor Resistance |
| Cancer-associated fibroblasts | Produce growth factors and cytokines that promote tumor growth and resistance |
| Immune cells | Can be immunosuppressive, creating an environment that protects the tumor |
| Endothelial cells | Form blood vessels that supply the tumor with nutrients and oxygen |
Cellular Heterogeneity
Tumors are made up of many different cell types. This diversity makes it hard to treat them effectively. Each cell type can respond differently to treatments.
Understanding and tackling this diversity is key to finding effective treatments. We need to target the different cell types in tumors.
Epigenetic Modifications
Epigenetic changes, like DNA methylation, also help tumors resist treatment. These changes can affect how genes are turned on or off without changing the DNA itself. This can influence how well tumor cells respond to therapy.
By studying how tumors resist treatment, we can find better ways to fight cancer. This includes looking at genetic changes, the tumor environment, cell diversity, and epigenetic modifications. This knowledge will help us improve cancer treatment outcomes.
Current Management Approaches for Incurable Tumors
Managing incurable tumors needs a mix of treatments. We look at all care options, from slowing tumor growth to improving life quality. This includes treatments that aim to change the disease and those that focus on comfort.
Disease-Modifying Treatments
Disease-modifying treatments try to slow tumor growth and extend life. These can be chemotherapy, targeted therapy, or immunotherapy. The right treatment depends on the tumor and the patient.
Targeted therapies have changed treatment for some incurable tumors. For example, BRAF inhibitors help in BRAF-mutated melanoma.
Palliative Interventions
Palliative care is key in managing symptoms and improving life quality. It includes pain management, nutrition support, and counseling. This care is for patients and their families.
Good palliative care needs a team of doctors, nurses, and specialists. They work together to meet the patient’s physical, emotional, and social needs. This way, we can greatly improve their life quality.
Quality of Life Considerations
Quality of life is very important when treating incurable tumors. We aim to extend life while keeping the patient comfortable and dignified.
Checking quality of life means looking at physical function, symptoms, and mental state. This helps us tailor care to each patient’s needs.
Novel Therapeutic Strategies
New treatments are being tested to help patients with incurable tumors. These include new immunotherapies and treatments that target several tumor growth pathways.
Joining clinical trials gives patients access to these new treatments. It also helps us improve cancer care. We’re committed to providing the best care for those with incurable tumors.
Promising Research and Future Directions
The field of oncology is on the verge of a big change. New research and directions offer hope for those with tough tumors. We’re learning more about cancer biology, leading to new ways to treat it.
Immunotherapy Innovations
Immunotherapy has changed cancer treatment a lot. CAR-T cell therapy is showing great promise in blood cancers. Researchers are working on making CAR-T cells more precise and exploring its use in solid tumors.
Checkpoint inhibitors have also made a big impact. They help the immune system fight cancer better. Trials are looking at combining these treatments and finding new targets to improve results.
Targeted Molecular Approaches
Targeted therapies have been a big step forward. They target specific changes in tumors. Precision medicine is becoming key, leading to more tailored treatments.
New tyrosine kinase inhibitors and PARP inhibitors are being developed. The challenge is to find the best targets and overcome resistance.
Combination Therapy Strategies
Using different treatments together is showing promise. Researchers are looking at combining immunotherapy with other therapies. This could lead to better results and make some tumors treatable.
Trials are testing the best ways to use these combinations. The aim is to get the most benefit while reducing side effects.
Early Detection Technologies
Early detection is key to better cancer outcomes. Liquid biopsy and imaging technologies are helping catch tumors early. These tools can spot cancers when they’re easier to treat and track how well treatments are working.
The next steps are to make these tests even better. The goal is to find cancers before symptoms show up, which could greatly improve survival rates.
Living with an Incurable Tumor Diagnosis
Dealing with an incurable tumor is more than just medical treatment. It needs a full support system. Patients and their families face physical, emotional, and psychological challenges.
Psychological Support Systems
Psychological support is key for those with incurable tumors. It includes counseling, support groups, and therapy. These help manage the emotional struggles that come with a serious diagnosis.
Support groups offer a community where patients can share and find comfort. Professional counseling helps manage anxiety, depression, and other mental health issues.
Palliative Care Integration
Palliative care is essential for managing incurable tumors. It aims to ease symptoms and stress, improving life quality for patients and families.
Palliative care teams help manage pain, symptoms, and offer emotional and spiritual support. This care is not just for end-of-life situations but can be given alongside other treatments.
Patient Advocacy and Resources
Patient advocacy is vital in navigating the healthcare system. Advocates help access resources, understand treatment options, and communicate with healthcare providers.
Many organizations provide resources for those with incurable tumors. These include educational materials, financial help, and support services. These can greatly help patients manage their condition.
Clinical Trial Participation
Clinical trials offer new treatments not available elsewhere. They can give hope and potentially better outcomes for patients with incurable tumors.
It’s important for patients to talk to their healthcare providers about clinical trials. This helps determine if they’re right for their situation.
| Support System | Description | Benefits |
| Psychological Support | Counseling, therapy, support groups | Coping strategies, emotional relief |
| Palliative Care | Symptom management, stress relief | Improved quality of life |
| Patient Advocacy | Navigation of healthcare system, resource access | Better healthcare outcomes, support |
| Clinical Trials | Access to new treatments | Potential improvement in condition, hope |
Conclusion
We’ve looked into the tough issues with tumor curability and the biggest challenges in treating them. Knowing what makes a tumor curable is key to tackling these hard-to-treat cancers.
Tumors like pancreatic cancer and brain tumors are very hard to cure. They don’t respond well to common treatments because of their biology and where they are in the body. But, new research and ideas in cancer care give us hope for better ways to manage these diseases.
As we face the hurdles of cancer treatment, we must value palliative care, patient support, and joining clinical trials. By teaming up to tackle these tough cases, we aim to provide top-notch care and support for those affected.
FAQ
What makes a tumor incurable?
A tumor is incurable if it can’t be fully removed or treated with today’s medicine. This is often because of its location, size, or spread to other parts of the body.
What are the most challenging incurable tumors?
Some of the toughest incurable tumors include pancreatic cancer, brain cancer in kids, and aggressive melanoma. Also, advanced breast cancer and lung cancer are very hard to treat.
What are the molecular and genetic factors that contribute to tumor incurability?
Genetic changes, epigenetic changes, and the tumor’s environment play big roles. These factors help tumors resist treatment and become incurable.
How do anatomical considerations affect tumor curability?
The tumor’s location and how close it is to important parts of the body matter a lot. This affects if surgery can work and how well other treatments will do.
What are the challenges associated with treating metastatic tumors?
Metastatic tumors are hard to treat because cancer cells spread to many places. This makes it tough to hit all the cancer cells with treatment.
What is the role of treatment resistance mechanisms in tumor incurability?
Treatment resistance comes from genetic changes, the tumor’s environment, and different types of cells. These factors make treatments less effective and tumors incurable.
What are the current management approaches for incurable tumors?
For incurable tumors, treatments aim to slow the disease and improve life quality. New treatments are being tested in clinical trials.
What are the promising research directions for incurable tumors?
New research focuses on immunotherapy, targeted treatments, and combining therapies. Early detection is also a key area of study.
How can patients with incurable tumors access psychological support and palliative care?
Patients can get support and care through their doctors. Doctors can help find resources and services to enhance life quality.
What is the importance of patient advocacy and clinical trial participation for patients with incurable tumors?
Being an advocate and joining clinical trials is vital. It offers new treatments and support to navigate the healthcare system.
How can patients with difficult to treat cancers, such as rare and aggressive tumors, find appropriate treatment options?
Patients should talk to their doctors and look into specialized cancer centers. Clinical trials for their cancer type are also worth exploring.
What are the challenges associated with advanced stage malignancies, and how can they be addressed?
Advanced cancers have few treatment options and a poor outlook. A team approach, including palliative care, is needed. Innovative treatments are also key.
How do tumor genetic variations impact treatment outcomes, and what are the implications for cancer therapy?
Genetic changes in tumors can affect how well treatments work. Understanding these changes is essential for creating personalized treatments and improving cancer care.
Reference
- Pillai, R. K., et al. (2017). Rare cancers: Challenges and issues. PMC, National Center for Biotechnology Information. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5460568/






















